Abstract
Background
After infant deaths due to non-accidental head injury (NAHI) with subdural hematoma (SDH), the magistrates ask experts to date the traumatic event. To do so, the expert only has tools based on adult series of NAHI. We aimed to develop an SDH dating system applicable to infants aged under 3 years.
Methods and results
We studied a retrospective multicenter collection of 235 infants who died between the ages of 0 and 36 months, diagnosed with SDH by forensic pathological examination and with known posttraumatic interval (PTI). Two pathologists assessed blindly and independently 12 histomorphological criteria relating to the clot and 14 relating to the dura mater in 73 victims (31 girls, 42 boys) whose median age was 3.8 months. Histopathological changes were significantly correlated with PTI for the appearance of red blood cells (RBCs) and the presence or absence of siderophages, and regarding the dura mater, the quantity of lymphocytes, macrophages, and siderophages; presence or absence of hematoidin deposits; collagen and fibroblast formation; neomembrane thickness; and presence or absence of neovascularization. Dating systems for SDH in adults are not applicable to infants. Notably, neomembrane of organized connective tissue is formed earlier in infants than in adults.
Conclusion
Our dating system improves the precision and reliability of forensic pathological expert examination of NAHI, particularly for age estimation of SDH in infants. However, the expert can only define a time interval. Histopathology is indispensable to detect repetitive trauma.

Similar content being viewed by others
Abbreviations
- NAHI:
-
Non-accidental head injury
- PTI:
-
Posttraumatic interval
- SDH:
-
Subdural hematoma
- RBCs:
-
Red blood cells
- PMNs:
-
Polymorphonuclear neutrophils
References
Haute Autorité de Santé - Recommandation : Syndrome du bébé secoué [Internet]. 2011 Mai [cited 2016 Nov 22]. Available from: http://www.has-sante.fr/portail/jcms/c_1095929/fr/recommandation-syndrome-du-bebe-secoue
Barlow KM, Minns RA (2000) Annual incidence of shaken impact syndrome in young children. Lancet 356(9241):1571–1572
Jayawant S, Rawlinson A, Gibbon F, Price J, Schulte J, Sharples P, Sibert JR, Kemp AM (1998) Subdural haemorrhages in infants: population based study. BMJ 317(7172):1558–1561
Mireau E (2005) Syndrome du bébé secoué, hématome sous-dural du nourrisson et maltraitance a propos d’une série de 404 cas. [Paris]: Paris V Rene Descartes
Duckett S (1995) Pediatric neuropathology. Williams and Wilkins, Pennsylvania
Leestma JE (2014) Forensic neuropathology, 3rd edn. CRC Press, Bosa Roca
Adamsbaum C, Rambaud C (2012) Abusive head trauma: don’t overlook bridging vein thrombosis. Pediatr Radiol 42(11):1298–1300
Munro D, Merritt HH (1936) Surgical pathology of subdural hematoma : based on a study of one hundred and five cases. Arch Neurol Psychiatr 35(1):64–78
Pearl GS (1998) Traumatic neuropathology. Clin Lab Med 18(1):39–64
Oehmichen M, Auer RN, König HG (2006) Forensic neuropathology and associated neurology. Springer Science & Business Media, Berlin
DiMaio VJM, Dana SE (2007) Handbook of forensic pathology, 2nd edn. Taylor & Francis, Boca Raton, United States
Walter T, Meissner C, Oehmichen M (2009) Pathomorphological staging of subdural hemorrhages: statistical analysis of posttraumatic histomorphological alterations. Leg Med Tokyo Jpn 11(Suppl 1):S56–S62
van den Bos D, Zomer S, Kubat B (2014) Dare to date: age estimation of subdural hematomas, literature, and case analysis. Int J Legal Med 128(4):631–640
Leary T (1934) Subdural hemorrhages. J Am Med Assoc 103(12):897–903
Andrew M, Paes B, Milner R, Johnston M, Mitchell L, Tollefsen DM et al (1987) Development of the human coagulation system in the full-term infant. Blood 70(1):165–172
Andrew M, Vegh P, Johnston M, Bowker J, Ofosu F, Mitchell L (1992) Maturation of the hemostatic system during childhood. Blood 80(8):1998–2005
Toulon P, De Pooter N (2013) Hemostase en pediatrie. 42ème Colloque National des Biologistes des Hopitaux 2013 Oct 2, Strasbourg
Haute Autorité de Santé - Recommandation : Syndrome du bébé secoué [Internet]. 2017 Sep [cited 2016 Nov 22]. Available from: http://www.has-sante.fr/portail/jcms/c_1095929/fr/recommandation-syndrome-du-bebe-secoue
Gilliland MG (1998) Interval duration between injury and severe symptoms in nonaccidental head trauma in infants and young children. J Forensic Sci 43(3):723–725
Starling SP, Patel S, Burke BL, Sirotnak AP, Stronks S, Rosquist P (2004) Analysis of perpetrator admissions to inflicted traumatic brain injury in children. Arch Pediatr Adolesc Med 158(5):454–458
Adamsbaum C, Morel B, Ducot B, Antoni G, Rey-Salmon C (2014) Dating the abusive head trauma episode and perpetrator statements: key points for imaging. Pediatr Radiol 44(Suppl 4):S578–S588
Willman KY, Bank DE, Senac M, Chadwick DL (1997) Restricting the time of injury in fatal inflicted head injuries. Child Abuse Negl 21(10):929–940
Fortin G, Stipanicic A (2010) How to recognize and diagnose abusive head trauma in infants. Ann Phys Rehabil Med 53(10):693–710
Rao MG, Singh D, Vashista RK, Sharma SK (2016) Dating of acute and subacute subdural haemorrhage: a histo-pathological study. J Clin Diagn Res 10(7):HC01–HC07
Feldman KW, Sugar NF, Browd SR (2015) Initial clinical presentation of children with acute and chronic versus acute subdural hemorrhage resulting from abusive head trauma. J Neurosurg Pediatr 16(2):177–185
Adamsbaum C (2013) Maltraitance chez l’enfant. Lavoisier MSP, Paris
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 19 kb)
ESM 2
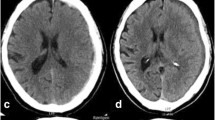
Qualitative classification of RBCs, from left to right: HES × 40. a Intact (discoid shape with a distinct contour and uniform staining); b Lysed cells (blurred contours, non-uniform staining): minimal lysis; c Distinct lysis; d Mixed. (PNG 8587 kb)
ESM 3
Semi-quantitative classification of PMNs: a No or very rare neutrophils, HES × 20; b Up to three clumps, HES × 20; c More than three clumps, HES × 20; d: Diffuse, HES × 20. (PNG 8941 kb)
ESM 4
Qualitative classification of neovascularization: a Capillary proliferation, HES × 10; b Giant capillaries, HES × 10; c Arterioles, HES × 20 (PNG 20735 kb)
ESM 5
Most important histological features over time. a Lysed red cells from 2 days onward, HES × 10; b Siderophages at 3 days in the dura mater and the clot, HES × 10; c Hemosiderin deposit from 12 days onward in the dura mater, Perls stain × 40, fibrinous organization; d Presence of fibroblasts and collagen from 3 days onward, HES × 30; e Neomembrane formation from 4 days onward, HES × 5; f neovascularization from 6 days onward, HES × 10. (PNG 3756 kb)
Rights and permissions
About this article
Cite this article
Delteil, C., Humez, S., Boucekine, M. et al. Histological dating of subdural hematoma in infants. Int J Legal Med 133, 539–546 (2019). https://doi.org/10.1007/s00414-018-1980-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-018-1980-8