Abstract
Background
In practice, warfarin-treated patients may share insight regarding their international normalized ratio (INR) value before it is measured. The accuracy and potential utility of these predictions have not been evaluated.
Objective
To (1) test how accurately patients can predict their INR; (2) identify demographic factors associated with their ability to predict their INR accurately; and (3) identify demographic factors associated with the patient’s INR being in the therapeutic range.
Methods
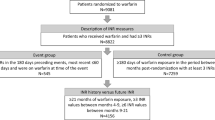
A prospective, multi-center cohort study enrolled patients from eight anticoagulation clinics in Iowa. Inclusion criteria were: age ≥ 18 years, warfarin use ≥ 60 days, INR goal of 2.0–3.0, and expected warfarin use > 6 months. Subjects completed a data collection form during enrollment and before each INR measurement. Data included demographics, a set of medication taking beliefs and practices, self-reported adherence, past INR values, INR prediction and reason(s) for the prediction.
Results
There were 87 subjects enrolled with 372 INR measurements. The mean (SD) number of INRs per subject was 4.3 (1.8). Thirty percent of subjects reported they could tell when their INR is out of goal range. Patients predicted that 90.5% of their INRs would be within goal range, although only 65.5% of INRs were therapeutic. Patients correctly predicted a low INR as low or high INR as high in only 9.4% of out of range instances. A set of demographic characteristics and medication beliefs were not associated with prediction accuracy or percentage of INR measurements in range (PINRR). Most patients did not give a reason for their predicted result. For those that did, the most common factor was perceived stability at current dose.
Conclusion
While some patients believed they could predict when their INR was out of range, only few were able to do so. Most patients assumed a therapeutic INR and missed when their INR was high or low. Patients should be advised against modifying their warfarin dose without consulting the provider that manages their therapy.
Trial registration
ClinicalTrials.gov number, NCT 02764112.
Similar content being viewed by others
Notes
The Adherence Estimator is a registered trademark of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA. Copyright © 2008 Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc. All rights reserved.
References
Wysowski DK, Nourjah P, Swartz L (2007) Bleeding complications with warfarin use: a prevalent adverse effect resulting in regulatory action. Arch Intern Med 167(13):1414–1419. https://doi.org/10.1001/archinte.167.13.1414
Food and Drug Administration approves updated warfarin (coumadin) prescribing information. https://wayback.archive-it.org/7993/20170113091731/http:/www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2007/ucm108967.htm. Accessed 20 Apr 2018
Ageno W, Gallus AS, Wittkowsky A, Crowther M, Hylek EM, Palareti G (2012) Oral anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. CHEST 141(2 Suppl):e44S–e88S. https://doi.org/10.1378/chest.11-2292
Proietti M, Nobili A, Raparelli V, Napoleone L, Mannucci PM, Lip GY (2016) Adherence to antithrombotic therapy guidelines improves mortality among elderly patients with atrial fibrillation: insights from the REPOSI study. Clin Res Cardiol 105(11):912–920. https://doi.org/10.1007/s00392-016-0999-4 PMID: 27245329
Skeppholm M, Friberg L (2014) Adherence to warfarin treatment among patients with atrial fibrillation. Clin Res Cardiol 103(12):998–1005. https://doi.org/10.1007/s00392-014-0742-y
Connolly SJ, Pogue J, Eikelboom J, Flaker G, Commerford P, Franzosi MG, Healey JS, Yusuf S (2008) Benefit of oral anticoagulant over antiplatelet therapy in atrial fibrillation depends on the quality of international normalized ratio control achieved by centers and countries as measured by time in therapeutic range. Circulation 118:2029–2037. https://doi.org/10.1161/CIRCULATIONAHA.107.750000
Cannegieter SC, Rosendaal FR, Wintzen AR, van der Meer FJM, Vandenbrouchhke JP, Briet E (1995) Optimal oral anticoagulant therapy in patients with mechanical heart valves. N Engl J Med 333(1):11–17. https://doi.org/10.1056/NEJM199507063330103
Biskupiak J, Ghate SR, Jiao T, Brixner D (2013) Cost implications of formulary discussions on oral anticoagulants in nonvalvular atrial fibrillation. J Manag Care Pharm 19(9):789–798. https://doi.org/10.18553/jmcp.2013.19.9.789
Holbrook A, PSchulman S, Witt DM, Vandvik PO, Fish J, Kovacs MJ, Svensson PJ, Veenstra DL, Crowther M, Guyatt GH. Evidence-based management of anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012;141(2 Suppl):e152s–e184s. https://doi.org/10.1378/chest.11-2295
Freeman JV, Zhu RP, Owens DK, Garber AM, Hutton DW, Go AS, Wang PJ, Turakhia MP (2011) Cost-effectiveness of dabigatran compared with warfarin for stroke prevention in atrial fibrillation. Ann Intern Med 154(1):1–11. https://doi.org/10.7326/0003-4819-154-1-201101040-00289
Lee S, Mullin R, Blazawski J, Coleman, Cl (2012) Cost-effectiveness of apixaban compared with warfarin for stroke prevention in atrial fibrillation. PLoS One 7(10):e47473. https://doi.org/10.1371/journal.pone.0047473
McEvoy GK (ed) (2018) AHFS: drug information. American Society of Health-System Pharmacists, Besthesda
Aronson JK (2016) Vitamin K analogues. In: Aronson JK (ed) Meyler’s side effects of drugs, 16th edn. Elsevier Science, Amsterdam, pp 494–499
Mc Horney CA (2009) The adherence estimator: a brief, proximal screener for patient propensity to adhere to prescription medications for chronic disease. Curr Med Res Opin 25(1):215–238. https://doi.org/10.1185/03007990802619425
Rosendaal FR, Cannegieter SC, Van Der Meer FJM, Briet E (1993) A method to determine the optimal intensity of oral anticoagulant therapy. Thromb Haemost 69:236–239
Chan PH, Li WH, Hai JJ, Chan EW, Wong IC, Tse HF, Lip GY, Siu CW. Time in therapeutic range and percentage of international normalized ratio in the therapeutic range as a measure of quality of anticoagulation control in patients with atrial fibrillation. Can J Cardiol 2016;32(10):1247.e23–1247.e28. https://doi.org/10.1016/j.cjca.2015.10.029
Pokorney SD, Simon DN, Thomas L, Gersh BJ, Hylek EM, Piccini JP, Peterson ED (2016) Stability of international normalized ratios in patients taking long-term warfarin therapy. JAMA 316(6):661–663. https://doi.org/10.1001/jama.2016.9356
Dumas S, Rouleua-Mailloux E, Bouchama N, Lahcene H, Talajic M, Tardif JC, Gaulin MJ, Provost S, Dube MP, Perreault S (2016) Pillbox use and INR stability in a prospective cohort of new warfarin users. J Manag Care Spec Pharm 22(6):676–684. https://doi.org/10.18553/jmcp.2016.22.6.676
Pokorney SD, Simon DN, Thomas L, Fonarow GC, Kowey PR, Chang P, Singer DE, Ansell J, Blanco RG, Gersh B, Mahaffey KW, Hylek EM, Go AS, Piccini JP, Peterson ED (2015) Patients’ time in therapeutic range on warfarin among US patients with atrial fibrillation: results from ORBIT-AF registry. Am Heart J 170(1):141–148. https://doi.org/10.1016/j.ahj.2015.03.017
Oramasionwu CU, Bailey SC, Duffey KE, Shilliday BB, Brown LC, Denslow SA, Michalets EL (2014) The association of health literacy with time in therapeutic range for patients on warfarin therapy. J Health Commun 19(Suppl 2):19–28. https://doi.org/10.1080/10810730.2014.934934
van Walraven C, Jennings A, Oake N, Fergusson D, Forster AJ (2006) Effect of study setting on anticoagulation control: a systematic review and metaregression. Chest 129(5):1155–1166. https://doi.org/10.1378/chest.129.5.1155
Witt DM, Delate T, Clark NP, Martell C, Tran T, Crowther MA, Garcia DA, Ageno W, Hylek EM (2010) Twelve-month outcomes and preditors of very stable INR control in prevalent warfarin users. J Thromb Haemost 8(4):744–749. https://doi.org/10.1111/j.1538-7836.2010.03756.x
Acknowledgements
The authors would like to acknowledge statistical support from Brahmendra Viyyuri.
Author information
Authors and Affiliations
Corresponding author
Additional information
Views expressed in the following article are those of the author(s) and not an official position of institutions involved in this study.
Rights and permissions
About this article
Cite this article
McNamara, K., Witry, M., Bryant, G. et al. A prospective, multi-center cohort study: investigating the ability of warfarin-treated patients to predict their INR. Clin Res Cardiol 108, 212–217 (2019). https://doi.org/10.1007/s00392-018-1345-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-018-1345-9