Abstract
Purpose
To study if short-term exposure (2 h and 6 h) of endometrial/endometriotic tissues and cells to 10% seminal plasma (SP) can induce EMT/metaplasia.
Methods
Basic research experimental study was carried out in a University hospital-based fertility center. Semen samples, peritoneal fluid (PF) from endometriosis patients, endometrial biopsy from premenopausal women, immortalized endometriotic epithelial cell line (12Z), and immortalized endometrial stromal cell line (St-T1b) were studied. Rapid stain identification test (RSID), TGFβ1 immunofluorescence of washed sperms, TGFβ1-ELISA of SP and PF, in vitro study (2 h and 6 h incubation) and real-time PCR of endometrial tissue and cell lines to analyze gene expression of EMT/metaplasia markers and mediators were done.
Results
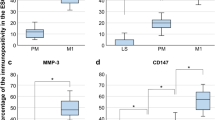
SP is still detectable in washed semen. TGFβ1 was expressed on the plasma membrane of the sperms and was significantly more concentrated in SP (88.17 ng/ml) than PF. 10% SP induced an up-regulation of alpha smooth muscle actin expression in endometrial tissue (p = 0.008) and in 12Z cells (p = 0.05), mostly TGFβ1-independent. TWIST expression was persistently significantly down-regulated while Snail1 and 2 were up-regulated, though insignificant.
Conclusion
Our results provide novel evidence to support that even in semen washed twice, SP is still detectable. The changes in EMT/metaplasia markers and mediators give a new insight into a possible effect of SP on the pathogenesis of endometriosis.





Similar content being viewed by others
References
Mehasseb MK, Bell SC, Pringle JH, Habiba MA (2010) Uterine adenomyosis is associated with ultrastructural features of altered contractility in the inner myometrium. Fertil Steril 93(7):2130–2136. https://doi.org/10.1016/j.fertnstert.2009.01.097
Dunselman GA, Vermeulen N, Becker C, Calhaz-Jorge C, D'Hooghe T, De Bie B, Heikinheimo O, Horne AW, Kiesel L, Nap A, Prentice A, Saridogan E, Soriano D, Nelen W (2014) ESHRE guideline: management of women with endometriosis. Hum Reprod 29(3):400–412. https://doi.org/10.1093/humrep/det457
Omwandho CO, Konrad L, Halis G, Oehmke F, Tinneberg HR (2010) Role of TGF-betas in normal human endometrium and endometriosis. Hum Reprod 25(1):101–109. https://doi.org/10.1093/humrep/dep382
Liu Y, Dong Z, Liu H, Zhu J, Liu F, Chen G (2015) Transition of mesothelial cell to fibroblast in peritoneal dialysis: EMT, stem cell or bystander? Perit Dial Int J Int Soc Perit Dial 35(1):14–25. https://doi.org/10.3747/pdi.2014.00188
De Vriese AS, Tilton RG, Mortier S, Lameire NH (2006) Myofibroblast transdifferentiation of mesothelial cells is mediated by RAGE and contributes to peritoneal fibrosis in uraemia. Nephrol, Dial Transpl 21(9):2549–2555. https://doi.org/10.1093/ndt/gfl271
Bartley J, Julicher A, Hotz B, Mechsner S, Hotz H (2014) Epithelial to mesenchymal transition (EMT) seems to be regulated differently in endometriosis and the endometrium. Arch Gynecol Obstet 289(4):871–881. https://doi.org/10.1007/s00404-013-3040-4
Lv ZD, Na D, Ma XY, Zhao C, Zhao WJ, Xu HM (2011) Human peritoneal mesothelial cell transformation into myofibroblasts in response to TGF-ss1 in vitro. Int J Mol Med 27(2):187–193. https://doi.org/10.3892/ijmm.2010.574
Matsuzaki S, Darcha C (2012) Epithelial to mesenchymal transition-like and mesenchymal to epithelial transition-like processes might be involved in the pathogenesis of pelvic endometriosis. Hum Reprod 27(3):712–721. https://doi.org/10.1093/humrep/der442
Miano JM, Olson EN (1996) Expression of the smooth muscle cell calponin gene marks the early cardiac and smooth muscle cell lineages during mouse embryogenesis. J Biol Chem 271(12):7095–7103
Catteau X, Simon P, Noel JC (2014) Myofibroblastic stromal reaction and lymph node status in invasive breast carcinoma: possible role of the TGF-beta1/TGF-betaR1 pathway. BMC Cancer 14:499. https://doi.org/10.1186/1471-2407-14-499
Hagiwara H, Ohwada N, Aoki T, Suzuki T, Takata K (2008) Immunohistochemical and electron microscopic observations of stromal cells in the human oviduct mucosa. Med Mol Morphol 41(4):221–226. https://doi.org/10.1007/s00795-008-0422-y
Nasu K, Nishida M, Matsumoto H, Bing S, Inoue C, Kawano Y, Miyakawa I (2005) Regulation of proliferation, motility, and contractivity of cultured human endometrial stromal cells by transforming growth factor-beta isoforms. Fertil Steril 84(Suppl 2):1114–1123. https://doi.org/10.1016/j.fertnstert.2005.02.055
Strakova Z, Livak M, Krezalek M, Ihnatovych I (2008) Multipotent properties of myofibroblast cells derived from human placenta. Cell Tissue Res 332(3):479–488. https://doi.org/10.1007/s00441-008-0604-x
Daimon E, Shibukawa Y, Wada Y (2013) Calponin 3 regulates stress fiber formation in dermal fibroblasts during wound healing. Arch Dermatol Res 305(7):571–584. https://doi.org/10.1007/s00403-013-1343-8
Anaf V, Simon P, Fayt I, Noel J (2000) Smooth muscles are frequent components of endometriotic lesions. Hum Reprod 15(4):767–771
Mechsner S, Bartley J, Loddenkemper C, Salomon DS, Starzinski-Powitz A, Ebert AD (2005) Oxytocin receptor expression in smooth muscle cells of peritoneal endometriotic lesions and ovarian endometriotic cysts. Fertil Steril 83(Suppl 1):1220–1231
Itoga T, Matsumoto T, Takeuchi H, Yamasaki S, Sasahara N, Hoshi T, Kinoshita K (2003) Fibrosis and smooth muscle metaplasia in rectovaginal endometriosis. Pathol Int 53(6):371–375
van Kaam KJ, Schouten JP, Nap AW, Dunselman GA, Groothuis PG (2008) Fibromuscular differentiation in deeply infiltrating endometriosis is a reaction of resident fibroblasts to the presence of ectopic endometrium. Hum Reprod 23(12):2692–2700
Sopha SC, Rosado FG, Smith JJ, Merchant NB, Shi C (2015) Hepatic uterus-like mass misdiagnosed as hepatic abscess. Int J Surg Pathol 23(2):134–139. https://doi.org/10.1177/1066896914534465
Flieder DB, Moran CA, Travis WD, Koss MN, Mark EJ (1998) Pleuro-pulmonary endometriosis and pulmonary ectopic deciduosis: a clinicopathologic and immunohistochemical study of 10 cases with emphasis on diagnostic pitfalls. Hum Pathol 29(12):1495–1503
Ibrahim MG, Delarue E, Abesadze E, Haas M, Sehouli J, Chiantera V, Mechsner S (2017) Abdominal wall endometriosis: myofibroblasts as a possible evidence of metaplasia: a case report. Gynecol Obstet Investig 82(1):96–101. https://doi.org/10.1159/000452101
Young VJ, Brown JK, Saunders PT, Duncan WC, Horne AW (2014) The peritoneum is both a source and target of TGF-beta in women with endometriosis. PLoS One 9(9):e106773. https://doi.org/10.1371/journal.pone.0106773
Gazvani R, Templeton A (2002) Peritoneal environment, cytokines and angiogenesis in the pathophysiology of endometriosis. Reproduction 123(2):217–226
Oosterlynck DJ, Meuleman C, Waer M, Koninckx PR (1994) Transforming growth factor-beta activity is increased in peritoneal fluid from women with endometriosis. Obstet Gynecol 83(2):287–292
Zhang Q, Duan J, Liu X, Guo SW (2016) Platelets drive smooth muscle metaplasia and fibrogenesis in endometriosis through epithelial-mesenchymal transition and fibroblast-to-myofibroblast transdifferentiation. Mol Cell Endocrinol 428:1–16. https://doi.org/10.1016/j.mce.2016.03.015
Guo SW, Du Y, Liu X (2016) Platelet-derived TGF-beta1 mediates the down-modulation of NKG2D expression and may be responsible for impaired natural killer (NK) cytotoxicity in women with endometriosis. Hum Reprod 31(7):1462–1474. https://doi.org/10.1093/humrep/dew057
Komiyama S, Aoki D, Komiyama M, Nozawa S (2007) Local activation of TGF-beta1 at endometriosis sites. J Reprod Med 52(4):306–312
Inagaki N, Ung L, Otani T, Wilkinson D, Lopata A (2003) Uterine cavity matrix metalloproteinases and cytokines in patients with leiomyoma, adenomyosis or endometrial polyp. Eur J Obstet Gynecol Reprod Biol 111(2):197–203
Politch JA, Tucker L, Bowman FP, Anderson DJ (2007) Concentrations and significance of cytokines and other immunologic factors in semen of healthy fertile men. Hum Reprod 22(11):2928–2935. https://doi.org/10.1093/humrep/dem281
Robertson SA, Prins JR, Sharkey DJ, Moldenhauer LM (2013) Seminal fluid and the generation of regulatory T cells for embryo implantation. Am J Reprod Immunol 69(4):315–330. https://doi.org/10.1111/aji.12107
Chu TM, Nocera MA, Flanders KC, Kawinski E (1996) Localization of seminal plasma transforming growth factor-beta1 on human spermatozoa: an immunocytochemical study. Fertil Steril 66(2):327–330
Kunz G, Leyendecker G (2002) Uterine peristaltic activity during the menstrual cycle: characterization, regulation, function and dysfunction. Reprod Biomed Online 4(Suppl 3):5–9
Robertson SA (2005) Seminal plasma and male factor signalling in the female reproductive tract. Cell Tissue Res 322(1):43–52. https://doi.org/10.1007/s00441-005-1127-3
Pang BC, Cheung BK (2007) Identification of human semenogelin in membrane strip test as an alternative method for the detection of semen. Forensic Sci Int 169(1):27–31. https://doi.org/10.1016/j.forsciint.2006.07.021
de Lamirande E (2007) Semenogelin, the main protein of the human semen coagulum, regulates sperm function. Semin Thromb Hemost 33(1):60–68. https://doi.org/10.1055/s-2006-958463
Cooper TG, Noonan E, von Eckardstein S, Auger J, Baker HW, Behre HM, Haugen TB, Kruger T, Wang C, Mbizvo MT, Vogelsong KM (2010) World Health Organization reference values for human semen characteristics. Hum Reprod Update 16(3):231–245. https://doi.org/10.1093/humupd/dmp048
Chen JC, Johnson BA, Erikson DW, Piltonen TT, Barragan F, Chu S, Kohgadai N, Irwin JC, Greene WC, Giudice LC, Roan NR (2014) Seminal plasma induces global transcriptomic changes associated with cell migration, proliferation and viability in endometrial epithelial cells and stromal fibroblasts. Hum Reprod 29(6):1255–1270. https://doi.org/10.1093/humrep/deu047
Schuring AN, Schulte N, Kelsch R, Ropke A, Kiesel L, Gotte M (2011) Characterization of endometrial mesenchymal stem-like cells obtained by endometrial biopsy during routine diagnostics. Fertil Steril 95(1):423–426. https://doi.org/10.1016/j.fertnstert.2010.08.035
Zeitvogel A, Baumann R, Starzinski-Powitz A (2001) Identification of an invasive, N-cadherin-expressing epithelial cell type in endometriosis using a new cell culture model. Am J Pathol 159(5):1839–1852. https://doi.org/10.1016/S0002-9440(10)63030-1
Samalecos A, Reimann K, Wittmann S, Schulte HM, Brosens JJ, Bamberger AM, Gellersen B (2009) Characterization of a novel telomerase-immortalized human endometrial stromal cell line, St-T1b. Reprod Biol Endocrinol RB&E 7:76. https://doi.org/10.1186/1477-7827-7-76
Pizzo A, Salmeri FM, Ardita FV, Sofo V, Tripepi M, Marsico S (2002) Behaviour of cytokine levels in serum and peritoneal fluid of women with endometriosis. Gynecol Obst Investig 54(2):82–87. https://doi.org/10.1159/000067717
Hocevar BA, Brown TL, Howe PH (1999) TGF-beta induces fibronectin synthesis through a c-Jun N-terminal kinase-dependent, Smad4-independent pathway. EMBO J 18(5):1345–1356. https://doi.org/10.1093/emboj/18.5.1345
Smith BN, Bhowmick NA (2016) Role of EMT in metastasis and therapy resistance. J Clin Med 5(2):17. https://doi.org/10.3390/jcm5020017
Khan KN, Kitajima M, Hiraki K, Fujishita A, Sekine I, Ishimaru T, Masuzaki H (2010) Effect of human seminal fluid on the growth of endometrial cells of women with endometriosis. Eur J Obst Gynecol Reprod Biol 149(2):204–209. https://doi.org/10.1016/j.ejogrb.2009.12.022
Acknowledgements
We would like to thank Professor Anna Starzinski-Powitz for supplying the 12Z cell line and Dr. Birgit Gellersen for supplying the St-T1b cell line. Moreover, we appreciate the valuable technical assistance by Mrs. Birgit Pers in the gynecology laboratory and the medical technicians in the andrology laboratory at the Center of Reproductive Medicine and Andrology (CeRA) during the whole study.
Author information
Authors and Affiliations
Contributions
MGI study design, data analysis, manuscript drafting, and critical discussion. EA statistical analysis and critical discussion. SS, SK and LK manuscript editing and critical discussion. MV RSID test execution, interpretation, and manuscript critical discussion. MGI, SS and SK, ANS samples collection. MG and ANS shared in the study design, manuscript editing and critical discussion.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
All patients included in this study gave written informed consent. The study was approved by the local research and ethics committee of the medical faculty and the regional medical board of Westfalen, Münster (1 IX Greb).
Electronic supplementary material
Below is the link to the electronic supplementary material.
404_2018_4965_MOESM1_ESM.docx
Supplementary figure (1): Immunostaining of the 12Z cell line. The epithelial cells express cytokeratin (middle panel) and vimentin (lower panel) but no ASMA (upper panel). Supplementary figure (2): Immunostaining of the St-T1b cell line. The stromal cells express vimentin (lower panel) but neither cytokeratin (middle panel) nor ASMA (upper panel) (DOCX 180 kb)
Rights and permissions
About this article
Cite this article
Ibrahim, M.G., Elghonaimy, E.A., Schäfer, S. et al. Seminal plasma (SP) induces a rapid transforming growth factor beta 1 (TGFβ1)—independent up-regulation of epithelial–mesenchymal transdifferentiation (EMT) and myofibroblastic metaplasia-markers in endometriotic (EM) and endometrial cells. Arch Gynecol Obstet 299, 173–183 (2019). https://doi.org/10.1007/s00404-018-4965-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-018-4965-4