Abstract
Purpose
Surgery for primary hyperparathyroidism is undertaken by many specialties but predominantly endocrine and ear, nose and throat (ENT) surgeons. There is currently no consensus on the peri-operative management of primary hyperparathyroidism. We sought to determine current surgical practice and identify any inter-specialty variation in the United Kingdom (UK).
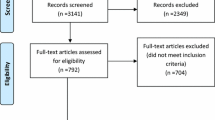
Methods
An online survey was disseminated to members of the British Association of Endocrine & Thyroid Surgeons (BAETS) in the UK.
Results
78 surgeons responded (40 Endocrine, 37 ENT and 1 maxillofacial). 90% of surgeons used ultrasound and sestamibi for pre-operative localisation. Intraoperative frozen section (31%) and parathyroid hormone monitoring (41%) were the most common adjuncts used intraoperatively. 68% of surgeons did not use any wound drains. Nearly two-thirds of surgeons (64%) discharged patients from the clinic within 3 months, There were some significant differences (p < 0.05) in particular areas of practice between endocrine and ENT surgeons (%, p): use of single-photon emission computed tomography (SPECT) (Endocrine 25% vs. ENT 5%), preoperative laryngeal assessment (endocrine 58% vs. ENT 95%), intraoperative laryngeal nerve monitoring (endocrine 35% vs. ENT 68%), use of monopolar diathermy (endocrine 58% vs. ENT 22%), bipolar diathermy (endocrine 60% vs. 89%) and surgical ties (endocrine 48% vs. ENT 19%).
Conclusion
Our study demonstrates some similarities as well as some notable differences in practice between endocrine and ENT surgeons, and therefore, highlights the need for national consensus with respect to some key areas in parathyroid surgery.
Similar content being viewed by others
References
Melton LJIII (2002) The epidemiology of primary hyperparathyroidism in North America. J Bone Miner Res 17S2:N12–N17
Wermers RA, Khosla S, Atkinson EJ, Achenbach SJ, Oberg AL, Grant CS, Melton LJ 3rd (2006) Incidence of primary hyperparathyroidism in Rochester, Minnesota, 1993–2001: an update on the changing epidemiology of the disease. J Bone Miner Res 21(1):171–177
Wieneke JA, Smith A (2008) Parathyroid adenoma. Head Neck Pathol 2(4):305–308
Maniakas A, Christopoulos A, Bissada E, Guertin L, Olivier MJ, Malaise J, Ayad T (2017) Peri-operative practices in thyroid surgery: an international survey. Head Neck 39(7):1296–1305
BAETS (2003) BAETS guidelines. http://www.baets.org.uk/wp-content/uploads/2013/02/BAETS-Guidelines-2003.pdf. Accessed 18 June 2018
BAETS (2018) BAETS audit report. http://www.baets.org.uk/wp-content/uploads/BAETS-Audit-National-Report-2017.pdf. Accessed 18 June 2018
Cheung K, Wang TS, Farrokhyar F, Roman SA, Sosa JA (2012) A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol 19(2):577–583
Nafisi Moghadam R, Amlelshahbaz AP, Namiranian N, Sobhan-Ardekani M, Emami-Meybodi M, Dehghan A, Rahmanian M, Razavi-Ratki SK (2017) Comparative diagnostic performance of ultrasonography and 99mTc-Sestamibi scintigraphy for parathyroid adenoma in primary hyperparathyroidism; systematic review and meta-analysis. Asian Pac Cancer Prev 18(12):3195–3200
Siperstein A, Berber E, Mackey R, Alghoul M, Wagner K, Milas M (2004) Prospective evaluation of sestamibi scan, ultrasonography, and rapid PTH to predict the success of limited exploration for sporadic primary hyperparathyroidism. Surgery 136(4):872–880
Raruenrom Y, Theerakulpisut D, Wongsurawat N, Somboonporn C (2018) Diagnostic accuracy of planar, SPECT, and SPECT/CT parathyroid scintigraphy protocols in patients with hyperparathyroidism. Nucl Med Rev Cent East Eur 21(1):20–25
Shen W, Düren M, Morita E, Higgins C, Duh QY, Siperstein AE, Clark OH (1996) Reoperation for persistent or recurrent primary hyperparathyroidism. Arch Surg 131(8):861–867 (discussion 867–9)
Gotway MB, Reddy GP, Webb WR et al (2001) Comparison between MR imaging and 99mTc MIBI scintigraphy in the evaluation of recurrent of persistent hyperparathyroidism. Radiology 218(3):783–790
Reading CC, Gorman CA (1993) Thyroid imaging techniques. Clin Lab Med 13(3):711–724
Marmin C, Toledano M, Lemaire S, Boury S, Mordon S, Ernst O (2012) Computed tomography of the parathyroids: the value of density measurements to distinguish between parathyroid adenomas of the lymph nodes and the thyroid parenchyma. Diagn Interv Imaging 93(7–8):597–603
Yamada T, Ikuno M, Shinjo Y, Hiroishi A, Matsushita S, Morimoto T, Kumano R, Yagihashi K, Katabami T (2017) Selective venous sampling for primary hyperparathyroidism: how to perform an examination and interpret the results with reference to thyroid vein anatomy. Jpn J Radiol 35(8):409–416
Jones JJ, Brunaud L, Dowd CF, Duh QY, Morita E, Clark OH (2002) Accuracy of selective venous sampling for intact parathyroid hormone in difficult patients with recurrent or persistent hyperparathyroidism. Surgery 132(6):944–950 (discussion 950–1)
Chaffanjon PC, Voirin D, Vasdev A, Chabre O, Kenyon NM, Brichon PY (2004) Selective venous sampling in recurrent and persistent hyperparathyroidism: indication, technique, and results. World J Surg 28(10):958–961 (Epub 2004 Sep 29)
Sinclair CF, Bumpous JM, Haugen BR, Chala A, Meltzer D, Miller BS, Tolley NS, Shin JJ, Woodson G, Randolph GW (2016) Laryngeal examination in thyroid and parathyroid surgery: an American Head and Neck Society consensus statement: AHNS Consensus Statement. Head Neck 38(6):811–819
Farrag TY, Samlan RA, Lin FR, Tufano RP (2006) The utility of evaluating true vocal fold motion before thyroid surgery. Laryngoscope 116(2):235–238
Barczynski M, Konturek A, Hubalewska-Dydejczyk A et al (2009) Evaluation of Halle, Miami, Rome, and Vienna intraoperative iPTH assay criteria in guiding minimally invasive parathyroidectomy. Langenbecks Arch Surg 394(5):843–849
Patel KN, Caso R (2016) Intraoperative parathyroid hormone monitoring: optimal utilization. Surg Oncol Clin N Am 25(1):91–101
Morris LF, Zanocco K, Ituarte PH, Ro K, Duh QY, Sturgeon C, Yeh MW (2010) The value of intraoperative parathyroid hormone monitoring in localized primary hyperparathyroidism: a cost analysis. Ann Surg Oncol 17(3):679–685
Patel HP, Chadwick DR, Harrison BJ, Balasubramanian SP (2012) Systematic review of intravenous methylene blue in parathyroid surgery. Br J Surg 99(10):1345–1351
Randolph GW, Dralle H, International Intraoperative Monitoring Study Group, Abdullah H, Barczynski M, Bellantone R, Brauckhoff M, Carnaille B, Cherenko S, Chiang FY, Dionigi G, Finck C, Hartl D, Kamani D, Lorenz K, Miccolli P, Mihai R, Miyauchi A, Orloff L, Perrier N, Poveda MD, Romanchishen A, Serpell J, Sitges-Serra A, Sloan T, Van Slycke S, Snyder S, Takami H, Volpi E, Woodson G (2011) Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope 121(Suppl 1):S1–S16
Ghani U, Assad S, Assad S (2016) Role of intraoperative nerve monitoring during parathyroidectomy to prevent recurrent laryngeal nerve injury. Cureus 8(11):e880
Mourad M, Kadakia S, Jategaonkar A, Gordin E, Ducic Y (2017) Intraoperative nerve monitoring during parathyroid surgery: the fort worth experience. Head Neck 39(8):1662–1664
Malik R, Linos D (2016) Intraoperative neuromonitoring in thyroid surgery: a systematic review. World J Surg 40(8):2051–2058
Tabaqchali MA, Hanson JM, Proud G (1999) Drains for thyroidectomy/parathyroidectomy: fact or fiction? Ann R Coll Surg Engl 81(5):302–305
Doran HE, England J, Palazzo F, British Association of Endocrine and Thyroid Surgeons (2012) Questionable safety of thyroid surgery with same day discharge. Ann R Coll Surg Engl 94(8):543–547
Lou I, Balentine C, Clarkson S, Schneider DF, Sippel RS, Chen H (2017) How long should we follow patients after apparently curative parathyroidectomy? Surgery 161(1):54–61
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Human and animal participants’ statement
No human or animal participants were involved in this study.
Rights and permissions
About this article
Cite this article
Varadharajan, K., Choudhury, N. Current practice in the surgical management of parathyroid disorders: a United Kingdom survey. Eur Arch Otorhinolaryngol 275, 2549–2553 (2018). https://doi.org/10.1007/s00405-018-5094-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-5094-1