Abstract
Purpose
The purpose of this study was to investigate the effects of sequential medial release on the stiffness and collateral stability of the ligament complex of the knee. Irrespective of the implantation technique used, varus deformity frequently requires release of the capsular ligament complex. Yet, no data are available on how stiffness and stability of the knee ligament complex are weakened by such release.
Methods
After total knee arthroplasty, ten healthy Thiel-fixed knee joints were subjected to sequential medial release consisting of six release steps. After each step, stiffness and stability were determined at 0°, 30°, 60°, and 90°.
Results
Sequential medial release increasingly weakened the ligament complex. In extension, release of the anteromedial tibial sleeve 4 cm below the joint line already weakened the ligament complex by approximately 13%. Release 6 cm below the joint line reduced stiffness and stability by 15–20% over the entire range of motion. After detachment of the medial collateral ligament, stability was only about 60% of its initial value.
Conclusion
Our study showed for the first time the association between medial release and stiffness and stability of the knee ligament complex. To maintain stability, vigorous detachment of the knee ligament complex should be avoided. Release of the anteromedial tibial sleeve already initiates loss of stability. The main stabiliser is the medial ligament, which should never be completely detached.
Level of evidence
IV.
Similar content being viewed by others
Introduction
The prerequisite for successful total knee arthroplasty is optimal postoperative kinematics coupled with stable ligament guidance over the full range of motion [10, 21]. In addition to surgical exposure of the knee joint, which should always be as cautious as possible, a medial release is required in 78% (Aunan et al.), 76% (Whiteside et al.), and 88% (Griffin et al.) of varus deformities; thus, medial release represents a standard intraoperative mode of balancing [2, 7, 21]. Various soft-tissue techniques have been described in the literature [4, 8,9,10,11,12, 14, 19, 21]. For instance, Whiteside et al. detached the dorsal or anterior parts of the medial collateral ligament (MCL) from the tibia in a targeted manner depending on the extension or flexion contracture, whereas Lee et al. gradually released the MCL at the femoral insertion of the ligament [11, 21]. Other studies describe balancing of the knee by means of the pie-crusting technique or by sequential release [4, 8, 9, 13, 14, 19]. However, although each technique results in balanced extension and flexion gap, the common denominator of all studies is the lack of an examination how the capsular ligament complex is weakened by release. We assumed that the knee ligament complex is weakened by any type of release, which—depending on the extent—may lead to secondary instability.
Purpose and hypothesis
We hypothesised that medial release weakens the knee ligament complex and that over-release may lead to secondary instability. Therefore, we conducted sequential medial release as a part of total knee arthroplasty and determined the stiffness and stability of the knee ligament complex at 0°, 30°, 60°, and 90°. The study clearly showed the stage at which instability occurs.
Materials and methods
Cadaver specifications
In the current study, we used unhurt full body preparation of Thiel-embalmed specimens. We examined the stability in five left and five right knee joints. None of the knees showed any deformity, and none of the specimens had previously received surgery on the lower extremities. At the time of examination, the knee joints were clinically stable. All knees and hip joints had a full range of motion. The mean leg axis was 171.8° ± 1.7°, the anatomical lateral distal femur angle (aLDFA) 79.2° ± 1.8°, the anatomical medial proximal tibia angle (aMPTA) 87.7° ± 1.8° and the joint line convergence angle (JLCA) 1.8° ± 1.7°.
Surgical technique and in vitro measurements
Force–elongation curves were determined during our standard surgical routine for total knee arthroplasty. First, a mid-line skin incision was made, and the capsule was opened according to the medial parapatellar approach, followed by the resection of the anterior cruciate ligament and the menisci. 2 Schanz screws were bicortically drilled into the femur and tibial plateau outside the joint capsule to avoid soft-tissue damage. Subsequently, the passive optical reference arrays were fixed (Brainlab AG, Munich, Germany). According to the navigation workflow, the femoral head centre was determined by circumduction. Anatomical landmarks on the tibia and femur were identified by means of a pointer (femoral: distal femoral knee centre, medial and lateral epicondyle, Whiteside line, articulating surface of the medial and lateral condyle; tibial: tibial plateau size, medial and lateral malleolus, Akagi line as tibial AP axis and the articulating surface of the medial and lateral tibial plateau). Leg alignments were recorded in full extension and in 90° flexion. According to our standard surgical routine, the tibial slope was set to 4° posterior slope, and the tibial cutting jig was aligned according to the recommendation of the navigation system perpendicular to the mechanical axis of the tibia. The jig was fixed, and the tibial cut was made, removing 8 mm of bone and cartilage of the healthy lateral compartment. The collateral ligaments were thereby protected by retractors. After removal of the jig, the cut was verified, and the femur was prepared. The distal cut was made perpendicular to the femoral mechanical axis. Femoral rotation was set to an external rotation of 3°. During each preparation step, damage to the knee ligament complex was carefully avoided. A femoral trail component (Depuy PFC Sigma cruciate retaining, Depuy, Warsaw, IN, USA) was firmly inserted and mediolaterally centred with optimal coverage of the femoral bone. The knee balancer was placed into the extension gap between the tibia and femur. The leg was straightened, and a preload of about 10–20 N was applied to the medial and lateral ligament complex. The medial and lateral ligament complex was slowly spread up to 180 N. The expansion was recorded on video. The videos were evaluated after surgery. The procedure was repeated in 30°, 60°, and 90° flexion. Knee flexion was adjusted with a continuous passive motion device and monitored with the navigation system. Sequential release was performed stepwise, and measurements were carried out as described below and repeated twice. Arthroplasty was performed by one surgeon with 10 years of surgical experience.
Sequential medial soft-tissue release
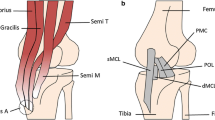
The method of sequential medial release was modified according to the recommendations by Matsueda et al. [14]. Medial release consisted of six successive steps. The structures were subperiosteally or subligamentously released with a scalpel or a Cobb elevator (Fig. 1):
-
1.
release of the anteromedial tibial sleeve 2 cm below the joint line;
-
2.
release of the tibial attachment of the semimembranosus muscle;
-
3.
release of the anteromedial tibial sleeve 4 cm below the joint line;
-
4.
release of the anteromedial tibial sleeve 6 cm below the joint line;
-
5.
release of the medial collateral ligament from the femoral condyle;
-
6.
release of the entire posterior cruciate ligament on the tibial side.
Reconstruction of the force–elongation curve
The force–elongation curve was reconstructed with the ‘knee balancer’ (P.F.C Sigma and LCS Complete EGF Instrumentation of Depuy Synthes, Warsaw, USA), which displays the applied force and elongation at all times. The balancer had been validated prior to the study.
For evaluation, the videos were read into Matlab (Mathworks, Natick, USA), and every tenth frame was extracted. The applied force and the elongation of the capsular ligaments were calculated by means of the frames. The force–elongation curve was obtained by plotting the current force against the elongation. The slope of the linear section (from approximately 80 N) of the force–elongation curve was defined as the stiffness of the ligament complex and represented the structural properties. The slope, box plots, and 3D plots were calculated in Excel (Microsoft Corp. Redmond, USA). For calculating stability, the mean value of stiffness was set to 100% at the native (unreleased) knee joint. Decreased stability as a result of the release refers to the respective native value at 0°, 30°, 60°, and 90°.
Statistical analysis
For statistical analysis, measurements are presented as box plots. Group comparisons were done with the Mann–Whitney U test because of the non-normal distribution of the data. The primary hypothesis was tested at a two-sided 5% significance level. IBM SPSS Statistics 23 (SPSS Inc, Chicago, IL, USA) was used for analysis.
Results
Tables 1 and 2 show the summary of mean stiffness and interquartile range depending on knee joint flexion and release steps. Figure 2 shows stiffness as a function of release for the medial (A–D) and lateral (E–H) compartments. Figure 3 depicts the 3D plots of stability for the medial compartment and Fig. 4 for the lateral compartment.
Stiffness of the medial (blue, a full extension, b 30° flexion, c 60° flexion, and d 90° flexion) and lateral (green, e full extension, f 30° flexion, g 60° flexion, and h 90° flexion) compartment depending on the release of the medial knee ligament complex. In the medial compartment, stiffness decreases with increasing release, whereas stiffness at the lateral compartment remains the same. *p < 0.05, **p < 0.01
Medial compartment
Stiffness successively decreases with increasing release, but a highly significant drop is only observed after detaching the medial collateral ligament and the posterior cruciate ligament. Stability of the medial compartment is not reduced by release of the anteromedial tibial sleeve 2 cm below the joint line and the tibial insertion of the semimembranosus muscle. Release of the tibial sleeve 4 cm below the joint line weakens the ligament complex by approximately 13% in extension only. After release of the tibial sleeve 6 cm below the joint line, stability drops by 15–20% over the entire range of motion. After detachment of the medial collateral ligament, stability is only about 60% of the initial value (see Table 1, Figs. 2, 3).
Lateral compartment
Release of the medial ligament complex does not initially affect the stability of the lateral compartment; only release of the medial collateral ligament leads to non-significant loss of stiffness and stability of up to 25%. Release of the posterior cruciate ligament does not lead to further substantial weakening of the knee ligament complex (see Table 2, Figs. 2, 4).
Discussion
The most important findings of the present study were that detachment of the anterior tibial sleeve already leads to loss of stiffness and that detachment of the medial collateral ligament leads to a significant decrease in stiffness and thus to loss of stability of the knee joint over the entire range of motion. This is the first study showing the association between sequential medial release and stiffness and stability of the knee ligament complex and the only study determining the stiffness of the entire knee joint. Therefore, the results of this study cannot be compared with the findings of other studies, but may primarily be discussed on the basis of anatomical considerations.
In the medial compartment, anteromedial detachment of the tibial sleeve 2 cm below the joint capsule did not change stiffness or stability of the knee ligament complex (see Table 1, Figs. 2, 3). This finding may be explained by the fact that, at 2 cm below the joint line, only small parts of the capsule and deep medial collateral ligament were detached [5, 10, 15]. Large parts of the joint capsule and the superficial medial collateral ligament remain untouched, thus providing maximum stability. Therefore, no loss of stiffness can be observed.
Detachment of the semimembranosus muscle does also not affect stiffness of the knee ligament complex (see Table 1, Figs. 2, 3), which is not surprising, because muscles in the cadaveric knee are relaxed without providing stability, also in the native state. In vivo, the semimembranosus muscle is a dynamic stabiliser of the knee joint that depends on muscle tension [5, 15].
Initial weakening of stability (even if not significant) can be measured in full extension after release of the anteromedial tibial sleeve 4 cm below the joint line (see Table 1, Figs. 2, 3). In consideration of the anatomy, release leads to the detachment of additional parts of the joint capsule, the medial retinaculum as well as the proximal parts of the superficial medial collateral ligament [21]. The anteromedial capsule should, therefore, only be released far enough to be able to access the knee joint.
These findings are all the more important, because we were able to show that even detachment of the anteromedial capsule 6 cm below the joint line leads to loss of stiffness and destabilisation by 15–20% over the entire range of motion (see Table 1, Figs. 2, 3). Anatomically, anterior proximal parts of the superficial medial collateral ligament are also detached. According to Whiteside et al., particularly, the anterior proximal parts of the ligament stabilise the knee joint during flexion [21]. Whiteside et al. were able to show that release of these parts of the ligament leads to a significant change in the leg axis, especially at 60° and 90° flexion. This finding corresponds to our results.
Complete release of the medial collateral ligament leads to residual stability of only about 60% of the initial value (see Table 1, Figs. 2, 3). Stiffness of the joint is also reduced, especially in extension, as well as in 90° flexion. Lüring et al. and Matsueda and al. were able to show a significant change in the leg axis and gaps after the release of the medial collateral ligament in full extension and 90° flexion [12,13,14]. The superficial medial collateral ligament should, therefore, be regarded as the main passive stabiliser of the medial compartment over the entire range of motion.
However, our study did not show any further loss of stiffness or stability after release of the posterior cruciate ligament (see Table 1, Figs. 2, 3). Lüring et al. and Matsueda and al. reported a significant change in the leg axis and gaps after release of the posterior cruciate ligament [12,13,14] which also has to be a load-bearing passive stabiliser. Accordingly, a change in stiffness and stability should also occur in this ligament. This finding can only be explained by the fact that the remaining structures such as the lateral collateral ligament or posterolateral ligament structures have the same stiffness as the posterior cruciate ligament.
The lateral compartment did not show any loss of stiffness or stability over the first four steps of the release (see Table 2, Figs. 2, 4), which was to be expected, because the primary lateral stabilisers such as the lateral collateral ligament or the iliotibial band remain intact. Only after detachment of the entire medial collateral ligament did stiffness and stability decrease by about 20–25% in relation with the initial value. According to the findings of Lüring et al., a clear opening of the knee joint gap is clinically visible at the medial joint space as well as at the lateral compartment [13]. The change in stiffness and stability at the lateral joint gap in this release step is thus not surprising.
Our study showed that sequential medial release increasingly weakens the knee ligament complex. However, the results themselves are difficult to transfer to other release forms or other sequential release sequences. The loss of stiffness and thus stability in another sequence of the release is bound to be different. Especially, in the pie-crusting technique, loss of stiffness and stability depends on the location, number, and depth of the punctures. Standardised procedures are hardly possible in this context. Nevertheless, we suggest that detachment of the anteromedial tibial sleeve leads to a first weakening of the knee ligament complex and that the medial collateral ligament is the most important stabiliser for collateral ligament stability at the inside of the knee.
As noted above, no work has yet been published on the stiffness of the entire knee joint, but some publications have determined the stiffness of separate ligaments [16, 17, 22, 24]. When examining the medial collateral ligament complex of cadaveric knees, Robinson et al. found a stiffness value of 80.0 ± 8 Nm m−1 for the superficial ligament complex and 42.0 ± 14 Nm m−1 for the deep medial collateral ligament complex [16]. Sugita et al. described a stiffness value of 58.1 ± 22.8 Nm m−1 (range 26.0–83.0 Nm m−1) for the lateral collateral ligament in ten cadaveric knees [17]. In the current study, median stiffness in full extension was 27.75 Nm m−1 (IQR 16.81 Nm m−1) for the medial compartment and 28.14 Nm m−1 (IQR 12.73 Nm m−1) for the lateral compartment (Tables 1, 2). However, stiffness values of separate ligaments were higher than those in the current study. The reasons for this difference may be very complex. Thus, the present study determined the stiffness of the entire knee joint. The direction of the tensile force can, therefore, not be aligned with the ligament structures itself, but may only be examined in different joint positions. The fibres of the individual ligaments always run transversely to the direction of the tensile force, which reduces stiffness values [15, 17]. Another reason could be that Thiel-fixed whole-body preparations were used in the current study, which are characterised by their lifelike histological structure, colour, and ligament consistency [18]. Nevertheless, biomechanical properties can be falsified through fixation [6]. In principle, Wilke et al. were able to demonstrate biomechanical comparability with regard to the non-linear load-deformation characteristic of spinal motion segments in comparison to tests with fresh frozen cadaver. However, flexibility was increased [23]. In a separate study on the ligamentous properties of the knee joints, Völlner et al. did not find any significant differences to intraoperative comparative measurements in vivo [20].
Another effect on stiffness, especially on the lateral compartment, might be the patellar eversion during preparation of the knee joint and determination of stiffness. Aunan et al. showed a minimal effect on the ligament laxity (condylar lift-off) in flexion of 0.6 mm with the patella repositioned compared to everted [3]. No differences were found in extension or medially in flexion. They themselves estimate the influence of patella eversion on ligament laxity as too small to be clinically relevant. Nevertheless, the eversion could have an influence on the stiffness. However, data on this cannot be found in the literature.
This study has several limitations. The first limitation is the small number of ten knee joints. According to Audigé et al., a sample size of at least ten is required for analysing a new method [1]. A further limitation of the study is the use of knees without any deformity, which is also similar to other studies [13, 14, 21]. However, the effect of the described release sequence may differ from the clinical situation. We are, therefore, conducting a study on the effect of sequential release in knees with varus deformities in vivo. Furthermore, it should be noted that only passive stabilisers such as ligaments and capsule portions were recorded in our study. No active stabilisation by the knee joint musculature was detected, a factor that we estimate to be very high in vivo. Furthermore, our examination only represents a snapshot. The healing process and scarring after total knee arthroplasty may further alter stiffness and stability of the knee. The knee balancer only enables extension of the knee ligament complex up to a force of 180 N per side. Further extension would be desirable to be able to determine the slope of the linear region over a larger area. On the other hand, further extension could damage the knee ligament complex. In our view, further extension is not absolutely necessary because of the presence of a linear region of the force–extension curve in every measurement.
Conclusion
Release of the anteromedial tibial sleeve 4 cm below the joint line leads to a first decrease in stiffness and loss of stability in extension. During preparation for total knee arthroplasty, the capsule should only be released so far as to gain access to the knee joint. Release of the medial collateral ligament results in a significant decrease in stiffness and in a 40% loss of stability over the entire range of motion. The medial collateral ligament should, therefore, never be released completely.
References
Audigé L, Bhandari M, Kellam J (2004) How reliable are reliability studies of fracture classifications? A systematic review of their methodologies. Acta Orthop Scand 75:184–194
Aunan E, Kibsgård T, Clarke-Jenssen J, Röhrl SM (2012) A new method to measure ligament balancing in total knee arthroplasty: laxity measurements in 100 knees. Arch Orthop Trauma Surg 132:1173–1181
Aunan E, Kibsgård T, Röhrl SM (2017) Minimal effect of patella eversion on ligament balancing in cruciate-retaining total knee arthroplasty. Arch Orthop Trauma Surg 137:387–392
Bellemans J, Vandenneucker H, Van Lauwe J, Victor J (2010) A new surgical technique for medial collateral ligament balancing. J Arthroplasty 25:1151–1156
Beltran J, Matityahu A, Hwang K, Jbara M, Maimon R, Padron M, Mota J, Beltran L, Sundaram M (2003) The distal semimembranosus complex: normal MR anatomy, variants, biomechanics and pathology. Skelet Radiol 32:435–445
Fessel G, Frey K, Schweizer A, Calcagni M, Ullrich O, Snedeker JG (2011) Suitability of Thiel embalmed tendons for biomechanical investigation. Ann Anat Anat Anz 193:237–241
Griffin FM, Insall JN, Scuderi GR (2000) Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty 15:970–973
He X, Cai H, Zhang K (2018) Pie-crusting technique is effective and safe to release superficial medial collateral ligament for total knee arthroplasty. J Orthop Transl 13:33–40
Herschmiller T, Grosso MJ, Cunn GJ, Murtaugh TS, Gardner TR, Geller JA (2017) Step-wise medial collateral ligament needle puncturing in extension leads to a safe and predictable reduction in medial compartment pressure during TKA. Knee Surg Sports Traumatol Arthrosc 26(6):1759–1766
Hunt NC, Ghosh KM, Athwal KK, Longstaff LM, Amis AA, Deehan DJ (2014) Lack of evidence to support present medial release methods in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:3100–3112
Lee S-Y, Yang J-H, Lee Y-I, Yoon J-R (2016) A novel medial soft tissue release method for varus deformity during total knee arthroplasty: femoral origin release of the medial collateral ligament. Knee Surg Relat Res 28:153–160
Luring C, Bäthis H, Hüfner T, Grauvogel C, Perlick L, Grifka J (2006) Gap configuration and anteroposterior leg axis after sequential medial ligament release in rotating-platform total knee arthroplasty. Acta Orthop 77:149–155
Luring C, Hüfner T, Perlick L, Bäthis H, Krettek C, Grifka J (2006) The effectiveness of sequential medial soft tissue release on coronal alignment in total knee arthroplasty. J Arthroplasty 21:428–434
Matsueda M, Gengerke TR, Murphy M, Lew WD, Gustilo RB (1999) Soft tissue release in total knee arthroplasty: cadaver study using knees without deformities. Clin Orthop 366:264
Pedersen R (2016) The medial and posteromedial ligamentous and capsular structures of the knee: review of anatomy and relevant imaging findings. Semin Musculoskelet Radiol 20:012–025
Robinson JR, Bull AM, Amis AA (2005) Structural properties of the medial collateral ligament complex of the human knee. J Biomech 38:1067–1074
Sugita T, Amis AA (2001) Anatomic and biomechanical study of the lateral collateral and popliteofibular ligaments. Am J Sports Med 29:466–472
Thiel W (1992) The preservation of the whole corpse with natural color. Ann Anat Anat Anz Off Organ Anat Ges 174:185–195
Verdonk PCM, Pernin J, Pinaroli A, Selmi TAS, Neyret P (2009) Soft tissue balancing in varus total knee arthroplasty: an algorithmic approach. Knee Surg Sports Traumatol Arthrosc 17:660–666
Völlner F, Pilsl U, Craiovan B, Zeman F, Schneider M, Wörner M, Grifka J, Weber M (2017) Stability of knee ligament complex of Thiel-embalmed cadaver compared to in vivo knee. J Mech Behav Biomed Mater 71:392–396
Whiteside LA, Saeki K, Mihalko WM (2000) Functional medical ligament balancing in total knee arthroplasty. Clin Orthop Relat Res 380:45–57
Wijdicks CA, Ewart DT, Nuckley DJ, Johansen S, Engebretsen L, LaPrade RF (2010) Structural properties of the primary medial knee ligaments. Am J Sports Med 38:1638–1646
Wilke H-J, Werner K, Häussler K, Reinehr M, Böckers TM (2011) Thiel-fixation preserves the non-linear load-deformation characteristic of spinal motion segments, but increases their flexibility. J Mech Behav Biomed Mater 4:2133–2137
Wilson WT, Deakin AH, Payne AP, Picard F, Wearing SC (2012) Comparative analysis of the structural properties of the collateral ligaments of the human knee. J Orthop Sports Phys Ther 42:345–351
Acknowledgements
The authors thank Professor Friedrich Anderhuber (Institute of Anatomy at the Medical University of Graz, Austria) for providing the specimens for this investigation. The authors thank Martin Bauer and his team (Brainlab, Feldkirchen, Germany) for providing the navigation devices and the detailed information on the processed data. Furthermore, we thank Monika Schöll for the linguistic review of our manuscript.
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
According to the local ethical committee, no approval was necessary.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Völlner, F., Fischer, J., Weber, M. et al. Weakening of the knee ligament complex due to sequential medial release in total knee arthroplasty. Arch Orthop Trauma Surg 139, 999–1006 (2019). https://doi.org/10.1007/s00402-019-03181-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-019-03181-z