Abstract
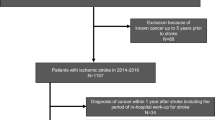
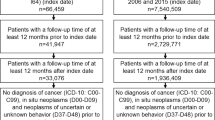
Ischemic stroke in patients with cancer is thought to be associated with a worse prognosis and might be the initial symptom of an unknown malignancy. However, diagnostic algorithms to reliably identify cancer-associated stroke have not been developed. In this retrospective single-centre analysis, 68 patients with ischemic stroke and an active solid malignancy were identified. Neurological assessment and outcome, cardiovascular risk factors, neuroimaging studies as well as laboratory findings were compared to 68 age- and sex-matched control subjects with ischemic stroke without diagnosis of cancer. Lung, pancreatic and renal cancer showed increased prevalences compared to those of the general population in Germany. Diagnosis of cancer was most often made within the 12 months preceding (32.4%) or during the diagnostic work-up for stroke (17.7%). Cancer-associated stroke was characterized by a more severe clinical deficit, frequent clinical deterioration (13.2 vs. 1.5%) or death (25 vs. 4.4%). Ischemic lesions often involved multiple territories (51.6 vs. 12.7%), more often with co-existing subacute and acute infarctions in imaging studies (54.8 vs. 11.1%). Patients with cancer had significantly higher levels of C-reactive protein, relative granulocytosis and serum lactate dehydrogenase activity. Using receiver operating characteristics-based multiple analysis, we developed a model using these parameters which detected cancer-associated stroke with a sensitivity of 75% and specificity of 95%. Our analysis suggests that a multiple algorithm combining the number of territories involved and laboratory signs of inflammation and cell turnover might identify patients with stroke suffering from previously unknown malignancy.


Similar content being viewed by others
References
GBD 2013 Mortality and Causes of Death Collaborators (2015) Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 385(9963):117–171. doi:10.1016/S0140-6736(14)61682-2
Bouillard JBB (1823) De l’Obliteration des veines et de son influence sur la formation des hydropisies partielles: consideration sur la hydropisies passive et general. Arch Gen Med 1:188–204
Graus F, Rogers LR, Posner JB (1985) Cerebrovascular complications in patients with cancer. Medicine (Baltimore) 64(1):16–35
Haddad TC, Greeno EW (2006) Chemotherapy-induced thrombosis. Thromb Res 118(5):555–568. doi:10.1016/j.thromres.2005.10.015
Bang OY, Seok JM, Kim SG, Hong JM, Kim HY, Lee J, Chung PW, Park KY, Kim GM, Chung CS, Lee KH (2011) Ischemic stroke and cancer: stroke severely impacts cancer patients, while cancer increases the number of strokes. J Clin Neurol 7(2):53–59. doi:10.3988/jcn.2011.7.2.53
Kim SG, Hong JM, Kim HY, Lee J, Chung PW, Park KY, Kim GM, Lee KH, Chung CS, Bang OY (2010) Ischemic stroke in cancer patients with and without conventional mechanisms: a multicenter study in Korea. Stroke 41(4):798–801. doi:10.1161/STROKEAHA.109.571356
Lee EJ, Nah HW, Kwon JY, Kang DW, Kwon SU, Kim JS (2014) Ischemic stroke in patients with cancer: is it different from usual strokes? Int J Stroke 9(4):406–412. doi:10.1111/ijs.12124
Gon Y, Okazaki S, Terasaki Y, Sasaki T, Yoshimine T, Sakaguchi M, Mochizuki H (2016) Characteristics of cryptogenic stroke in cancer patients. Ann Clin Transl Neurol 3(4):280–287. doi:10.1002/acn3.291
Schwarzbach CJ, Schaefer A, Ebert A, Held V, Bolognese M, Kablau M, Hennerici MG, Fatar M (2012) Stroke and cancer: the importance of cancer-associated hypercoagulation as a possible stroke etiology. Stroke 43(11):3029–3034. doi:10.1161/STROKEAHA.112.658625
Hron G, Kollars M, Weber H, Sagaster V, Quehenberger P, Eichinger S et al (2007) Tissue factor-positive microparticles: cellular origin and association with coagulation activation in patients with colorectal cancer. Thromb Haemost 97:119–123
Wahlund LO, Barkhof F, Fazekas F, Bronge L, Augustin M, Sjogren M, Wallin A, Ader H, Leys D, Pantoni L, Pasquier F, Erkinjuntti T, Scheltens P, European Task Force on Age-Related White Matter C (2001) A new rating scale for age-related white matter changes applicable to MRI and CT. Stroke 32(6):1318–1322
Kang DW, Chalela JA, Ezzeddine MA, Warach S (2003) Association of ischemic lesion patterns on early diffusion-weighted imaging with TOAST stroke subtypes. Arch Neurol 60(12):1730–1734. doi:10.1001/archneur.60.12.1730
Mun JK, Park SJ, Kim SJ, Bang OY, Chung CS, Lee KH, Kim GM (2016) Characteristic lesion pattern and echocardiographic findings in extra-cardiac shunt-related stroke. J Neurol Sci 369:176–180. doi:10.1016/j.jns.2016.08.024
Toiyama Y, Inoue Y, Saigusa S, Kawamura M, Kawamoto A, Okugawa Y, Hiro J, Tanaka K, Mohri Y, Kusunoki M (2013) C-reactive protein as predictor of recurrence in patients with rectal cancer undergoing chemoradiotherapy followed by surgery. Anticancer Res 33(11):5065–5074
Jafri SH, Shi R, Mills G (2013) Advance lung cancer inflammation index (ALI) at diagnosis is a prognostic marker in patients with metastatic non-small cell lung cancer (NSCLC): a retrospective review. BMC Cancer 13:158. doi:10.1186/1471-2407-13-158
Zhang Y, Jiang C, Li J, Sun J, Qu X (2015) Prognostic significance of preoperative neutrophil/lymphocyte ratio and platelet/lymphocyte ratio in patients with gallbladder carcinoma. Clin Transl Oncol 17(10):810–818. doi:10.1007/s12094-015-1310-2
Gallo M, Sapio L, Spina A, Naviglio D, Calogero A, Naviglio S (2015) Lactic dehydrogenase and cancer: an overview. Front Biosci (Landmark Ed) 20:1234–1249
Khorana AA (2009) Cancer and thrombosis: implications of published guidelines for clinical practice. Ann Oncol 20(10):1619–1630. doi:10.1093/annonc/mdp068
Timp JF, Braekkan SK, Versteeg HH, Cannegieter SC (2013) Epidemiology of cancer-associated venous thrombosis. Blood 122(10):1712–1723. doi:10.1182/blood-2013-04-460121
Prandoni P, Falanga A, Piccioli A (2007) Cancer, thrombosis and heparin-induced thrombocytopenia. Thromb Res 120(Suppl 2):S137–S140. doi:10.1016/S0049-3848(07)70143-3
Cestari DM, Weine DM, Panageas KS, Segal AZ, DeAngelis LM (2004) Stroke in patients with cancer: incidence and etiology. Neurology 62(11):2025–2030
Grecu N, Tiu C, Terecoasa E, Bajenaru O (2014) Endocarditis and stroke. Maedica (Buchar) 9(4):375–381
Abdelgawad EA, Higazi MM, Abdelbaky AO, Abdelghany HS (2016) Diagnostic performance of CT cerebral blood volume colour maps for evaluation of acute infarcts; comparison with diffusion-weighted MRI within 12 h of major stroke onset. J Neuroradiol. doi:10.1016/j.neurad.2016.10.005
Schaefer PW, Souza L, Kamalian S, Hirsch JA, Yoo AJ, Kamalian S, Gonzalez RG, Lev MH (2015) Limited reliability of computed tomographic perfusion acute infarct volume measurements compared with diffusion-weighted imaging in anterior circulation stroke. Stroke 46(2):419–424. doi:10.1161/STROKEAHA.114.007117
el-Shami K, Griffiths E, Streiff M, (2007) Nonbacterial thrombotic endocarditis in cancer patients: pathogenesis, diagnosis, and treatment. Oncologist 12(5):518–523. doi:10.1634/theoncologist.12-5-518
Wun T, White RH (2009) Venous thromboembolism (VTE) in patients with cancer: epidemiology and risk factors. Cancer Invest 27(Suppl 1):63–74. doi:10.1080/07357900802656681
Horowitz N, Brenner B (2008) Thrombophilia and cancer. Pathophysiol Haemost Thromb 36(3–4):131–136. doi:10.1159/000175151
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical standards
This retrospective study has been approved by the local Ethics Committee (University of Ulm, Germany) and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Katharina Althaus and Jan Lewerenz contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kassubek, R., Bullinger, L., Kassubek, J. et al. Identifying ischemic stroke associated with cancer: a multiple model derived from a case–control analysis. J Neurol 264, 781–791 (2017). https://doi.org/10.1007/s00415-017-8432-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-017-8432-0