Abstract
Purpose
Inositol (ISL) embraces a family of simple carbohydrates with insulin-sensitizing properties, whose most common isoforms are Myo-inositol (MYO) and d-chiro inositol (DCI). The aim of the present study was to assess the efficacy and safety of ISL supplementation during pregnancy for the prevention of gestational diabetes (GDM).
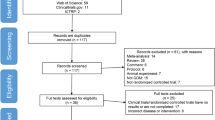
Methods
We conducted a systematic literature search in electronic databases until October 2017. We included all randomized controlled trials (RCTs) comparing pregnant women with GDM who were randomized to either ISL (i.e., intervention group) or either placebo or no treatment (i.e., control group). The primary outcome was the preventive effect on GDM, defined as the rate of GDM in women without a prior diagnosis of GDM. Pooled results were expressed as odds ratio (OR) with a 95% confidence interval (95% CI).
Results
Five RCTs were included (including 965 participants). ISL supplementation was associated with lower rate of GDM (OR 0.49, 95% CI 0.24–1.03, p = 0.01) and lower preterm delivery rate (OR 0.35, 95% CI 0.17–0.74, p = 0.006). No adverse effects were reported. Adjusting for the type of intervention (MYO 2 g twice daily vs MYO 1100 mg plus DCI 27.6 mg daily), a significant effect was found only in patients receiving 2 g MYO twice daily.
Conclusions
ISLs administration during pregnancy appears to be safe and may represent a novel strategy for GDM prevention. In particular, the double administration of MYO 2 g per day may improve the glycemic homeostasis and may reduce GDM rate and preterm delivery rate.



Similar content being viewed by others
References
Baz B, Riveline JP, Gautier JF (2016) Endocrinology of pregnancy: gestational diabetes mellitus: definition, aetiological and clinical aspects. Eur J Endocrinol 174(2):R43–R51
Caissutti C, Berghella V (2017) Scientific evidence for different options for GDM screening and management: controversies and review of the literature. Biomed Res Int 2017:2746471
Farrar D, Simmonds M, Bryant M, Sheldon TA, Tuffnell D, Golder S, Dunne F, Lawlor DA (2016) Hyperglycaemia and risk of adverse perinatal outcomes: systematic review and meta-analysis. BMJ 13(354):i4694
Vitagliano A, Noventa M, Gizzo S (2015) Is it time to consider patients suffering from endometriosis-related infertility as “novel candidates” for targeted peri-conceptional d-chiro inositol supplementation? Hypothesis, rationale and some considerations. J Assist Reprod Genet 32(3):407–408
Pintaudi B, Di Vieste G, Bonomo M (2016) The effectiveness of Myo-inositol and d-chiro inositol treatment in type 2 diabetes. Int J Endocrinol 2016:9132052
Dell’Edera D, Sarlo F, Allegretti A, Simone F, Lupo MG, Epifania AA (2017) The influence of d-chiro-inositol and d-myo-inositol in pregnant women with glucose intolerance. Biomed Rep. 7(2):169–172
Muscogiuri G, Palomba S, Laganà AS, Orio F (2016) Inositols in the treatment of insulin-mediated diseases. Int J Endocrinol 2016:3058393
Noventa M, Vitagliano A, Quaranta M, Borgato S, Abdulrahim B, Gizzo S (2016) Preventive and therapeutic role of dietary inositol supplementation in periconceptional period and during pregnancy: a summary of evidences and future applications. Reprod Sci 23(3):278–288
Nas K, Tűű L (2017) A comparative study between myo-inositol and metformin in the treatment of insulin-resistant women. Eur Rev Med Pharmacol Sci 21(2 Suppl):77–82
Costabile L, Unfer V (2017) Treatment of gestational diabetes mellitus with myo-inositol: analyzing the cutting edge starting from a peculiar case. Eur Rev Med Pharmacol Sci. 21(2 Suppl):73–76
Crawford TJ, Crowther CA, Alsweiler J, Brown J (2015) Antenatal dietary supplementation with myo-inositol in women during pregnancy for preventing gestational diabetes. Cochrane Database Syst Rev. 12:CD011507
Santamaria A, Di Benedetto A, Petrella E, Pintaudi B, Corrado F, D’Anna R, Neri I, Facchinetti F (2016) Myo-inositol may prevent gestational diabetes onset in overweight women: a randomized, controlled trial. J Matern Fetal Neonatal Med 29(19):3234–3237
Farren M, Daly N, McKeating A, Kinsley B, Turner MJ, Daly S (2017) The prevention of gestational diabetes mellitus with antenatal oral inositol supplementation: a randomized controlled trial. Diabetes Care 40(6):759–763
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Corrado F, D’Anna R, Di Vieste G, Giordano D, Pintaudi B, Santamaria A, DiBenedetto A (2011) The effect of myoinositol supplementation on insulin resistance inpatients with gestational diabetes. Diabet Med 28(8):972–975
Matarrelli B, Vitacolonna E, D’Angelo M, Pavone G, Mattei PA, Liberati M, Celentano C (2013) Effect of dietary myo-inositol supplementation in pregnancy on theincidence of maternal gestational diabetes mellitus and fetal outcomes: a randomized controlled trial. J Matern Fetal Neonatal Med 26(10):967–972
Malvasi A, Kosmas I, Mynbaev OA, Sparic R, Gustapane S, Guido M, Tinelli A (2017) Can trans resveratrol plus d-chiro-inositol and myo-inositol improve maternal metabolic profile in overweight pregnant patients? Clin Ther 168(4):e240–e247
Lubin V, Shojai R, Darmon P, Cosson E (2016) A pilot study of gestational diabetes mellitus not controlled by diet alone: first-line medical treatment with myoinositol may limit the need for insulin. Diabetes Metab 42(3):192–195
Ferrari F, Facchinetti F, Ontiveros AE, Roberts RP, Saade MM, Blackwell SC, Sibai BM, Refuerzo JS, Longo M (2016) The effect of combined inositol supplementation on maternal metabolic profile in pregnancies complicated by metabolic syndrome and obesity. Am J Obstet Gynecol 215(4):503.e1–503.e8
Groenen PM, Roes EM, Peer PG, Merkus HM, Steegers EA, Steegers-Theunissen RP (2006) Myo-inositol, glucose and zinc concentrations determined in the preconceptional period, during and after pregnancy. Eur J Obstet Gynecol Reprod Biol 127(1):50–55
Facchinetti F, Pignatti L, Interdonato ML, Neri I, Bellei G, D’Anna R (2013) Myoinositol supplementation in pregnancies at risk for gestational diabetes. Interim analysis of a randomized controlled trial (RCT). Am J Obstet Gynecol 208(1):S36 (ISN: 0002-9378)
Malvasi A, Casciaro F, Minervini MM, Kosmas I, Mynbaev OA, Pacella E, MontiCondesnitt V, Creanza A, Di Renzo GC, Tinelli A (2014) Myo-inositol, d-chiro-inositol, folic acid and manganese in secondtrimester of pregnancy: a preliminaryinvestigation. Eur Rev Med Pharmacol Sci 18(2):270–274
D’Anna R, Scilipoti A, Giordano D, Caruso C, Cannata ML, Interdonato ML, Corrado F, Di Benedetto A (2013) myo-Inositol supplementation and onset of gestational diabetes mellitus in pregnant women with a family history of type 2 diabetes: a prospective, randomized, placebo-controlled study. Diabetes Care 36(4):854–857
DʼAnna R, Di Benedetto A, Scilipoti A, Santamaria A, Interdonato ML, Petrella E, Neri I, Pintaudi B, Corrado F, Facchinetti F (2015) Myo-inositol supplementation for prevention of gestational diabetes in obese pregnant women: a randomized controlled trial. Obstet Gynecol 126(2):310–315
International Association of Diabetes and Pregnancy Study Groups Consensus Panel, Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, Damm P, Dyer AR, Leiva Ad, Hod M, Kitzmiler JL, Lowe LP, McIntyre HD, Oats JJ, Omori Y, Schmidt MI (2010) International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 33(3):676–682
Ferrara A (2007) Increasing prevalence of gestational diabetes mellitus: a public health perspective. Diabetes Care 30(Suppl 2):S141–S146 (Erratum in: Diabetes Care. 2007 Dec;30(12):3154)
Poomalar GK (2015) Changing trends in management of gestational diabetes mellitus. World J Diabetes 6(2):284–295
Rajput M, Bairwa M, Rajput R (2014) Prevalence of gestational diabetes mellitus in rural Haryana: a community-based study. Indian J Endocrinol Metab 18(3):350–354
McCance DR (2011) Pregnancy and diabetes. Best Pract Res Clin Endocrinol Metab 25(6):945–958
Vitagliano A, Quaranta M, Noventa M, Gizzo S (2015) “Empiric” inositol supplementation in normal-weight non insulin resistant women with polycystic ovarian disease: from the absence of benefit to the potential adverse effects. Arch Gynecol Obstet 291(5):955–957
Celentano C, Matarrelli B, Mattei PA, Pavone G, Vitacolonna E, Liberati M (2016) Myo-Inositol supplementation to prevent gestational diabetes mellitus. Curr Diab Rep 16(3):30
Laganà AS, Garzon S, Casarin J, Franchi M, Ghezzi F (2018) Inositol in polycystic ovary syndrome: restoring fertility through a pathophysiology-based approach. Trends Endocrinol Metab 29(11):768–780
Larner J, Craig JW (1996) Urinary myo-inositol-to-chiro-inositol ratios and insulin resistance. Diabetes Care 19(1):76–78
Heimark D, McAllister J, Larner J (2014) Decreased myo-inositol to chiro-inositol (M/C) ratios and increased M/C epimerase activity in PCOS theca cells demonstrate increased insulin sensitivity compared to controls. Endocr J 61(2):111–117 (Epub 2013 Nov 2)
Pundir J, Psaroudakis D, Savnur P, Bhide P, Sabatini L, Teede H, Coomarasamy A, Thangaratinam S (2018) Inositol treatment of anovulation in women with polycystic ovary syndrome: a meta-analysis of randomised trials. BJOG 125(3):299–308
Pintaudi B, Di Vieste G, Bonomo M (2016) The effectiveness of Myo-inositol and d-chiro inositol treatment in type 2 diabetes. Int J Endocrinol 2016:9132052
Laganà AS, Vitagliano A, Noventa M, Ambrosini G, D’Anna R (2018) Myo-inositol supplementation reduces the amount of gonadotropins and length of ovarian stimulation in women undergoing IVF: a systematic review and meta-analysis of randomized controlled trials. Arch Gynecol Obstet 298(4):675–684
Papaleo E, Unfer V, Baillargeon JP, De Santis L, Fusi F, Brigante C, Marelli G, Cino I, Redaelli A, Ferrari A (2007) Myo-inositol in patients with polycystic ovary syndrome: a novel method for ovulation induction. Gynecol Endocrinol 23(12):700–703
Plows JF, Budin F, Andersson RA, Mills VJ, Mace K, Davidge ST, Vickers MH, Baker PN, Silva-Zolezzi I, Stanley JL (2017) The effects of Myo-Inositol and B and D vitamin supplementation in the db/+mouse model of gestational diabetes mellitus. Nutrients. https://doi.org/10.3390/nu9020141
Orrù B, Circo R, Logoteta P, Petousis S, Carlomagno G (2017) Finding the best therapeutic approach for PCOS: the importance of inositol(s) bioavailability. Eur Rev Med Pharmacol Sci 21(2 Suppl):83–88
Funding
None.
Author information
Authors and Affiliations
Contributions
AV: Conceptualization, data curation, formal analysis, investigation, methodology, original draft writing. GS: Investigation, validation, formal analysis original draft writing, review and editing. EC: Supervision, review and editing. SV: Validation, original draft writing, review and editing. FD: Manuscript review and editing. GA: Supervision, validation, review and editing. VB: Conceptualization, project administration, supervision, review and editing
Corresponding author
Ethics declarations
Conflict of interest
Nothing to declare.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Vitagliano, A., Saccone, G., Cosmi, E. et al. Inositol for the prevention of gestational diabetes: a systematic review and meta-analysis of randomized controlled trials. Arch Gynecol Obstet 299, 55–68 (2019). https://doi.org/10.1007/s00404-018-5005-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-018-5005-0