Abstract
Purpose
The purpose of this study was to test for differences between patient-reported outcome measures (PROMs) at 1 and 2 years following total hip (THA) or knee (TKA) arthroplasty.
Methods
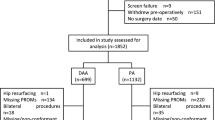
Between 2015 and 2016, n = 469 and n = 414 patients underwent THA and TKA, respectively. Demographic and PROMs data were collected at 1 and 2 years post-operatively. PROMs included Veterans Rand 12-item (VR-12), Hip Injury and Osteoarthritis Outcomes Score (HOOS) Pain subscore, HOOS-Physical Function Short-form (HOOS-PS), Knee Injury and Osteoarthritis Outcomes Score (KOOS) Pain subscore, and KOOS-Physical Function Short-form (KOOS-PS). Paired t tests assessed differences between groups. N = 298 (65.8%) and n = 240 (64%) patients followed-up at 1 year, and 205 (72% of 1-year responders) and 174 (76%) at 2 years in the THA and TKA cohorts, respectively.
Results
No statistically significant differences were observed between 1 and 2 years for HOOS pain (p = 0.445), HOOS-PS (p = 0.265), VR-12 PCS (p = 0.239), VR-12 MCS scores (p = 0.342) in THA and TKA cohorts [KOOS pain (p = 0.242), KOOS-PS (p = 0.088), VR-12 PCS (p < 0.2757), VR-12 MCS scores (p < 0.075)]. There were statistically significant baseline differences between responders and non-responders (patients lost to follow-up), but differences were small and not clinically relevant. PROMs were not significantly different between 1- and 2-year time points for THA and TKA. Minimal demographic or baseline differences between responders and non-responders suggest a representative sample.
Conclusion
These data support a minimum follow-up of 1 year for studies with PROMs as the primary outcome variable following THA and TKA.

Similar content being viewed by others
References
Cizmic Z, Novikov D, Feng J, Iorio R, Meftah M (2019) Alternative payment models in total joint arthroplasty under the affordable care act. JBJS Rev 7(3):e4. https://doi.org/10.2106/JBJS.RVW.18.00061
Squitieri L, Bozic KJ, Pusic AL (2017) The role of patient-reported outcome measures in value-based payment reform. Value Heal 20(6):834–836. https://doi.org/10.1016/j.jval.2017.02.003
Zusman EE (2012) Hcahps replaces press ganey survey as quality measure for patient hospital experience. Neurosurgery 71(2):N21–N24. https://doi.org/10.1227/01.neu.0000417536.07871.ed
Ramkumar PN, Navarro SM, Haeberle HS, Ng M, Piuzzi NS, Spindler KP (2018) No difference in outcomes 12 and 24 months after lower extremity total joint arthroplasty: a systematic review and meta-analysis. J Arthroplasty 33(7):2322–2329. https://doi.org/10.1016/j.arth.2018.02.056
Samuelsson K, Magnussen RA, Alentorn-Geli E et al (2017) Equivalent knee injury and osteoarthritis outcome scores 12 and 24 months after anterior cruciate ligament reconstruction: results from the swedish national knee ligament register. Am J Sports Med 45(9):2085–2091. https://doi.org/10.1177/0363546517702871
Lyman S, Lee YY, McLawhorn AS, Islam W, MacLean CH (2018) What are the minimal and substantial improvements in the HOOS and KOOS and JR versions after total joint replacement? ClinOrthopRelat Res 476(12):2432–2441. https://doi.org/10.1097/CORR.0000000000000456
Rolfson O, Bohm E, Franklin P et al (2016) Patient-reported outcome measures in arthroplasty registries: Report of the patient-reported outcome measures working group of the international society of arthroplasty registries Part II. Recommendations for selection, administration, and analysis. Acta Orthop. 87:9–23. https://doi.org/10.1080/17453674.2016.1181816
Cleveland O, Piuzzi NS, Strnad G et al (2019) Implementing a scientifically valid, cost-effective, and scalable data collection system at point of care: the cleveland clinic OME cohort. J Bone Joint Surg Am 101:458–464. https://doi.org/10.2106/JBJS.18.00767
Piuzzi NS, Strnad GJ, SakrEsa WA, Barsoum WK, Bloomfield MR, Brooks PJ, Higuera-Rueda CA, Joyce MJ, Kattan MW, Klika AA, Krebs V, Mesko NW, Mont MA, Murray TG, Muschler GF, Nickodem RJ, Patel PD, Schaffer JL, Spindler KP, Stearns KL, Suarez JC, Zajichek A (2019) The main predictors of length of stay after total knee arthroplasty: patient-related or procedure-related risk factors. J Bone Joint Surg Am 101(12):1093–1101. https://doi.org/10.2106/JBJS.18.00758
Kazis LF, Miller DR, Clark JA et al (2004) Improving the response choices on the veterans SF-36 health survey role functioning scales: Results from the veterans health study. J Ambul Care Manage 27(3):263–280. https://doi.org/10.1097/00004479-200407000-00010
Kazis LE, Miller DR, Skinner KM et al (2006) Applications of methodologies of the veterans health study in the VA healthcare system: conclusions and summary. J Ambul Care Manage 29(2):182–188. https://doi.org/10.1097/00004479-200604000-00011
Klässbo M, Larsson E, Mannevik E (2003) Hip disability and osteoarthritis outcome score: An extension of the western ontario and mcmaster universities osteoarthritis index. Scand J Rheumatol 32(1):46–51. https://doi.org/10.1080/03009740310000409
Davis AM, Perruccio AV, Canizares M et al (2009) Comparative, validity and responsiveness of the HOOS-PS and KOOS-PS to the WOMAC physical function subscale in total joint replacement for Osteoarthritis. OsteoarthrCartil 17(7):843–847. https://doi.org/10.1016/j.joca.2009.01.005
Boston University School of Public Health. VR-36, VR-12 and VR-6D. Boston: Boston University; Available at: https://www.bu.edu/sph/about/departments/health-law-policy-and-management/research/vr-36-vr-12-and-vr-6d/ Accessed May 20, 2019
Centers for Medicare & Medicaid Services. Health Outcomes Survey (HOS). Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/HOS/index.html Accessed May 20, 2019
Patient-Reported Outcomes Summit for Total Joint Arthroplasty Report (2015) Double Tree by Hilton Baltimore North-Pikesville (August 31. J Arthroplast 30:1860–1862
Nilsdotter A, Bremander A (2011) Measures of hip function and symptoms: harris hip score (HHS), hip disability and osteoarthritis outcome score (HOOS), oxford hip score (OHS), lequesne index of severity for osteoarthritis of the hip (LISOH), and american academy of orthopedic surgeons. Arthritis Care Res 63(S11):S200–S207. https://doi.org/10.1002/acr.20549
Centers for Medicare & Medicaid Services. Measure Methodology. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html. Accessed May 20, 2019
Roos H, Laurén M, Adalberth T, Roos EM, Jonsson K, Lohmander LS (1998) Knee osteoarthritis after meniscectomy: prevalence of radiographic changes after twenty-one years, compared with matched controls. Arthritis Rheum 41(4):687–693. https://doi.org/10.1002/1529-0131(199804)41:4%3c687::AID-ART16%3e3.0.CO;2-2
Roos EM, Toksvig-Larsen S (2003) Knee injury and osteoarthritis outcome score (KOOS) - Validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes 1:17. https://doi.org/10.1186/1477-7525-1-17
Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM (2011) Measures of knee function: international knee documentation committee (IKDC) subjective knee evaluation form, knee injury and osteoarthritis outcome score (KOOS), knee injury and osteoarthritis outcome score physical function short form (KOOS-PS). Knee Ou Arthritis Care Res 63(S11):S208–S228. https://doi.org/10.1002/acr.20632
Reinholdsson J, Kraus-Schmitz J, Forssblad M, Edman G, Byttner M, Stålman A (2017) A non-response analysis of 2-year data in the Swedish Knee Ligament Register. Knee Surg Sport TraumatolArthrosc 25(8):2481–2487. https://doi.org/10.1007/s00167-015-3969-x
Rahr-Wagner L, Thillemann TM, Lind MC, Pedersen AB (2013) Validation of 14,500 operated knees registered in the danish knee ligament reconstruction register: Registration completeness and validity of key variables. ClinEpidemiol 5:219–228. https://doi.org/10.2147/CLEP.S45752
Holve CD, Segal PD, Franklin DC et al (2016) Incorporating patient-reported outcomes into health care to engage patients and enhance care. Health Aff 35(4):575–582. https://doi.org/10.1377/hlthaff.2015.1362
Acknowledgements
The Cleveland Clinic OME Arthroplasty Group consists of: Marcelo BP Siqueira, MDa; Peter A Surace, MDa; Wael K. Barsoum, MDa; Isaac Briskin, MAb; Carlos A Higuera Rueda, MDa; Atul F. Kamath, MDa; Alison K Klika, MSa; Melissa N Orr, BSa ; Brian M Leo, MDc; Preetesh D. Patel, MDa; Jordan Patterson, BSd; Kurt P Spindler, MDe; Amy Shuster, BSd; Gregory J Strnad, MSe; Juan Suarez, MDc, Robert Zaas, BAf; Nicolas S Piuzzi, MDa. aCleveland Clinic Department of Orthopaedic Surgery, 9500 Euclid Avenue, Cleveland, OH 44195, USA. bCleveland Clinic Department of Quantitative Health Sciences, 9620 Carnegie Avenue, Cleveland, OH 44106. cCleveland Clinic Florida, 2950 Cleveland Clinic Blvd. Weston, FL 33331, USA. dOhio University Heritage College of Osteopathic Medicine, 35 W Green Dr, Athens, OH 45701 USA. eCleveland Clinic Orthopaedic Sports Health, 5555 Transportation Blvd., Garfield Heights, OH 44125 USA. fCase Western Reserve University School of Medicine, 10900 Euclid Ave., Cleveland, OH 44106 USA. Thank you to the Cleveland Clinic orthopaedic patients, staff, and research personnel whose efforts related to regulatory, data collection, subject follow-up, data quality control, analyses, and manuscript preparation have made this consortium successful. Also thank you to Brittany Stojsavljevic, editor assistant, Cleveland Clinic Foundation, with editorial management.
Funding
There is no funding source.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Dr. Bogliolo Piancastelli Siqueira has nothing to disclose. Dr. Surace has nothing to disclose. Dr. Barsoum reports personal fees from DJO, personal fees from Stryker, personal fees from Zimmer, personal fees from Orthosensor, other from Custom Orthopaedic Solutions, other from PeerWell, other from Capsico Health, personal fees from Exactech, personal fees from Arthrex, other from Beyond Limits, other from Sight Medical, other from PT Genie, outside the submitted work. Mr. Briskin reports personal fees from CHEST Journal, outside the submitted work. Dr. Higuera reports grants from Stryker, grants and personal fees from KCI, grants from Ferring Pharmaceuticals, grants from CD Diagnostics, grants from OREF, grants from Orthofix, grants from Lyfstoine, grants from Zimmer Biomet, outside the submitted work. Dr. Kamath reports personal fees and other from DePuy Synthes, personal fees and other from Zimmer Biomet, outside the submitted work. Ms. Klika has nothing to disclose. Ms. Orr has nothing to disclose. Dr. Leo reports other from Zimmer Biomet, outside the submitted work. Dr. Patel reports personal fees from Stryker, personal fees from Zimmer-Biomet, outside the submitted work. Mr. Patterson has nothing to disclose. Dr. Spindler reports grants from NIH/NIAMS R01 AR053684, grants from NIH/NIAMS R01 AR074131, grants from NIH/NIAMS R01 AR075422-01, other from NFL, other from Service Excellence, other from Mitek, other from Flexion Therapeutics, other from Samumed, other from Novopeds, outside the submitted work. Ms. Shuster has nothing to disclose. Mr. Strnad has nothing to disclose. Dr. Suarez reports other from Corin USA, other from Depuy Orthopedics, outside the submitted work. Mr. Zaas has nothing to disclose. Dr. Piuzzi reports other from ISCT, other from Orthopaedic Research Society, other from Zimmer, outside the submitted work.
Ethical approval
This study was approved under Cleveland Clinic IRB #06-196.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of Cleveland Clinic O. M. E. Arthroplasty Group are list in acknowledgements.
Rights and permissions
About this article
Cite this article
Piuzzi, N.S., Cleveland Clinic O. M. E. Arthroplasty Group. Patient-reported outcomes at 1 and 2 years after total hip and knee arthroplasty: what is the minimum required follow-up?. Arch Orthop Trauma Surg 142, 2121–2129 (2022). https://doi.org/10.1007/s00402-021-03819-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03819-x