Abstract
Purpose
We investigated the effect of a chondrocyte-derived extracellular matrix (CDECM) on experimental corneal alkaline burns in rabbits.
Methods
Corneal neovascularization (NV) was induced by applying an 8-mm filter paper soaked in 1 N NaOH to the right central corneas of rabbits for 1 minute. Ten days later, the rabbits were randomly divided into three groups: the alkaline burn group, the CDECM transplantation group, and the human amniotic membrane (HAM) transplantation group. The left eyes were used as controls. CDECM and HAM were transplanted onto the corneal surface to completely cover the resected area and were subsequently sutured. On the 10th day after transplantation, the structural changes of the cornea were analyzed histologically. We examined the effects of CDECM on clinical NV features and on the expression of corneal NV markers.
Results
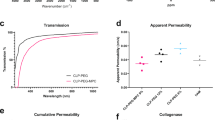
The alkaline burn produced significant NV and increased the corneal thickness. On day 10 after transplantation, the thickness, NV and opacity of the cornea were markedly decreased in the CDECM group (p < 0.001). However, the HAM transplantation group did not exhibit improvements in these clinical parameters, and there were no significant differences relative to the burn group. In addition, the use of CDECM improved the healing of the cornea following the alkaline burn by disrupting the corneal epithelial proliferation and reducing the fibrotic changes of the stroma. The hallmarks of NV were significantly induced in the subepithelium by the alkaline burn, and these levels were also suppressed by CDECM. The CDECM suppressed corneal NV by inhibiting nuclear factor-kappa B (NF-κB) activation by blocking the PKC and Akt signaling pathways.
Conclusions
CDECM transplantation was markedly effective in healing alkali-burned corneas by modulating the translocation of NF-κB to the nucleus, thereby representing a promising material for the noninvasive treatment of ocular surface disease.







Similar content being viewed by others
References
Liesegang TJ (1989) Epidemiology of ocular herpes simplex. Natural history in Rochester, Minn, 1950 through 1982. Arch Ophthalmol 107:1160–1165
Resnikoff S, Pascolini D, Etya’ale D, Kocur I, Pararajasegaram R, Pokharel GP, Mariotti SP (2004) Global data on visual impairment in the year 2002. Bull World Health Organ 82:844–851
Lee P, Wang CC, Adamis AP (1998) Ocular neovascularizaion: An epidemiologic review. Surv Ophthalmol 43:245–269
Clements JL, Dana R (2011) Inflammatory corneal neovascularization: Etiopathogenesis. Semin Ophthalmol 26:235–245
Yoon KC, Ahn KY, Lee JH, Chun BJ, Park SW, Seo MS, Park YG, Kim KK (2005) Lipid-mediated delivery of brain-specific angiogenesis inhibitor 1 gene reduces corneal neovascularization in an in vivo rabbit model. Gene Ther 12:617–624
Chang JH, Gabison EE, Kato T, Azar DT (2001) Corneal neovascularization. Curr Opin Ophthalmol 12:242–249
Ge H, Xia N, Yin X, Fu S, Ge J, Shi Y, Liu P (2011) Comparison of the antiangiogenic activity of modified RGDRGD-endostatin to endostatin delivered by gene transfer in vivo rabbit neovascularization model. Mol Vis 17:1918–1928
Maddula S, Davis DK, Maddula S, Burrow MK, Ambati BK (2011) Horizons in therapy for corneal angiogensis. Am J Ophthalmol 118:591–599
Montexuma SR, Vavvas D, Miller JM (2009) Review of the ocular angiogenesis animal models. Semin Ophthamol 24:52–56
Jang IK, Ahn JI, Shin JS, Kwon YS, Ryu YH, Lee JK, Park JK, Song KY, Yang EK, Kim JC (2006) Transplantation of reconstructed corneal layer composed of corneal epithelium and fibroblasts on a lyophilized amniotic membrane to severely alkali-burned cornea. Artif Organs 30:424–431
Shahriari HA, Tokhmehchi F, Reza M, Hashemi NF (2008) Comparison of the effect of amniotic membrane suspension and autologous serum on alkaline corneal epithelial wound healing in the rabbit model. Cornea 27(10):1148–1150
Kim JS, Kim JC, Na BK, Jeong JM, Song CY (2000) Amniotic membrane patching promotes healing and inhibits proteinase activity on wound healing following acute corneal alkali burn. Exp Eye Res 70:329–337
Domarus DV, Nauman GOH (1986) Accidental and surgical trauma and wound healing of the eye. Pathology of the eye. Springer-Verlag, New York
Bouchard CS, John T (2004) Amniotic membrane transplantation in the management of severe ocular surface disease: indications and outcomes. Ocul Surf 2:201–211
Kheirkhah A, Johnson DA, Paranjpe DR, Raju VK, Casas V, Tseng SC (2008) Temporary sutureless amniotic membrane patch for acute alkaline burns. Arch Ophthalmol 126:1059–1066
Clare G, Suleman H, Bunce D, Dua H (2012) Amniotic membrane transplantation for acute ocular burns. Cochrane Database Syst Rev. doi:10.1002/14651858, CD009379.pub2
Yang LL, Zhou QJ, Gao Y, Wang YO (2012) Comparison of the therapeutic effects of extracts from Spirulina platensis and amniotic membrane on inflammation-associated corneal neovascularization. Int J Ophthalmol 5:32–37
Schmidt CE, Baier JM (2000) Acellular vascular tissues: natural biomaterials for tissue repair and tissue engineering. Biomaterials 21:2215–2231
Kopp BP, Rippy MK, Badylak SF, Adams MC, Keating MA, Rink RC, Thor KB (1996) Regenerative urinary bladder augmentation using small intestinal submucosa: urodynamic and histopathologic assessment in long-term canine bladder augmentations. J Urol 155:2098–2104
Badylak SF, Tullius R, Kokini K, Shelbourne KD, Klootwyk T, Voytik SL, Kraine MR, Simmons C (1995) The use of xenogeneic small intestinal submucosa as a biomaterial for Achilles tendon repair in a dog model. J Biomed Mater Res 29:977–985
Piechota HJ, Dahms SF, Probst M, Gleason CA, Nunes LS, Dahiya R, Lue TF, Tanagho EA (1998) Functional rat bladder regeneration though xenotransplantation of the bladder acellular matrix graft. Br J Urol 81:548–559
Lee SH, Tseng SCG (1997) Amniotic membrane transplantation for persistent epithelial defects with ulceration. Am J Ophthalmol 123:303–312
Jin CZ, Park SR, Choi BH, Park KD, Min BH (2007) In vivo cartilage tissue engineering using a cell-derived extracellular matrix (ECM) scaffold. Artif Organs 31:183–189
Choi KH, Song BR, Choi BH, Lee MH, Park SR, Min BH (2012) Cartilage tissue engineering using chondrocyte-derived extracellular matrix scaffold suppressed vessel invasion during chondrogenesis of mesenchymal stem cells in vivo. Tissue Eng 9:43–50
Lee HS, Lee JH, Yang JW (2014) Effect of porcine chondrocyte-derived extracellular matrix on the pterygium in mouse model. Graefes Arch Clin Exp Ophthalmol 252:609-618. doi:10.1007/s00417-014-2592-8
Yang JW, Heo MS, Lee CH, Moon SW, Min BH, Choi BH, Kang MS, Moon SH (2014) The effect of the cell-derived extracellular matrix membrane on wound adhesions in rabbit strabismus surgery. J Tissue Eng Regen Med 11:1–8
Choi KH, Choi BH, Park SR, Kim BJ, Min BH (2010) The chondrogenic differentiation of mesenchymal stem cells on an extracellular matrix scaffold derived from porcine chondrocytes. Biomaterials 31:5355–5365
Chie S, Leonard PK, Noriko K, Higashihara H, Ueta M, Inatomi T, Yokoi N, Kaido M, Dogru M, Shimazaki J, Tsubota K, Yamada M, Kinoshita S (2007) New grading system for the evaluation of chronic ocular manifestations in patients with Stevens–Johnson syndrome. Ophthamology 114:1294–1302
Rao K, Farley WJ, Pflugfelder SC (2010) Association between high tear epidermal growth factor levels and corneal subepithelial fibrosis in dry eye conditions. Invest Ophthalmol Vis Sci 51:844–849
Qazi Y, Maddula S, Ambati BK (2009) Mediators of ocular angiogemesis. J Genet 88:495–515
Cursiefen C, Kuchle M, Naumann GO (1997) Angiogenesis in corneal disease: histologic evaluation of 254 human corneal buttons with neovascularization. Cornea 17:611–613
Epstein RJ, Stulting RD, Hendricks RL (1987) Corneal neovascularization. Pathogenesis and inhibition. Cornea 6:250–257
Klinger P, Surmann-Schmitt C, Brem M, Swoboda B, Distler JH, Carl HD, von der Mark K, Hennig FF, Gelse K (2011) Chondromodulin I stabilizes the chondrocyte phenotype and inhibits endochondral ossification of cartilage repair tissue. Arthritis Rheum 63:2721–2731
Pufe T, Petersen WJ, Miosge N, Goldring MB, Mentlein R, Varoga DJ, Tillmann BN (2004) Endostatin/collagen XVIII—an inhibitor of angiogenesis is expressed in cartilage and fibrocartilage. Matrix Biol 23:267–276
Hopkinson A, Mclntosh RS, Tighe PJ, James DK, Dua HS (2006) Amniotic membrane for ocular surface reconstruction: donor variations and the effect of handling on TFG-beta content. Invest Ophthalmol Vis Sci 47:4316–4322
Tamhane A, Vajpayee BB, Biswas NR, Pandey RM, Sharma N, Titiyal JS, Tandon R (2005) Evaluation of amniotic membrane transplantation as an adjunct to medical therapy as compared with medical therapy alone in acute ocular burns. Ophthalmology 112:1963–1969
Azar DT (2006) Corneal angiogenic privilege: Angiogenic and antiangiogenic factors in corneal avascularity, vasculogenesis, and wound healing (an American Ophthalmological Society thesis). Trans Am Ophthamol Soc 104:264–302
Amano S, Rohan R, Kuroki M, Tolentino M, Adamis AP (1998) Requirement for vascular endothelial growth factor in wound- and inflammation-related corneal neovascularizaion. Invest Ophthalmol Vis Sci 39(1):18–22
Kvanta A, Sarman S, Fagerholm P, Seregard S, Steen B (2000) Expression of matrix metalloproteinase-2 (MMP-2) and vascular endothelial growth factor (VEGF) in inflammation-associated corneal neovascularization. Exp Eye Res 70:419–428
Mastyugin V, Mosaed S, Bonazzi A, Dunn MW, Schwartzman ML (2001) Corneal epithelial VEGF and cytochrome P450 4B1 expression in a rabbit model of closed eye contact lens wear. Curr Eye Res 23:1–10
Zheng M, Deshpande S, Lee S, Ferrara N, Rouse BT (2001) Contribution of vascular endothelial growth factor in the neovascularization process during the pathogenesis of herpetic stromal keratitis. J Virol 75:9828–9835
Mignatti P, Rifkin DB (1996) Plasminogen activators and matrix metalloproteinases in angiogenesis. Enzyme Protein 49:117–137
van Hinsbergh VW, Engelse MA, Quax PH (2006) Pericellular proteases in angiogenesis and vasculogenesis. Arterioscler Thromb Vasc Biol 26:716–728
Lan W, Petznick A, Heryati S, Rifada M, Tong L (2012) Nuclear factor- κB: Central regulator in ocular surface inflammation and disease. Ocul Surf 10:137–148
Chariot A, Meuwis MA, Bonif M, Leonard A, Merville MP, Gielen J, Piette J, Siebenlist U, Bours V (2003) NF-kappa B activating scaffold proteins as signaling molecules and putative therapeutic targets. Curr Med Chem 10:593–602
Srivastava SK, Ramana KV (2009) Focus on molecules: nuclear factor-kappa B. Exp Eye Res 88:2–3
Rajaiya J, Xiao J, Rajala RV, Chodosh J (2008) Human adenovirus type 19 infection of corneal cells induces p38 MAPK-dependent interleukin-8 expression. Virol J 5:17. doi:10.1186/1743-422X-5-17
Rajala MS, Rajala RV, Astley RA, Butt AL, Chodosh J (2005) Corneal cell survival in adenovirus type 19 infection requires phosphoinositide 3-kinase/Akt activation. J Virol 79:12332–12341
Saishin Y, Silva RL, Callahan K, Callahan K, Schoch C, Ahlheim M, Lai H, Kane F, Brazzell RK, Bodmer D, Campochiaro PA (2003) Periocular injection of microspheres containing PKC412 inhibits choroidal neovascularization in a porcine model. Invest Ophthalmol Vis Sci 44:4989–4993
Nakamura S, Chikaraishi Y, Tsuruma K, SHimazawa M, Hara H (2009) Ruboxistaurin, a PKC beta inhibitor, inhibits retinal neovascularization via suppression of phosphorylation of ERK1/2 and Akt. Exp Eye Res 90:137–145
Financial support
This study was supported by a grant from the Korea Healthcare Technology R&D Project, Ministry of Health and Welfare Affairs, Republic of Korea (grant #: HI12C0005).
Disclosure of potential conflicts of interest
The authors indicate no potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
H.S. Lee: conception and design; data analysis and interpretation; manuscript writing. J.H. Lee: data analysis and interpretation. C.E. Kim: data analysis and interpretation. J.W. Yang: conception and design; financial support; manuscript writing; final approval manuscript.
Rights and permissions
About this article
Cite this article
Lee, H.S., Lee, J.H., Kim, C.E. et al. Anti-neovascular effect of chondrocyte-derived extracellular matrix on corneal alkaline burns in rabbits. Graefes Arch Clin Exp Ophthalmol 252, 951–961 (2014). https://doi.org/10.1007/s00417-014-2633-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-014-2633-3