Abstract
Background
The importance of the defunctioning stoma on minimizing anastomotic leak in colorectal surgery is well established. However, a defunctioning stoma can substantially impact on quality of life (QoL). Circumferential purse-string approximation (PSA) and linear skin closure (LSC) are the most commonly performed surgical technique for reversal of stoma. The aim of this review was to systemically review and meta-analyze available randomized controlled trials (RCTs) comparing PSA and LSC.
Methods
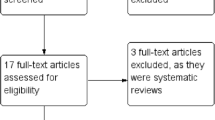
An electronic systematic search using MEDLINE databases (PubMed, EMBASE, and Web of Science) of RCTs comparing PSA and LSC was performed. Eight RCTs totalling 647 patients met the inclusion criteria and were included in this meta-analysis.
Results
Patient’s satisfaction is significantly lower in PSA group during the first postoperative week, but it sharply improves afterwards and no difference were noted at 1 and 6 months between the two groups. Relative risk (RR) of developing a SSI is significantly lower in PSA compared to LSC group (RR 0.16 95% CI 0.09; 0.30; p = 0.0001), whereas incisional hernia (RR 0.53 95% CI 0.08; 3.53; p = 0.512), operative time (MD − 0.06 95% CI − 0.30; 0.17; p = 0.593), and hospital stay (MD − 0.09 (95% CI − 0.29-0.11; p = 0.401) remain similar.
Discussion
QoL was similar in both patients groups after the first postoperative week. PSA significantly reduced SSI rate. No difference was observed in incisional hernia rate, operative time, or length of hospital stay.






Similar content being viewed by others
References
Tan WS, Tang CL, Shi L, Eu KW (2009) Meta-analysis of defunctioning stomas in low anterior resection for rectal cancer. Br J Surg 96(5):462–472
Wrenn SM, Cepeda-Benito A, Ramos-Valadez DI, Cataldo PA (2018) Patient perceptions and quality of life after colon and rectal surgery: what do patients really want? Dis Colon Rectum 61(8):971–978
Yin TC, Tsai HL, Yang PF, Su WC, Ma CJ, Huang CW, Huang MY, Huang CM, Wang JY (2017) Early closure of defunctioning stoma increases complications related to stoma closure after concurrent chemoradiotherapy and low anterior resection in patients with rectal cancer. World J Surg Oncol 15(1):80
McCartan DP, Burke JP, Walsh SR, Coffey JC (2013) Purse-string approximation is superior to primary skin closure following stoma reversal: a systematic review and meta-analysis. Tech Coloproctol 17(4):345–351
Banerjee A (1997) Pursestring skin closure after stoma reversal. Dis Colon Rectum 40(8):993–994
O'Leary DP, Carter M, Wijewardene D, Burton M, Waldron D, Condon E et al (2017) The effect of purse-string approximation versus linear approximation of ileostomy reversal wounds on morbidity rates and patient satisfaction: the ‘STOMA’ trial. Tech Coloproctol 21(11):863–868
Zubaidah NH, Soo JY, Qisti N, Ong KW, Gee T (2016) Wound infection following stoma reversal: a prospective comparative study between primary closure and partial closure with intervening silver dressings. Int J Color Dis 31:1381–1382
Hsieh MC, Kuo LT, Chi CC, Huang WS, Chin CC (2015) Pursestring closure versus conventional primary closure following stoma reversal to reduce surgical site infection rate: a meta-analysis of randomized controlled trials. Dis Colon Rectum 58(8):808–815
Sureshkumar S, Jubel K, Ali MS, Vijayakumar C, Amaranathan A, Sundaramoorthy S et al (2018) Comparing surgical site infection and scar cosmesis between conventional linear skin closure versus purse-string skin closure in stoma reversal - a randomized controlled trial. Cureus 10(2):e2181
Lopez MP, Melendres MF, Maglangit SA, Roxas MF, Monroy HJ 3rd, Crisostomo AC (2015) A randomized controlled clinical trial comparing the outcomes of circumferential subcuticular wound approximation (CSWA) with conventional wound closure after stoma reversal. Tech Coloproctol 19(8):461–468
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Sweeting MJ, Sutton AJ, Lambert PC (2004) What to add to nothing? Use and avoidance of continuity corrections in meta-analysis of sparse data. Stat Med 23(9):1351–1375
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Duval SJ (2005) The trim and fill method. In: Rothstein HR, Sutton AJ, Borenstein M (eds) Publication bias in meta-analysis: prevention, assessment, and adjustments. Wiley, Chichester, pp 127–144
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Borenstein M, Hedges LV, Higgins JP, Rothstein HR (2010) A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods 1(2):97–111
Cooper H, Hedges LV (1994) The handbook of research synthesis. Russell Sage Foundation, Newbury Park
R Development Core Team (2015) A language and enviroment for statistical computing. R Foundation for Statistical Computing, Vienna ISBN 3-900051-07-0
Draaijers LJ, Tempelman FR, Botman YA, Tuinebreijer WE, Middelkoop E, Kreis RW et al (2004) The patient and observer scar assessment scale: a reliable and feasible tool for scar evaluation. Plast Reconstr Surg 113(7):1960–1965 discussion 6-7
Dunker MS, Stiggelbout AM, van Hogezand RA, Ringers J, Griffioen G, Bemelman WA (1998) Cosmesis and body image after laparoscopic-assisted and open ileocolic resection for Crohn’s disease. Surg Endosc 12(11):1334–1340
Polle SW, Dunker MS, Slors JF, Sprangers MA, Cuesta MA, Gouma DJ et al (2007) Body image, cosmesis, quality of life, and functional outcome of hand-assisted laparoscopic versus open restorative proctocolectomy: long-term results of a randomized trial. Surg Endosc 21(8):1301–1307
Likert R (1932) A techique for the measurement of attitudes. Arch Psychol 140:1–55
Ware JE Jr, Kosinski M, Gandek B, Aaronson NK, Apolone G, Bech P, Brazier J, Bullinger M, Kaasa S, Leplège A, Prieto L, Sullivan M (1998) The factor structure of the SF-36 Health Survey in 10 countries: results from the IQOLA project. International quality of life assessment. J Clin Epidemiol 51(11):1159–1165
Alvandipour M, Gharedaghi B, Khodabakhsh H, Karami MY (2016) Purse-string versus linear conventional skin wound closure of an ileostomy: a randomized clinical trial. Ann Coloproctol 32(4):144–149
Camacho-Mauries D, Rodriguez-Diaz JL, Salgado-Nesme N, Gonzalez QH, Vergara-Fernandez O (2013) Randomized clinical trial of intestinal ostomy takedown comparing pursestring wound closure vs conventional closure to eliminate the risk of wound infection. Dis Colon Rectum 56(2):205–211
Dusch N, Goranova D, Herrle F, Niedergethmann M, Kienle P (2013) Randomized controlled trial: comparison of two surgical techniques for closing the wound following ileostomy closure: purse string vs direct suture. Color Dis 15(8):1033–1040
Lee JT, Marquez TT, Clerc D, Gie O, Demartines N, Madoff RD, Rothenberger DA, Christoforidis D (2014) Pursestring closure of the stoma site leads to fewer wound infections: results from a multicenter randomized controlled trial. Dis Colon Rectum 57(11):1282–1289
Reid K, Pockney P, Pollitt T, Draganic B, Smith SR (2010) Randomized clinical trial of short-term outcomes following purse-string versus conventional closure of ileostomy wounds. Br J Surg 97(10):1511–1517
Gu WL, Wu SW (2015) Meta-analysis of defunctioning stoma in low anterior resection with total mesorectal excision for rectal cancer: evidence based on thirteen studies. World J Surg Oncol 13:9
Worni M, Witschi A, Gloor B, Candinas D, Laffer UT, Kuehni CE (2011) Early closure of ileostomy is associated with less postoperative nausea and vomiting. Dig Surg 28(5–6):417–423
Herrle F, Sandra-Petrescu F, Weiss C, Post S, Runkel N, Kienle P (2016) Quality of life and timing of stoma closure in patients with rectal cancer undergoing low anterior resection with diverting stoma: a multicenter longitudinal observational study. Dis Colon Rectum 59(4):281–290
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
What does this paper add to the existing literature?
This review showed that patient’s satisfaction is lower in PSA group during the first postoperative week, whereas there is no difference when compared at 1 and 6 months. SSI rate is lower in PSA, whereas incisional hernia rate, operative time, and length of hospital stay are similar between the two groups.
Paper is containing original research and has not been submitted/published earlier in any journal and is not being considered for publication elsewhere.
Rights and permissions
About this article
Cite this article
Rausa, E., Kelly, M.E., Sgroi, G. et al. Quality of life following ostomy reversal with purse-string vs linear skin closure: a systematic review. Int J Colorectal Dis 34, 209–216 (2019). https://doi.org/10.1007/s00384-018-3219-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-3219-z