Abstract
Purpose
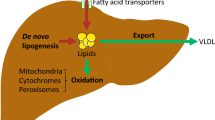
In obesity and diabetes the liver is highly susceptible to abnormal uptake and storage of fat. In certain individuals hepatic steatosis predisposes to the development of non-alcoholic steatohepatitis (NASH), a disease marked by hepatic inflammation and fibrosis. Although the precise pathophysiology of NASH is unknown, it is believed that the gut microbiota-liver axis influences the development of this disease. With few treatment strategies available for NASH, exploration of gut microbiota-targeted interventions is warranted. We investigated the therapeutic potential of a prebiotic supplement to improve histological parameters of NASH.
Methods
In a placebo-controlled, randomized pilot trial, 14 individuals with liver-biopsy-confirmed NASH [non-alcoholic fatty liver activity score (NAS) ≥ 5] were randomized to receive oligofructose (8 g/day for 12 weeks followed by 16 g/day for 24 weeks) or isocaloric placebo for 9 months. The primary outcome measure was the change in liver biopsy NAS score and the secondary outcomes included changes in body weight, body composition, glucose tolerance, inflammatory markers, and gut microbiota.
Results
Independent of weight loss, oligofructose improved liver steatosis relative to placebo and improved overall NAS score (P = 0.016). Bifidobacterium was enhanced by oligofructose, whereas bacteria within Clostridium cluster XI and I were reduced with oligofructose (P < 0.05). There were no adverse side effects that deterred individuals from consuming oligofructose for treatment of this disease.
Conclusions
Independent of other lifestyle changes, prebiotic supplementation reduced histologically-confirmed steatosis in patients with NASH. Larger follow-up studies are warranted.
Clinical Trial
This trial was registered at Clinicaltrials.com as NCT03184376.



Similar content being viewed by others
References
Rinella ME (2015) Non-alcoholic fatty liver disease. JAMA 313(22):2263–2273. https://doi.org/10.1001/jama.2015.5370
Yilmaz Y, Younossi ZM (2014) Obesity-associated non-alcoholic fatty liver disease. Clin Liver Dis 18(1):19–31. https://doi.org/10.1016/j.cld.2013.09.018
Anderson EL, Howe LD, Jones HE, Higgins JP, Lawlor DA, Fraser A (2015) The prevalence of non-alcoholic fatty liver disease in children and adolescents: a systematic review and meta-analysis. PLoS One 10(10):e0140908. https://doi.org/10.1371/journal.pone.0140908
Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L, Torres-Gonzalez A, Gra-Oramas B, Gonzalez-Fabian L, Friedman SL, Diago M, Romero-Gomez M (2015) Weight loss through lifestyle modification significantly reduces features of non-alcoholic steatohepatitis. Gastroenterology 149(2):367–378.e365. https://doi.org/10.1053/j.gastro.2015.04.005
Dudekula A, Rachakonda V, Shaik B, Behari J (2014) Weight loss in non-alcoholic fatty liver disease patients in an ambulatory care setting is largely unsuccessful but correlates with frequency of clinic visits. PLoS One 9(11):e111808. https://doi.org/10.1371/journal.pone.0111808
Tilg H, Moschen AR (2010) Evolution of inflammation in non-alcoholic fatty liver disease: the multiple parallel hits hypothesis. Hepatology 52(5):1836–1846. https://doi.org/10.1002/hep.24001
de Faria Ghetti F, Oliveira DG, de Oliveira JM, de Castro Ferreira L, Cesar DE, Moreira APB (2018) Influence of gut microbiota on the development and progression of non-alcoholic steatohepatitis. Eur J Nutr 57(3):861–876. https://doi.org/10.1007/s00394-017-1524-x
Moschen AR, Kaser S, Tilg H (2013) Non-alcoholic steatohepatitis: a microbiota-driven disease. Trends Endocrinol Metab 24(11):537–545. https://doi.org/10.1016/j.tem.2013.05.009
Nieuwdorp M, Gilijamse PW, Pai N, Kaplan LM (2014) Role of the microbiome in energy regulation and metabolism. Gastroenterology 146(6):1525–1533. https://doi.org/10.1053/j.gastro.2014.02.008
Le Roy T, Llopis M, Lepage P, Bruneau A, Rabot S, Bevilacqua C, Martin P, Philippe C, Walker F, Bado A, Perlemuter G, Cassard-Doulcier AM, Gerard P (2013) Intestinal microbiota determines development of non-alcoholic fatty liver disease in mice. Gut 62(12):1787–1794. https://doi.org/10.1136/gutjnl-2012-303816
Brandl K, Schnabl B (2017) Intestinal microbiota and non-alcoholic steatohepatitis. Curr Opin Gastroenterol 33(3):128–133. https://doi.org/10.1097/mog.0000000000000349
Gibson GR, Hutkins R, Sanders ME, Prescott SL, Reimer RA, Salminen SJ, Scott K, Stanton C, Swanson KS, Cani PD, Verbeke K, Reid G (2017) Expert consensus document: the International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat Rev Gastroenterol Hepatol 14(8):491–502. https://doi.org/10.1038/nrgastro.2017.75
Corradini C, Lantano C, Cavazza A (2013) Innovative analytical tools to characterize prebiotic carbohydrates of functional food interest. Anal Bioanal Chem 405(13):4591–4605. https://doi.org/10.1007/s00216-013-6731-6
Mokhtari Z, Gibson DL, Hekmatdoost A (2017) Non-alcoholic fatty liver disease, the gut microbiome, and diet. Adv Nutr 8:240–252. https://doi.org/10.3945/an.116.013151
Parnell JA, Raman M, Rioux KP, Reimer RA (2012) The potential role of prebiotic fibre for treatment and management of non-alcoholic fatty liver disease and associated obesity and insulin resistance. Liver Int 32(5):701–711. https://doi.org/10.1111/j.1478-3231.2011.02730.x
Dewulf EM, Cani PD, Claus SP, Fuentes S, Puylaert PG, Neyrinck AM, Bindels LB, de Vos WM, Gibson GR, Thissen JP, Delzenne NM (2013) Insight into the prebiotic concept: lessons from an exploratory, double blind intervention study with inulin-type fructans in obese women. Gut 62(8):1112–1121. https://doi.org/10.1136/gutjnl-2012-303304
Daubioul CA, Horsmans Y, Lambert P, Danse E, Delzenne NM (2005) Effects of oligofructose on glucose and lipid metabolism in patients with non-alcoholic steatohepatitis: results of a pilot study. Eur J Clin Nutr 59(5):723–726. https://doi.org/10.1038/sj.ejcn.1602127
Kellow NJ, Coughlan MT, Reid CM (2014) Metabolic benefits of dietary prebiotics in human subjects: a systematic review of randomised controlled trials. Br J Nutr 111(7):1147–1161. https://doi.org/10.1017/S0007114513003607
Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, Ferrell LD, Liu YC, Torbenson MS, Unalp-Arida A, Yeh M, McCullough AJ, Sanyal AJ, Non-alcoholic Steatohepatitis Clinical Research N (2005) Design and validation of a histological scoring system for non-alcoholic fatty liver disease. Hepatology 41(6):1313–1321. https://doi.org/10.1002/hep.20701
Bruhwyler J, Carreer F, Demanet E, Jacobs H (2009) Digestive tolerance of inulin-type fructans: a double-blind, placebo-controlled, cross-over, dose-ranging, randomized study in healthy volunteers. Int J Food Sci Nutr 60(2):165–175. https://doi.org/10.1080/09637480701625697
Godin G, Shephard RJ (1985) A simple method to assess exercise behavior in the community. Can J Appl Sport Sci 10(3):141–146
Fujii H, Kawada N (2012) Inflammation and fibrogenesis in steatohepatitis. J Gastroenterol 47(3):215–225. https://doi.org/10.1007/s00535-012-0527-x
Levy JC, Matthews DR, Hermans MP (1998) Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care 21(12):2191–2192
DeFronzo RA, Matsuda M (2010) Reduced time points to calculate the composite index. Diabetes Care 33(7):e93. https://doi.org/10.2337/dc10-0646
Bomhof MR, Paul HA, Geuking MB, Eller LK, Reimer RA (2016) Improvement in adiposity with oligofructose is modified by antibiotics in obese rats. FASEB J 30(8):2720–2732. https://doi.org/10.1096/fj.201600151R
Nicolucci AC, Hume MP, Martinez I, Mayengbam S, Walter J, Reimer RA (2017) Prebiotics reduce body fat and alter intestinal microbiota in children who are overweight or with obesity. Gastroenterology 153(3):711–722. https://doi.org/10.1053/j.gastro.2017.05.055
McMurdie PJ, Holmes S (2013) phyloseq: an R package for reproducible interactive analysis and graphics of microbiome census data. PLoS One 8(4):e61217. https://doi.org/10.1371/journal.pone.0061217
Love MI, Huber W, Anders S (2014) Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol 15(12):550. https://doi.org/10.1186/s13059-014-0550-8
Malaguarnera M, Vacante M, Antic T, Giordano M, Chisari G, Acquaviva R, Mastrojeni S, Malaguarnera G, Mistretta A, Li Volti G, Galvano F (2012) Bifidobacterium longum with fructo-oligosaccharides in patients with non alcoholic steatohepatitis. Dig Dis Sci 57(2):545–553. https://doi.org/10.1007/s10620-011-1887-4
Eslamparast T, Poustchi H, Zamani F, Sharafkhah M, Malekzadeh R, Hekmatdoost A (2014) Synbiotic supplementation in non-alcoholic fatty liver disease: a randomized, double-blind, placebo-controlled pilot study. Am J Clin Nutr 99(3):535–542. https://doi.org/10.3945/ajcn.113.068890
Aller R, De Luis DA, Izaola O, Conde R, Gonzalez Sagrado M, Primo D, De La Fuente B, Gonzalez J (2011) Effect of a probiotic on liver aminotransferases in non-alcoholic fatty liver disease patients: a double blind randomized clinical trial. Eur Rev Med Pharmacol Sci 15(9):1090–1095
Vajro P, Mandato C, Licenziati MR, Franzese A, Vitale DF, Lenta S, Caropreso M, Vallone G, Meli R (2011) Effects of Lactobacillus rhamnosus strain GG in pediatric obesity-related liver disease. J Ped Gastroenterol Nutr 52(6):740–743. https://doi.org/10.1097/MPG.0b013e31821f9b85
Wong VW, Won GL, Chim AM, Chu WC, Yeung DK, Li KC, Chan HL (2013) Treatment of non-alcoholic steatohepatitis with probiotics. A proof-of-concept study. Ann Hepatol 12(2):256–262
Bomhof MR, Saha DC, Reid DT, Paul HA, Reimer RA (2014) Combined effects of oligofructose and Bifidobacterium animalis on gut microbiota and glycemia in obese rats. Obesity 22(3):763–771. https://doi.org/10.1002/oby.20632;10.1002/oby.20632
Promrat K, Kleiner DE, Niemeier HM, Jackvony E, Kearns M, Wands JR, Fava JL, Wing RR (2010) Randomized controlled trial testing the effects of weight loss on non-alcoholic steatohepatitis. Hepatology 51(1):121–129. https://doi.org/10.1002/hep.23276
Morel FB, Dai Q, Ni J, Thomas D, Parnet P, Fanca-Berthon P (2015) Alpha-galacto-oligosaccharides dose-dependently reduce appetite and decrease inflammation in overweight adults. J Nutr 145(9):2052–2059. https://doi.org/10.3945/jn.114.204909
Parnell JA, Reimer RA (2009) Weight loss during oligofructose supplementation is associated with decreased ghrelin and increased peptide YY in overweight and obese adults. Am J Clin Nutr 89(6):1751–1759. https://doi.org/10.3945/ajcn.2009.27465
Daud NM, Ismail NA, Thomas EL, Fitzpatrick JA, Bell JD, Swann JR, Costabile A, Childs CE, Pedersen C, Goldstone AP, Frost GS (2014) The impact of oligofructose on stimulation of gut hormones, appetite regulation and adiposity. Obesity 22(6):1430–1438. https://doi.org/10.1002/oby.20754
Ryan MC, Itsiopoulos C, Thodis T, Ward G, Trost N, Hofferberth S, O’Dea K, Desmond PV, Johnson NA, Wilson AM (2013) The Mediterranean diet improves hepatic steatosis and insulin sensitivity in individuals with non-alcoholic fatty liver disease. J Hepatol 59(1):138–143. https://doi.org/10.1016/j.jhep.2013.02.012
Zhu L, Baker SS, Gill C, Liu W, Alkhouri R, Baker RD, Gill SR (2013) Characterization of gut microbiomes in non-alcoholic steatohepatitis (NASH) patients: a connection between endogenous alcohol and NASH. Hepatology 57(2):601–609. https://doi.org/10.1002/hep.26093
Mouzaki M, Comelli EM, Arendt BM, Bonengel J, Fung SK, Fischer SE, McGilvray ID, Allard JP (2013) Intestinal microbiota in patients with non-alcoholic fatty liver disease. Hepatology 58(1):120–127. https://doi.org/10.1002/hep.26319
Kalliomaki M, Carmen Collado M, Salminen S, Isolauri E (2008) Early differences in fecal microbiota composition in children may predict overweight. Am J Clin Nutr 87(3):534–538. https://doi.org/10.1093/ajcn/87.3.534
Ratziu V, Charlotte F, Heurtier A, Gombert S, Giral P, Bruckert E, Grimaldi A, Capron F, Poynard T, Group LS (2005) Sampling variability of liver biopsy in non-alcoholic fatty liver disease. Gastroenterology 128(7):1898–1906. https://doi.org/10.1053/j.gastro.2005.03.084
Trabulsi J, Schoeller DA (2001) Evaluation of dietary assessment instruments against doubly labeled water, a biomarker of habitual energy intake. Am J Physiol Endo Metab 281(5):E891–899. https://doi.org/10.1152/ajpendo.2001.281.5.E891
Helmerhorst HJ, Brage S, Warren J, Besson H, Ekelund U (2012) A systematic review of reliability and objective criterion-related validity of physical activity questionnaires. Int J Behav Nutr Phys Act 9:103. https://doi.org/10.1186/1479-5868-9-103
Kaczmarek JL, Musaad SM, Holscher HD (2017) Time of day and eating behaviors are associated with the composition and function of the human gastrointestinal microbiota. Am J Clin Nutr 106(5):1220–1231. https://doi.org/10.3945/ajcn.117.156380
Acknowledgements
The authors would like to thank all of the individuals who volunteered their time to participate and contribute to this study. The authors also thank Matt Workentine, Faculty of Veterinary Medicine, University of Calgary, for his technical assistance with 16S sequencing analysis.
Funding
This work was supported by a research grant from the Canadian Institutes of Health Research (MOP-136889) and a University of Calgary Seed Grant. MRB was supported by Alberta Innovates Health Solutions (AIHS) and an Honorary Izaak Walton Killam Doctoral Scholarship.
Author information
Authors and Affiliations
Contributions
MRB executed the study, collected data, analyzed data, and prepared the manuscript; JAP designed the study and obtained funding; HRR analyzed 16S gut microbiota sequencing data; PC collected data; KPR, SJ, and MR designed the study, collected data, and recruited participants; CSP performed VOC analysis; RAR designed the study, obtained funding and had final responsibility for the study. All authors had access to the study data and reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
MRB, JAP, HRR, PC, KPR, CSP, SJ, and MR declare no conflict of interest. RAR previously held a research grant from Beneo-Orafti, Inc., manufacturer of Orafti P95, for a project unrelated to this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bomhof, M.R., Parnell, J.A., Ramay, H.R. et al. Histological improvement of non-alcoholic steatohepatitis with a prebiotic: a pilot clinical trial. Eur J Nutr 58, 1735–1745 (2019). https://doi.org/10.1007/s00394-018-1721-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-018-1721-2