Abstract
Purpose
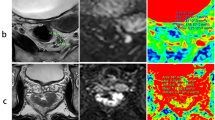
The prediction of an infiltration of the mesorectal fascia (MRF) and malignant lymph nodes is essential for treatment planning and prognosis of patients with rectal cancer. The aim of this study was to assess the additional diagnostic value of dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) for the detection of a malignant involvement of the MRF and of mesorectal lymph nodes in patients with locally advanced rectal cancer.
Methods
In this prospective study, 22 patients with locally advanced rectal cancer were examined with 1.5-T MRI between September 2012 and April 2015. Histopathological assessment of tumor size, tumor infiltration to the MRF, and malignant involvement of locoregional lymph nodes served as standard of reference. Sensitivity and specificity of detecting MRF infiltration and malignant nodes (nodal cut-off size [NCO] ≥ 5 and ≥ 10 mm, respectively) was determined by conventional MRI (cMRI; precontrast and postcontrast T1-weighted, T2-weighted, and diffusion-weighted images) and by additional semi-quantitative DCE-MRI maps (cMRI+DCE-MRI).
Results
Compared to cMRI, additional semi-quantitative DCE-MRI maps significantly increased sensitivity (86 vs. 71% [NCO ≥ 5 mm]/29% [NCO ≥ 10 mm]) and specificity (90 vs. 70% [NCO ≥ 5 mm]) of detecting malignant lymph nodes (p < 0.05). Moreover, DCE-MRI significantly augmented specificity (91 vs. 82%) of discovering a MRF infiltration (p < 0.05), while there was no change in sensitivity (83%; p > 0.05).
Conclusion
DCE-MRI considerably increases both sensitivity and specificity for the detection of small mesorectal lymph node metastases (≥ 5 mm but < 10 mm) and sufficiently improves specificity of a suspected MRF infiltration in patients with locally advanced rectal cancer.



Similar content being viewed by others
References
Siegel R, Naishadham D, Jemal A (2013) Cancer statistics, 2013. CA Cancer J Clin 63:11–30
Pox CP, Schmiegel W (2013) German S3-guideline colorectal carcinoma. Dtsch Med Wochenschr 138:2545
Marijnen CA et al (2005) Impact of short-term preoperative radiotherapy on health-related quality of life and sexual functioning in primary rectal cancer: report of a multicenter randomized trial. J Clin Oncol 23:1847–1858
Patel UB, Blomqvist LK, Taylor F, George C, Guthrie A, Bees N, Brown G (2012) MRI after treatment of locally advanced rectal cancer: how to report tumor response—the MERCURY experience. AJR Am J Roentgenol 199:W486–W495
Patel UB, Taylor F, Blomqvist L, George C, Evans H, Tekkis P, Quirke P, Sebag-Montefiore D, Moran B, Heald R, Guthrie A, Bees N, Swift I, Pennert K, Brown G (2011) Magnetic resonance imaging-detected tumor response for locally advanced rectal cancer predicts survival outcomes: MERCURY experience. J Clin Oncol 29:3753–3760
Taylor FG, Quirke P, Heald RJ, Moran BJ, Blomqvist L, Swift IR, Sebag-Montefiore D, Tekkis P, Brown G, Magnetic Resonance Imaging in Rectal Cancer European Equivalence Study Study Group (2014) Preoperative magnetic resonance imaging assessment of circumferential resection margin predicts disease-free survival and local recurrence: 5-year follow-up results of the MERCURY study. J Clin Oncol 32:34–43
Garcia-Aguilar J, Shi Q, Thomas CR, Chan E, Cataldo P, Marcet J, Medich D, Pigazzi A, Oommen S, Posner MC (2012) A phase II trial of neoadjuvant chemoradiation and local excision for T2N0 rectal cancer: preliminary results of the ACOSOG Z6041 trial. Ann Surg Oncol 19:384–391
Yu CS, Yun HR, Shin EJ, Lee KY, Kim NK, Lim SB, Oh ST, Kang SB, Choi WJ, Lee WY, Colorectal Cancer Study Group, Korean Society of Coloproctology (2013) Local excision after neoadjuvant chemoradiation therapy in advanced rectal cancer: a national multicenter analysis. Am J Surg 206:482–487
Shin YS, Yu CS, Park JH, Kim JC, Lim SB, Park IJ, Kim TW, Hong YS, Kim KP, Yoon SM, Joo JH, Kim JH (2017) Total mesorectal excision versus local excision after favorable response to preoperative chemoradiotherapy in “early” clinical T3 rectal cancer: a propensity score analysis. Int J Radiat Oncol Biol Phys 99:136–144
Beets-Tan RG et al (2013) Magnetic resonance imaging for the clinical management of rectal cancer patients: recommendations from the 2012 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. Eur Radiol 23:2522–2531
Quaia E, Gennari AG, de Paoli L, Angileri R, Ukmar M, Cova MA (2014) Predictors of mesorectal fascia invasion after gadolinium injection in rectal carcinoma after neoadjuvant therapy. Clin Imaging 38:698–703
Nougaret S, Reinhold C, Mikhael HW, Rouanet P, Bibeau F, Brown G (2013) The use of MR imaging in treatment planning for patients with rectal carcinoma: have you checked the “DISTANCE”? Radiology 268:330–344
Kono Y, Togashi K, Utano K, Horie H, Miyakura Y, Fukushima N, Lefor AT, Yasuda Y (2015) Lymph node size alone is not an accurate predictor of metastases in rectal cancer: a node-for-node comparative study of specimens and histology. Am Surg 81:1263–1271
Langman G, Patel A, Bowley DM (2015) Size and distribution of lymph nodes in rectal cancer resection specimens. Dis Colon Rectum 58:406–414
Kim IK, Kang J, Lim BJ, Sohn SK, Lee KY (2015) The impact of lymph node size to predict nodal metastasis in patients with rectal cancer after preoperative chemoradiotherapy. Int J Color Dis 30:459–464
Grone J, Loch FN, Taupitz M, Schmidt C, Kreis ME (2018) Accuracy of various lymph node staging criteria in rectal cancer with magnetic resonance imaging. J Gastrointest Surg 22:146–153
Heijnen LA, Maas M, Beets-Tan RG, Berkhof M, Lambregts DM, Nelemans PJ, Riedl R, Beets GL (2016) Nodal staging in rectal cancer: why is restaging after chemoradiation more accurate than primary nodal staging? Int J Color Dis 31:1157–1162
Brown G, Richards CJ, Bourne MW, Newcombe RG, Radcliffe AG, Dallimore NS, Williams GT (2003) Morphologic predictors of lymph node status in rectal cancer with use of high-spatial-resolution MR imaging with histopathologic comparison. Radiology 227:371–377
Bipat S, Glas AS, Slors FJM, Zwinderman AH, Bossuyt PMM, Stoker J (2004) Rectal cancer: local staging and assessment of lymph node involvement with endoluminal US, CT, and MR imaging—a meta-analysis. Radiology 232:773–783
Brix G, Semmler W, Port R, Schad LR, Layer G, Lorenz WJ (1991) Pharmacokinetic parameters in CNS Gd-DTPA enhanced MR imaging. J Comput Assist Tomogr 15:621–628
Gaa T, Neumann W, Sudarski S, Attenberger UI, Schönberg SO, Schad LR, Zöllner FG (2017) Comparison of perfusion models for quantitative T1 weighted DCE-MRI of rectal cancer. Sci Rep 7:12036
Koh TS, Bisdas S, Koh DM, Thng CH (2011) Fundamentals of tracer kinetics for dynamic contrast-enhanced MRI. J Magn Reson Imaging 34:1262–1276
Alberda WJ, Dassen HPN, Dwarkasing RS, Willemssen FEJA, van der Pool AEM, de Wilt JHW, Burger JWA, Verhoef C (2013) Prediction of tumor stage and lymph node involvement with dynamic contrast-enhanced MRI after chemoradiotherapy for locally advanced rectal cancer. Int J Color Dis 28:573–580
Yao WW, Zhang H, Ding B, Fu T, Jia H, Pang L, Song L, Xu W, Song Q, Chen K, Pan Z (2011) Rectal cancer: 3D dynamic contrast-enhanced MRI; correlation with microvascular density and clinicopathological features. Radiol Med 116:366–374
Do RK, Rusinek H, Taouli B (2009) Dynamic contrast-enhanced MR imaging of the liver: current status and future directions. Magn Reson Imaging Clin N Am 17:339–349
Sourbron S, Sommer WH, Reiser MF, Zech CJ (2012) Combined quantification of liver perfusion and function with dynamic gadoxetic acid-enhanced MR imaging. Radiology 263:874–883
Taylor FG et al (2011) One millimetre is the safe cut-off for magnetic resonance imaging prediction of surgical margin status in rectal cancer. Br J Surg 98:872–879
Ma X et al (2015) Characteristics and prognostic significance of preoperative magnetic resonance imaging-assessed circumferential margin in rectal cancer. Gastroenterol Res Pract 410150:2015
Yu XP, Wen L, Hou J, Wang H, Lu Q (2016) Discrimination of metastatic from non-metastatic mesorectal lymph nodes in rectal cancer using quantitative dynamic contrast-enhanced magnetic resonance imaging. J Huazhong Univ Sci Technolog Med Sci 36:594–600
Grovik E et al (2017) Dynamic multi-echo DCE- and DSC-MRI in rectal cancer: low primary tumor Ktrans and DeltaR2* peak are significantly associated with lymph node metastasis. J Magn Reson Imaging 46:194–206
Lollert A, Junginger T, Schimanski CC, Biesterfeld S, Gockel I, Düber C, Oberholzer K (2014) Rectal cancer: dynamic contrast-enhanced MRI correlates with lymph node status and epidermal growth factor receptor expression. J Magn Reson Imaging 39:1436–1442
Yu XP, Wen L, Hou J, Bi F, Hu P, Wang H, Wang W (2016) Discrimination between metastatic and nonmetastatic mesorectal lymph nodes in rectal cancer using intravoxel incoherent motion diffusion-weighted magnetic resonance imaging. Acad Radiol 23:479–485
van Gijn W, Marijnen CA, Nagtegaal ID, Kranenbarg EM, Putter H, Wiggers T, Rutten HJ, Påhlman L, Glimelius B, van de Velde C, Dutch Colorectal Cancer Group (2011) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol 12:575–582
Xie H, Zhou X, Zhuo Z, Che S, Xie L, Fu W (2014) Effectiveness of MRI for the assessment of mesorectal fascia involvement in patients with rectal cancer: a systematic review and meta-analysis. Dig Surg 31:123–134
Kim DJ, Kim JH, Lim JS, Yu JS, Chung JJ, Kim MJ, Kim KW (2010) Restaging of rectal cancer with MR imaging after concurrent chemotherapy and radiation therapy. Radiographics 30:503–516
Park MJ, Kim SH, Lee SJ, Jang KM, Rhim H (2011) Locally advanced rectal cancer: added value of diffusion-weighted MR imaging for predicting tumor clearance of the mesorectal fascia after neoadjuvant chemotherapy and radiation therapy. Radiology 260:771–780
Acknowledgements
The authors are most grateful to Dr. Simone Reu for providing histopathologic images and thank Dres. Ursula and Günther Karpitschka for their profound support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Armbruster, M., D’Anastasi, M., Holzner, V. et al. Improved detection of a tumorous involvement of the mesorectal fascia and locoregional lymph nodes in locally advanced rectal cancer using DCE-MRI. Int J Colorectal Dis 33, 901–909 (2018). https://doi.org/10.1007/s00384-018-3083-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-3083-x