Abstract
Purpose
Disorders related to pelvic floor include urinary incontinence (UI), anal incontinence, pelvic organ prolapse, sexual dysfunction and pelvic pain. Because pelvic floor dysfunctions (PFD) can be diagnosed clinically, imaging techniques serve as auxiliary tools for establishing an accurate diagnosis. The objective is to evaluate the PFD in primiparous women after vaginal delivery and the association between clinical examination and three-dimensional ultrasonography (3DUS).
Methods
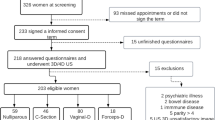
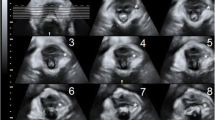
A cross-sectional study was conducted in a in tertiary maternity. All primiparous women with vaginal deliveries that occurred between January 2013 and December 2015 were invited. Women who attended the invitation underwent detailed anamnesis, questionnaire application, physical examination and endovaginal and endoanal 3DUS. Crude and adjusted predictor factors for PFD were analyzed.
Results
Fifty women were evaluated. Sexual dysfunction was the most prevalent PFD (64.6%). When associated with clinical features and PFD, oxytocin use increased by approximately four times the odds of UI (crude OR 4.182, 95% CI 1.149–15.219). During the multivariate analysis, the odds of UI were increased in forceps use by approximately 11 times (adjusted OR 11.552, 95% CI 11.155–115.577). When the clinical and obstetrical predictors for PFD were associated with 3DUS, forceps increased the odds of lesion of the pubovisceral muscle and anal sphincter diagnosed by 3DUS by sixfold (crude OR 6.000, 95% CI 1.172–30.725), and in multivariate analysis forceps again increased the odds of injury by approximately 7 times (adjusted OR 7.778, 95% CI 1.380–43.846).
Conclusion
Sexual dysfunction was the most frequent PFD. The use of forceps in primiparous women was associated with a greater chance of UI and pelvic floor muscle damage diagnosed by 3DUS.


Similar content being viewed by others
References
Dietz HP, Simpson JM (2008) Levator trauma is associated with pelvic organ prolapse. Bjog Int J Obstet Gynaecol 115(8):979–984
Bazi T, Takahashi S, Ismail S, Bo K, Ruiz-Zapata AM, Duckett J et al (2016) Prevention of pelvic floor disorders: international urogynecological association research and development committee opinion. Int Urogynecol J 27(12):1785–1795
Bo K, Frawley HC, Haylen BT, Abramov Y, Almeida FG, Berghmans B et al (2017) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Neurourol Urodyn 36(2):221–244
Volloyhaug I, van Gruting I, van Delft K, Sultan AH, Thakar R (2016) Is bladder neck and urethral mobility associated with urinary incontinence and mode of delivery 4 years after childbirth? Neurourol Urodyn 24(10):23123. https://doi.org/10.1002/nau.23123
Monteiro MVD, Pereira GMV, Aguiar RAP, Azevedo RL, Correia MD, Reis ZSN (2016) Risk factors for severe obstetric perineal lacerations. Int Urogynecol J 27(1):61–67
Mejido JAG, Mejias PV, Palacín AF, Barby MJB, De la Fuente Vaquero P, Bueno JAS (2017) Evaluation of isolatedurinary stress incontinence according to the type of levator ani muscle lesion using 3/4D transperineal ultrasound 36 months post-partum. Int Urogynecol J 28(7):1019–1026
Jármy-Di Bella ZIK, Júnior EA, Rodrigues CA, Torelli L, Martins WP, Moron AF et al (2016) Reproducibility in pelvic floor biometric parameters of nulliparous women assessed by translabial three-dimensional ultrasound using Omniview reformatting technique. Med Ultrasonogr 18(3):345–350
Guzman Rojas R, Shek K, Langer S, Dietz H (2013) Prevalence of anal sphincter injury in primiparous women. Ultrasound Obstet Gynecol 42(4):461–466
Dietz HP (2009) Pelvic floor assessment. Fetal Matern Med Rev 20(1):49–66
Thiel Rdo R, Dambros M, Palma PC, Thiel M, Riccetto CL, Ramos Mde F (2008) Translation into Portuguese, cross-national adaptation and validation of the Female Sexual Function Index. Rev Bras Ginecol Obstet 30(10):504–510
Edition F (2013) Diagnostic and statistical manual of mental disorders. Am Psychiatr Assoc
Wiegel M, Meston C, Rosen R (2005) The Female Sexual Function Index (FSFI): cross-validation and development of clinical cutoff scores. J Sex Marital Ther 31(1):1–20
Laycock J (1994) Female pelvic floor assessment: the Laycock ring of continence. J Natl Women Health Group Aust Physiother Assoc 1994:40–51
Haylen BT, Maher CF, Barber MD, Camargo S, Dandolu V, Digesu A et al (2016) Erratum to: an International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic organ prolapse (POP). Int Urogynecol J 27(4):655–684
Thom DH, Brown JS, Schembri M, Ragins AI, Creasman JM, Van Den Eeden SK (2011) Parturition events and risk of urinary incontinence in later life. Neurourol Urodyn 30(8):1456–1461
Casey BM, Schaffer JI, Bloom SL, Heartwell SF, McIntire DD, Leveno KJ (2005) Obstetric antecedents for postpartum pelvic floor dysfunction. Am J Obstet Gynecol 192(5):1655–1662
Svare JA, Hansen BB, Lose G (2014) Risk factors for urinary incontinence 1 year after the first vaginal delivery in a cohort of primiparous Danish women. Int Urogynecol J 25(1):47–51
Karahan N, Arslan H, Çam Ç (2018) The behaviour of pelvic floor muscles during uterine contractions in spontaneous and oxytocin-induced labour. J Obstet Gynaecol 2018:1–6
Meyer S, Schreyer A, De Grandi P, Hohlfeld P (1998) The effects of birth on urinary continence mechanisms and other pelvic-floor characteristics. Obstet Gynecol 92(4 Pt 1):613–618
DeLancey JO, Miller JM, Kearney R, Howard D, Reddy P, Umek W et al (2007) Vaginal birth and de novo stress incontinence: relative contributions of urethral dysfunction and mobility. Obstet Gynecol 110(2 Pt 1):354–362
DeLancey JOL, Kearney R, Chou Q, Speights S, Binno S (2003) The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol 101(1):46–53
Foldspang A, Hvidman L, Mommsen S, Bugge Nielsen J (2004) Risk of postpartum urinary incontinence associated with pregnancy and mode of delivery. Acta Obstet Gynecol Scand 83(10):923–927
Hannestad YS, Rortveit G, Sandvik H, Hunskaar S (2000) A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT Study. J Clin Epidemiol 53(11):1150–1157
DeLancey JO, Kearney R, Chou Q, Speights S, Binno S (2003) The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol 101(1):46–53
MacArthur C, Wilson D, Herbison P, Lancashire RJ, Hagen S, Toozs-Hobson P et al (2016) Urinary incontinence persisting after childbirth: extent, delivery history, and effects in a 12-year longitudinal cohort study. BJOG Int J Obstet Gynaecol 123(6):1022–1029
Dietz HP, Steensma AB (2006) The prevalence of major abnormalities of the levator ani in urogynaecological patients. BJOG 113(2):225–230
Murad-Regadas SM, Fernandes GOD, Regadas FSP, Rodrigues LV, Pereira JDR, Dealcanfreitas ID (2014) Assessment of pubovisceral muscle defects and levator hiatal dimensions in women with faecal incontinence after vaginal delivery: is there a correlation with severity of symptoms? Colorectal Dis 16(12):1010–1018
Varma A, Gunn J, Gardiner A, Lindow SW, Duthie GS (1999) Obstetric anal sphincter injury: prospective evaluation of incidence. Dis Colon Rectum 42(12):1537–1543
Dietz HP, Shek C (2008) Levator avulsion and grading of pelvic floor muscle strength. Int Urogynecol J Pelvic Floor Dysfunct 19(5):633–636
Kearney R, Miller JM, Delancey JO (2006) Interrater reliability and physical examination of the pubovisceral portion of the levator ani muscle, validity comparisons using MR imaging. Neurourol Urodyn 25(1):50–54
Dietz HP, Mann KP (2014) What is clinically relevant prolapse? An attempt at defining cutoffs for the clinical assessment of pelvic organ descent. Int Urogynecol J 25(4):451–455
Kahramanoglu I, Baktiroglu M, Hamzaoglu K, Kahramanoglu O, Verit FF, Yucel O (2017) The impact of mode of delivery on the sexual function of primiparous women: a prospective study. Arch Gynecol Obstet 295(4):907–916
Meriwether KV, Rogers RG, Dunivan GC, Alldredge JK, Qualls C, Migliaccio L et al (2016) Perineal body stretch during labor does not predict perineal laceration, postpartum incontinence, or postpartum sexual function: a cohort study. Int Urogynecol J 27(8):1193–1200
Wallwiener S, Müller M, Doster A, Kuon RJ, Plewniok K, Feller S et al (2017) Sexual activity and sexual dysfunction of women in the perinatal period: a longitudinal study. Arch Gynecol Obstet 295(4):873–883
Menees SB, Smith TM, Xu X, Chey WD, Saad RJ, Fenner DE (2013) Factors associated with symptom severity in women presenting with fecal incontinence. Dis Colon Rectum 56(1):97–102
O’Mahony F, Hofmeyr GJ, Menon V (2010) Choice of instruments for assisted vaginal delivery. Cochrane Database Syst Rev. 11:Cd005455
Dietz HP (2015) Forceps: towards obsolescence or revival? Acta Obstet Gynecol Scand 94(4):347–351
Acknowledgements
We would like to acknowledge the members of the Department of Obstetrics and Gynaecology, Medical Informatics and Surgery of the Hospital das Clínicas of Federal University of Minas Gerais for the support to this research. We thank all the primiparous women who participated in the study.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
GMV Pereira—protocol/project development, data collection or management, data analysis and manuscript writing/editing. MVC Monteiro—protocol/project development, data collection or management and manuscript writing/editing. ZSN Reis—protocol/project development, data analysis and manuscript writing/editing. BDS Rodrigues, KCLR Buzatti and MC Cruz—data collection or management.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The research project was approved by the Research Ethics Committee of the Federal University of Minas Gerais (UFMG) (CAAE: 42099115.3.0000.5149—26 March 2015).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pereira, G.M.V., Reis, Z.S.N., Rodrigues, B.D. et al. Association between pelvic floor dysfunction, and clinical and ultrasonographic evaluation in primiparous women: a cross-sectional study. Arch Gynecol Obstet 298, 345–352 (2018). https://doi.org/10.1007/s00404-018-4811-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-018-4811-8