Abstract
Background
Following abdominoperineal resection (APR) for rectal cancer, perineal wound complications are common. Omental flap creation may allow for decreased morbidity. The aim of this study was to assess wound complications in rectal cancer patients undergoing APR with and without the addition of an omental flap.
Methods
The National Surgical Quality Improvement Program Proctectomy targeted database from 2016 to 2017 was used to identify all patients undergoing APR for rectal cancer. The primary outcomes were wound complications such as superficial site infection, deep wound infection, organ space infection, and wound dehiscence.
Results
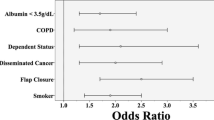
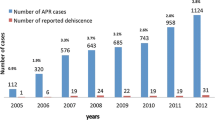
There were 3063 patients identified. One hundred seventy-three (5.6%) patients underwent APR with an omental flap repair while 2890 (94.4%) patients underwent APR without an omental flap repair. Patients in both groups were similar with regard to age, gender, body mass index, American Society of Anesthesia class, and neoadjuvant cancer treatment (all p > 0.05). Patients who underwent an omental flap repair were significantly more likely to have a postoperative organ space infection (10.4% vs. 6.5%, p = 0.04). There was no significant difference in rates of superficial site infection, deep wound infection, wound dehiscence, or reoperation between the two patient groups. In multivariable analysis, omental flap creation was independently associated with organ space infection (OR 1.72, 95%CI 1.02–2.90, p = 0.04).
Conclusions
This is the largest study to evaluate omental flap use in rectal cancer patients undergoing APR. Omental flaps are independently associated with organ space infection.

Similar content being viewed by others
References
Althumairi AA, Canner JK, Gearhart SL, Safar B, Sacks J, Efron JE (2016) Predictors of perineal wound complications and prolonged time to perineal wound healing after abdominoperineal resection. World J Surg 40(7):1755–1762
Rencuzogullari A, Gorgun E, Binboga S, Ozuner G, Kessler H, Abbas MA (2016) Predictors of wound dehiscence and its impact on mortality after abdominoperineal resection: data from the National Surgical Quality Improvement Program. Tech Coloproctol 20(7):475–482
Artioukh DY, Smith RA, Gokul K (2007) Risk factors for impaired healing of the perineal wound after abdominoperineal resection of rectum for carcinoma. Color Dis 9(4):362–367
Chessin DB, Hartley J, Cohen AM, Mazumdar M, Cordeiro P, Disa J, Mehrara B, Minsky BD, Paty P, Weiser M, Wong WD, Guillem JG (2005) Rectus flap reconstruction decreases perineal wound complications after pelvic chemoradiation and surgery: a cohort study. Ann Surg Oncol 12(2):104–110
Shukla HS, Tewari M (2010) An evolution of clinical application of inferior pedicle based rectus abdominis myocutaneous flap for repair of perineal defects after radical surgery for cancer. J Surg Oncol 102(3):287–294
Hawkins AT, Berger DL, Shellito PC, Sylla P, Bordeianou L (2014) Wound dehiscence after abdominoperineal resection for low rectal cancer is associated with decreased survival. Dis Colon Rectum 57(2):143–150
Butler CE, Gundeslioglu AO, Rodriguez-Bigas MA (2008) Outcomes of immediate vertical rectus abdominis myocutaneous flap reconstruction for irradiated abdominoperineal resection defects. J Am Coll Surg 206(4):694–703
Bullard KM, Trudel JL, Baxter NN, Rothenberger DA (2005) Primary perineal wound closure after preoperative radiotherapy and abdominoperineal resection has a high incidence of wound failure. Dis Colon Rectum 48(3):438–443
Wiatrek RL, Thomas JS, Papaconstantinou HT (2008) Perineal wound complications after abdominoperineal resection. Clin Colon Rectal Surg. 21(1):76–85
Kressner U, Graf W, Mahteme H, Pahlman L, Glimelius B (2002) Septic complications and prognosis after surgery for rectal cancer. Dis Colon Rectum 45(3):316–321
Christian CK, Kwaan MR, Betensky RA, Breen EM, Zinner MJ, Bleday R (2005) Risk factors for perineal wound complications following abdominoperineal resection. Dis Colon Rectum 48(1):43–48
Kamrava A, Mahmoud NN (2013) Prevention and management of nonhealing perineal wounds. Clin Colon Rectal Surg 26(2):106–111
Blok RD, de Jonge J, de Koning MA, van de Ven AWH, van der Bilt JDW, van Geloven AAW, Hompes R, Bemelman WA, Tanis PJ (2019) Propensity score adjusted comparison of pelviperineal morbidity with and without omentoplasty following abdominoperineal resection for primary rectal cancer. Dis Colon Rectum. https://doi.org/10.1097/DCR.0000000000001349
Kochar K, Marecik S, Prasad LM, Park J (2016) Omental pedicle flap does not decrease the incidence of bowel obstruction after abdominoperineal resection. Am Surg 82(11):e328–e330
ACS (2019). ACS National Surgical Quality Improvement Program. https://www.facs.org/quality-programs/acs-nsqip. Accessed 1 Apr 2019
Henderson WG, Daley J (2009) Design and statistical methodology of the National Surgical Quality Improvement Program: why is it what it is? Am J Surg 198(5 Suppl):S19–S27
ACS (2019). ACS NSQIP Participant Use Data File. https://www.facs.org/quality-programs/acs-nsqip/participant-use. Accessed 1 Apr 2019
Blok RD, Musters GD, Borstlap WAA et al (2018) Snapshot study on the value of omentoplasty in abdominoperineal resection with primary perineal closure for rectal cancer. Ann Surg Oncol 25(3):729–736
Anthony JP, Mathes SJ (1990) The recalcitrant perineal wound after rectal extirpation. Applications of muscle flap closure. Arch Surg 125(10):1371–1376 discussion 1376-1377
Oida T, Kawasaki A, Mimatsu K, Kano H, Kuboi Y, Fukino N, Kida K, Amano S (2012) Omental packing with continuous suction drainage following abdominoperineal resection. Hepatogastroenterology. 59(114):380–383
Hay JM, Fingerhut A, Paquet JC, Flamant Y (1997) Management of the pelvic space with or without omentoplasty after abdominoperineal resection for carcinoma of the rectum: a prospective multicenter study. The French Association for Surgical Research. Eur J Surg 163(3):199–206
Moreaux J, Horiot A, Barrat F, Mabille J (1984) Obliteration of the pelvic space with pedicled omentum after excision of the rectum for cancer. Am J Surg 148(5):640–644
Killeen S, Devaney A, Mannion M, Martin ST, Winter DC (2013) Omental pedicle flaps following proctectomy: a systematic review. Color Dis 15(11):e634–e645
Hultman CS, Sherrill MA, Halvorson EG, Lee CN, Boggess JF, Meyers MO, Calvo BA, Kim HJ (2010) Utility of the omentum in pelvic floor reconstruction following resection of anorectal malignancy: patient selection, technical caveats, and clinical outcomes. Ann Plast Surg 64(5):559–562
Nilsson PJ (2006) Omentoplasty in abdominoperineal resection: a review of the literature using a systematic approach. Dis Colon Rectum 49(9):1354–1361
Curran T, Poylin V, Nagle D (2016) Real world dehiscence rates for patients undergoing abdominoperineal resection with or without myocutaneous flap closure in the national surgical quality improvement project. Int J Color Dis 31(1):95–104
Manjoney DL, Koplewitz MJ, Abrams JS (1983) Factors influencing perineal wound healing after proctectomy. Am J Surg 145(1):183–189
Nissan A, Guillem JG, Paty PB, Wong DW, Minsky B, Saltz L, Cohen AM (2001) Abdominoperineal resection for rectal cancer at a specialty center. Dis Colon Rectum 44(1):27–35 discussion 35-26
Zaha H, Inamine S (2010) Laparoscopically harvested omental flap: results for 96 patients. Surg Endosc 24(1):103–107
Author information
Authors and Affiliations
Contributions
All authors had substantial contributions to design of work, drafted work, made final approval, and agreed to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Vanessa M. Welten and Adam C. Fields are co-first authors
Rights and permissions
About this article
Cite this article
Welten, V.M., Fields, A.C., Lu, P. et al. Omental flaps in patients undergoing abdominoperineal resection for rectal cancer. Int J Colorectal Dis 34, 1227–1232 (2019). https://doi.org/10.1007/s00384-019-03319-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03319-w