Abstract
Purpose
Recurrent prolapse of the posterior pelvic organ compartment presents a management challenge, with the best surgical procedure remaining unclear. We present functional outcome and patient satisfaction after laparoscopic and robotic ventral mesh rectopexy (VMR) with biological mesh in patients with recurrence.
Methods
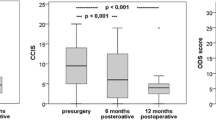
We analyzed data from 30 patients with recurrent posterior pelvic organ prolapse who underwent VMR with biological mesh from August 2012 to January 2018. Data included patient demographics and intra- and postoperative findings; functional outcome as assessed by Cleveland Clinic Constipation Score (CCCS), Obstructed Defecation Score Longo (ODS), and Cleveland Clinic Incontinence Score (CCIS); and patient satisfaction.
Results
CCCS, CCIS, and ODS were significantly improved at 6–12 months postoperatively and at last follow-up. Patient satisfaction (visual analog scale [VAS] 6.7 [0 to 10]), subjective symptoms (+ 3.4 [scale − 5 to + 5]), and quality of life improvement (+ 3.0 [scale from − 5 to + 5]) were high at last follow-up. The rates of morbidity and major complications were 13% and 3%, respectively. There were no mesh-related complications or deaths. Difference in type of previous surgery (abdominal or transanal/perineal) had no significant effect on results.
Conclusions
VMR with biological mesh is a safe and effective option for patients with recurrent posterior pelvic organ prolapse. It reduces functional symptoms, has a low complication rate, and promotes patient satisfaction.

Similar content being viewed by others
References
Xynos E (2012) Functional results after surgery for overt rectal prolapse. Acta Chir Iugosl 59:21–24
Formijne Jonkers HA, Draaisma WA, Wexner SD, Broeders IAMJ, Bemelman WA, Lindsey I, Consten ECJ (2013) Evaluation and surgical treatment of rectal prolapse: an international survey. Color Dis 15(1):115–119
D'Hoore A, Cadoni R, Penninckx F (2004) Long-term outcome of laparoscopic ventral rectopexy for total rectal prolapse. Br J Surg 91(11):1500–1505
van Iersel JJ, Paulides TJ, Verheijen PM et al (2016) Current status of laparoscopic and robotic ventral mesh rectopexy for external and internal rectal prolapse. World J Gastroenterol 22(21):4977–4987
Boons P, Collinson R, Cunningham C, Lindsey I (2010) Laparoscopic ventral rectopexy for external rectal prolapse improves constipation and avoids de novo constipation. Color Dis 12(6):526–532
Solomon MJ, Young CJ, Eyers AA, Roberts RA (2002) Randomized clinical trial of laparoscopic versus open abdominal rectopexy for rectal prolapse. Br J Surg 89(1):35–39
Balla A, Quaresima S, Smolarek S, Shalaby M, Missori G, Sileri P (2017) Synthetic versus biological mesh-related erosion after laparoscopic ventral mesh rectopexy: asystematic review. Ann Coloproctol 33(2):46–51
Smart NJ, Pathak S, Boorman P, Daniels IR (2013) Synthetic or biological mesh use in laparoscopic ventral mesh rectopexy--a systematic review. Color Dis 15(6):650–654
Consten EC, van Iersel JJ, Verheijen PM et al (2015) Along-term outcome after laparoscopic ventral mesh rectopexy: an observational study of 919 consecutive patients. Ann Surg 262:742–747 discussion 747-748
Mackenzie H, Dixon AR (2014) Proficiency gain curve and predictors of outcome for laparoscopic ventral mesh rectopexy. Surgery 156:158–167
Brunner M, Roth H, Günther K, Grützmann R, Matzel KE (2018) Ventral rectopexy with biological mesh: short-term functional results. Int J Color Dis 33(4):449–457
Raftopoulos Y, Senagore AJ, Di Giuro G, Bergamaschi R (2005) Rectal prolapse recurrence study group. Recurrence rates after abdominal surgery for complete rectal prolapse: a multicenter pooled analysis of 643 individual patient data. Dis Colon Rectum 48(6):1200–1206
Senapati A, Gray RG, Middleton LJ, Harding J, Hills RK, Armitage NC, Buckley L, Northover JM, PROSPER Collaborative Group (2013) PROSPER: a randomised comparison of surgical treatments for rectal prolapse. Color Dis 15(7):858–868
Hotouras A, Ribas Y, Zakeri S, Bhan C, Wexner SD, Chan CL, Murphy J (2015) A systematic review of the literature on the surgical management of recurrent rectal pro-lapse. Color Dis 17:657–664
Gurland B, Carvalho M, Ridgeway B et al (2017) Should we offer ventral rectopexy to patients with recurrent external rectal prolapse? Int J Color Dis 32:1561–1567
Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD (1996) A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum 39:681–685
Longo A (December 2006) 3rd German-Italian experts meeting, Rome, pp 12–14
Jorge JM, Wexner SD (1993) Etiology and management of fecal incontinence. Dis Colon Rectum 36:77–97
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
K.E. Matzel is a medical adviser to Medtronic.The other authors declare that they have no conflict of interest.
Statement of human rights
For this type of study, formal consent is not required.
Statement on the welfare of animals
This article does not contain any studies with animals performed by any of the authors.
Informed consent
This study contains no information that would enable individual patient identity.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brunner, M., Roth, H., Günther, K. et al. Ventral rectopexy with biological mesh for recurrent disorders of the posterior pelvic organ compartment. Int J Colorectal Dis 34, 1763–1769 (2019). https://doi.org/10.1007/s00384-019-03363-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03363-6