Abstract
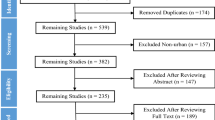
Worldwide, many people are exposed to biannual time changes. The benefit of Daylight Saving Time (DST) is controversially discussed and its impact on human health is largely unknown. The present study examines, whether effects of these time changes are seen in a forensic autopsy database. The mortality study is based on autopsy protocols provided by the Institute of Legal Medicine, University Clinic of the Goethe-University Frankfurt/Main, covering a period of 10 years (2006–2015). Data regarding mode and cause of death, age, and gender were evaluated for 4 weeks around the transition to and from DST in spring and autumn. A significant (p = 0.04) elevation in the number of autopsies was observed in the first week following the switch to DST in spring, but no significant changes were noted in autumn. Gender-specific analysis indicated that the autopsy rate of females showed a significant (p = 0.01) peak in the first and a decline (p = 0.05) in the second week following the switch to DST. Differences in non-natural death cases primarily included traffic accidents and suicides, in natural death cases fatal cardiac diseases like cardiac insufficiency and acute myocardial infarction. The number of suicides was low (p = 0.05) before, but high (p = 0.07) in the weeks after the introduction of DST. The present evaluation confirmed a potential effect of DST, such as a significant higher autopsy rate in spring during the first week after the introduction to DST. Moreover, a relation between the introduction to DST in spring and an increase in suicide cases was observed.

Similar content being viewed by others
References
Havranek T, Herman D, Irsova Z (2016) Does daylight saving save energy? A meta-analysis. Prague: Institute of Economic Studies, Faculty of Social Sciences Charles University. IES Working Paper: 24/2016
Kantermann T, Juda M, Merrow M, Roenneberg T (2007) The human circadian clock’s seasonal adjustment is disrupted by daylight saving time. Curr Biol 17:1996–2000. https://doi.org/10.1016/j.cub.2007.10.025
Allebrandt KV, Teder-Laving M, Kantermann T, Peters A, Campbell H, Rudan I, Wilson JF, Metspalu A, Roenneberg T (2014) Chronotype and sleep duration: the influence of season of assessment. Chronobiol Int 31:731–740. https://doi.org/10.3109/07420528.2014.901347
Lahti TA, Leppämäki S, Ojanen SM, Haukka J, Tuulio-Henriksson A, Lönnqvist J, Partonen T (2006) Transition into daylight saving time influences the fragmentation of the rest-activity cycle. J Circadian Rhythms 4:1. https://doi.org/10.1186/1740-3391-4-1
Kountouris Y, Remoundou K (2014) About time: Daylight Saving Time transition and individual well-being. Econ Lett 122:100–103. https://doi.org/10.1016/j.econlet.2013.10.032
Shapiro CM, Blake F, Fossey E, Adams B (1990) Daylight saving time in psychiatric illness. J Affect Disord 19:177–181. https://doi.org/10.1016/0165-0327(90)90089-Q
Barnes CM, Wagner DT (2009) Changing to daylight saving time cuts into sleep and increases workplace injuries. J Appl Psychol 94:1305–1317. https://doi.org/10.1037/a0015320
Lahti T, Sysi-Aho J, Haukka J, Partonen T (2011) Work-related accidents and daylight saving time in Finland. Occup Med (Lond) 61:26–28. https://doi.org/10.1093/occmed/kqq167
Lahti T, Nysten E, Haukka J, Sulander P, Partonen T (2010) Daylight saving time transitions and road traffic accidents. J Environ Public Health 2010:657167. https://doi.org/10.1155/2010/657167
Varughese J, Allen RP (2001) Fatal accidents following changes in daylight savings time: the American experience. Sleep Med 2:31–36. https://doi.org/10.1016/S1389-9457(00)00032-0
Coate D, Markowitz S (2004) The effects of daylight and daylight saving time on US pedestrian fatalities and motor vehicle occupant fatalities. Accid Anal Prev 36:351–357. https://doi.org/10.1016/S0001-4575(03)00015-0
Huang A, Levinson D (2010) The effects of daylight saving time on vehicle crashes in Minnesota. J Saf Res 41:513–520. https://doi.org/10.1016/j.jsr.2010.10.006
Janszky I, Ljung R (2008) Shifts to and from daylight saving time and incidence of myocardial infarction. N Engl J Med 359:1966–1968. https://doi.org/10.1056/NEJMc0807104
Janszky I, Ahnve S, Ljung R, Mukamal KJ, Gautam S, Wallentin L, Stenestrand U (2012) Daylight saving time shifts and incidence of acute myocardial infarction – Swedish Register of Information and Knowledge About Swedish Heart Intensive Care Admissions (RIKS-HIA). Sleep Med 13:237–242. https://doi.org/10.1016/j.sleep.2011.07.019
Kirchberger I, Wolf K, Heier M, Kuch B, von Scheidt W, Peters A, Meisinger C (2015) Are daylight saving time transitions associated with changes in myocardial infarction incidence? Results from the German MONICA/KORA Myocardial Infarction Registry. BMC Public Health 15:778. https://doi.org/10.1186/s12889-015-2124-4
European Parliament. Time change arrangements (2018) European Parliament resolution of 8 February 2018 on time change arrangements (2017/2968(RSP)). P8_TA-PROV(2018)0043
Anglmayer I, Ex-Post Evaluation Unit (2017) EU summer-time arrangements under Directive 2000/84/EC. Brussels: ex-post evaluation unit of the Directorate for Impact Assessment and European Added Value, Directorate–General for Parliamentary Research Services of the Secretariat of the European Parliament. Report Nr: PE611006
Ackermann H (2017) BiAS. für Windows. Version 11. Epsilon-Verlag, Hochheim Darmstadt
Ellis DA, Luther K, Jenkins R (2018) Missed medical appointments during shifts to and from daylight saving time. Chronobiol Int 35:584–588. https://doi.org/10.1080/07420528.2017.1417313
Lahti TA, Leppämäki S, Lönnqvist J, Partonen T (2006) Transition to daylight saving time reduces sleep duration plus sleep efficiency of the deprived sleep. Neurosci Lett 406:174–177. https://doi.org/10.1016/j.neulet.2006.07.024
Sharma BR (2007) Sudden infant death syndrome: a subject of medicolegal research. Am J Forensic Med Pathol 28:69–72. https://doi.org/10.1097/01.paf.0000220934.18700.ef
Vennemann MM, Hense HW, Bajanowski T, Blair PS, Complojer C, Moon RY, Kiechl-Kohlendorfer U (2012) Bed sharing and the risk of sudden infant death syndrome: can we resolve the debate? J Pediatr 160:44–48. https://doi.org/10.1016/j.jpeds.2011.06.052
Vennemann MM, Bajanowski T, Brinkmann B, Jorch G, Sauerland C, Mitchell EA, GeSID Study Group (2009) Sleep environment risk factors for sudden infant death syndrome: the German sudden infant death syndrome study. Pediatrics 123:1162–1170 https://doi.org/10.1542/peds.2008-0505
Moon RY, Task Force on Sudden Infant Death Syndrome (2016) SIDS and other sleep-related infant deaths: evidence base for 2016 updated recommendations for a safe infant sleeping environment. Pediatrics 138:e20162940. https://doi.org/10.1542/peds.2016-2940
Manfredini R, Fabbian F, De Giorgi A, Zucchi B, Cappadona R, Signani F, Katsiki N, Mikhailidis DP (2018) Daylight saving time and myocardial infarction: should we be worried? A review of the evidence. Eur Rev Med Pharmacol Sci 22:750–755. https://doi.org/10.26355/eurrev_201802_14306
Čulić V, Eterović D, Mirić D (2005) Meta-analysis of possible external triggers of acute myocardial infarction. Int J Cardio 99:1–8. https://doi.org/10.1016/j.ijcard.2004.01.008
Sandhu A, Seth M, Gurm HS (2014) Daylight savings time and myocardial infarction. Open Heart 1:e000019. https://doi.org/10.1136/openhrt-2013-000019
Elliott WJ (1998) Circadian variation in the timing of stroke onset: a meta-analysis. Stroke 29:992–996. https://doi.org/10.1161/01.STR.29.5.992
Foerch C, Korf HW, Steinmetz H, Sitzer M, Arbeitsgruppe Schlaganfall Hessen (2008) Abrupt shift of the pattern of diurnal variation in stroke onset with daylight saving time transitions. Circulation 118:284–290. https://doi.org/10.1161/CIRCULATIONAHA.108.771246
Sipilä JO, Ruuskanen JO, Rautava P, Kytö V (2016) Changes in ischemic stroke occurrence following daylight saving time transitions. Sleep Med 27-28:20–24. https://doi.org/10.1016/j.sleep.2016.10.009
International Transport Forum (ITF) (2017) Road safety annual report 2017. OECD Publishing, Paris. https://doi.org/10.1787/irtad-2017-en
McDonald KC, Saunders KE, Geddes JR (2017) Sleep problems and suicide associated with mood instability in the adult psychiatric morbidity survey, 2007. Aust N Z J Psychiatry 51:822–828. https://doi.org/10.1177/0004867416687398
Pigeon WR, Pinquart M, Conner K (2012) Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry 73:e1160–e1167. https://doi.org/10.4088/JCP.11r07586
Tonetti L, Erbacci A, Fabbri M, Martoni M, Natale V (2013) Effects of transitions into and out of daylight saving time on the quality of the sleep/wake cycle: an actigraphic study in healthy university students. Chronobiol Int 30:1218–1222. https://doi.org/10.3109/07420528.2013.812651
Lahti TA, Leppämäki S, Lönnqvist J, Partonen T (2008) Transitions into and out of daylight saving time compromise sleep and the rest-activity cycles. BMC Physiol 8:3. https://doi.org/10.1186/1472-6793-8-3
Berk M, Dodd S, Hallam K, Berk L, Gleeson J, Henry M (2008) Small shifts in diurnal rhythms are associated with an increase in suicide: the effect of daylight saving. Sleep Biol Rhythms 6:22–25. https://doi.org/10.1111/j.1479-8425.2007.00331.x
Harvey AG (2008) Sleep and circadian rhythms in bipolar disorder: seeking synchrony, harmony, and regulation. Am J Psychiatry 165:820–829. https://doi.org/10.1176/appi.ajp.2008.08010098
Lahti TA, Haukka J, Lönnqvist J, Partonen T (2008) Daylight saving time transitions and hospital treatments due to accidents or manic episodes. BMC Public Health 8(74). https://doi.org/10.1186/1471-2458-8-74
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Lindenberger, L.M., Ackermann, H. & Parzeller, M. The controversial debate about daylight saving time (DST)—results of a retrospective forensic autopsy study in Frankfurt/Main (Germany) over 10 years (2006–2015). Int J Legal Med 133, 1259–1265 (2019). https://doi.org/10.1007/s00414-018-1960-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-018-1960-z