Abstract
Purpose
Postoperative nasogastric decompression has been routinely used after intestinal surgery. However, the role of nasogastric decompression in preventing postoperative complications and promoting the recovery of bowel function in children remains controversial. This systematic review aimed to assess whether routine nasogastric decompression is necessary after intestinal surgery in children.
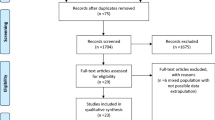
Methods
A systematic review was conducted following the PRISMA guideline. Literature search was performed in electronic databases including PubMed, Embase, CENTRAL, and Web of science. Studies comparing outcomes between children who underwent intestinal surgery with postoperative nasogastric tube (NGT) placement (NGT group) and without postoperative NGT placement (no NGT group) were included.
Results
Six studies were eligible for inclusion criteria including two randomized controlled trials (RCT) and four comparative observational studies. The overall rate of postoperative anastomotic leak was 0.6% (1/179) in NGT group and 0.9% (2/223) in no NGT group. The overall rate of wound dehiscence was 2.4% (4/169) in NGT group and 1.6% (4/245) in no NGT group. Meta-analysis of two RCTs in children undergoing elective intestinal surgery showed significant increase of mild vomiting in no NGT group compared with NGT group (OR 3.54 95% CI 1.04, 11.99) but no significant difference in persistent vomiting requiring NGT reinsertion (OR 3.11 95% CI 0.47, 20.54), abdominal distension (OR 2.36 95% CI 0.34, 16.59), NGT reinsertion (OR 3.11 95% CI 0.47, 20.54), wound infection (OR 1.63 95% CI 0.49, 5.48) and time to return of bowel movement (MD − 0.14 95% CI − 0.45, 0.17). There was no incidence of anastomotic leak in these 2 RCTs. However, there was an incidence of NGT-related discomfort in NGT group, which ranged from 30 to 100% of children studied.
Conclusion
Routine postoperative nasogastric decompression can be omitted in children undergoing intestinal surgery due to no benefit in preventing postoperative complications while increasing patient discomfort.


Similar content being viewed by others
References
Savassi-Rocha PR, Conceicão SA, Ferreira JT et al (1992) Evaluation of the routine use of the nasogastric tube in digestive operation by a prospective controlled study. Surg Gynecol Obstet 174:317–320. https://doi.org/10.1097/00132586-199212000-00025
Nelson R, Edwards S, Tse B (2005) Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD004929.pub2
Rao W, Zhang X, Zhang J et al (2011) The role of nasogastric tube in decompression after elective colon and rectum surgery: a meta-analysis. Int J Colorectal Dis 26:423–429. https://doi.org/10.1007/s00384-010-1093-4
Sapkota R, Bhandari RS (2013) Prophylactic nasogastric decompression after emergency laparotomy. J Nepal Med Assoc 52:437–442. https://doi.org/10.31729/jnma.2263
Vinay HG, Raza M, Siddesh G (2015) Elective bowel surgery with or without prophylactic nasogastric decompression: a prospective, randomized trial. J Surg Tech Case Rep 7:37–41. https://doi.org/10.4103/2006-8808.185654
Macarone RP, Amodio PM, Rizzello M et al (2012) Does the nasogastric tube has a role in elective colo-rectal surgery? Il G Chir 33:58–61
Varadhan KK, Neal KR, Dejong CHC et al (2010) The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta-analysis of randomized controlled trials. Clin Nutr 29:434–440. https://doi.org/10.1016/j.clnu.2010.01.004
Gustafsson UO, Scott MJ, Schwenk W et al (2012) Guidelines for perioperative care in elective colonic surgery: enhanced recovery after surgery (ERAS®) society recommendations. Clin Nutr Edinb Scotl 31:783–800. https://doi.org/10.1016/j.clnu.2012.08.013
Shinnick JK, Short HL, Heiss KF et al (2016) Enhancing recovery in pediatric surgery: a review of the literature. J Surg Res 202:165–176. https://doi.org/10.1016/j.jss.2015.12.051
Gao R, Yang H, Li Y et al (2019) Enhanced recovery after surgery in pediatric gastrointestinal surgery. J Int Med Res 47:4815–4826. https://doi.org/10.1177/0300060519865350
Davila-Perez R, Bracho-Blanchet E, Tovilla-Mercado JM et al (2010) Unnecessary gastric decompression in distal elective bowel anastomoses in children: a randomized study. World J Surg 34:947–953. https://doi.org/10.1007/s00268-010-0442-3
Khan NA, Roy Choudhury S, Yadav PS et al (2017) Role of nasogastric tube in children undergoing elective distal bowel surgery. Pediatr Surg Int 33:229–234. https://doi.org/10.1007/s00383-016-4019-6
Abantanga FA (2012) Nasogastric tube use in children after abdominal surgery- how long should it be kept in situ? West Afr J Med 31:19–23
Sandler AD, Evans D, Ein SH (1998) To tube or not to tube: do infants and children need post-laparotomy gastric decompression? Pediatr Surg Int 13:411–413. https://doi.org/10.1007/s003830050351
St Peter SD, Valusek PA, Little DC et al (2007) Does routine nasogastric tube placement after an operation for perforated appendicitis make a difference? J Surg Res 143:66–69. https://doi.org/10.1016/j.jss.2007.04.009
Sekioka A, Fukumoto K, Takahashi T et al (2019) Is a nasogastric tube necessary after transumbilical laparoscopic-assisted appendectomy in children with perforated appendicitis? World J Pediatr 15:615–619. https://doi.org/10.1007/s12519-019-00280-0
Gustafsson UO, Scott MJ, Hubner M et al (2019) Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS®) society recommendations: 2018. World J Surg 43:659–695. https://doi.org/10.1007/s00268-018-4844-y
Hayashi M, Kawakubo H, Shoji Y et al (2019) Analysis of the effect of early versus conventional nasogastric tube removal on postoperative complications after transthoracic esophagectomy: a single-center, randomized controlled trial. World J Surg 43:580–589. https://doi.org/10.1007/s00268-018-4825-1
Kimura Y, Yano H, Iwazawa T et al (2017) One-day nasogastric tube decompression after distal gastrectomy: a prospective randomized study. Surg Today 47:1080–1085. https://doi.org/10.1007/s00595-017-1475-0
Wen Z, Zhang X, Liu Y et al (2019) Is routine nasogastric decompression after hepatic surgery necessary? A systematic review and meta-analysis. Int J Nurs Stud 100:103406. https://doi.org/10.1016/j.ijnurstu.2019.103406
Kleive D, Sahakyan MA, Labori KJ, Lassen K (2019) Nasogastric tube on demand is rarely necessary after pancreatoduodenectomy within an enhanced recovery pathway. World J Surg 43:2616–2622. https://doi.org/10.1007/s00268-019-05045-4
Zhao T, Huang L, Tian Y et al (2014) Is it necessary to insert nasogastric tube routinely after radical cystectomy with urinary diversion? A meta-analysis. Int J Clin Exp Med 7:4627–4634
Erickson BA, Dorin RP, Clemens JQ (2007) Is nasogastric tube drainage required after reconstructive surgery for neurogenic bladder dysfunction? Urology 69:885–888. https://doi.org/10.1016/j.urology.2007.01.061
Tanguy M, Seguin P, Mallédant Y (2007) Bench-to-bedside review: routine postoperative use of the nasogastric tube—utility or futility? Crit Care 11:201. https://doi.org/10.1186/cc5118
Sholadoye TT, Suleiman AF, Mshelbwala PM, Ameh EA (2012) Early oral feeding following intestinal anastomoses in children is safe. Afr J Paediatr Surg 9:113–116. https://doi.org/10.4103/0189-6725.99395
Mamatha B, Alladi A (2015) Early oral feeding in pediatric intestinal anastomosis. Indian J Surg 77:670–672. https://doi.org/10.1007/s12262-013-0971-8
Sangkhathat S, Patrapinyokul S, Tadyathikom K (2003) Early enteral feeding after closure of colostomy in pediatric patients. J Pediatr Surg 38:1516–1519. https://doi.org/10.1016/s0022-3468(03)00506-2
Yadav PS, Choudhury SR, Grover JK et al (2013) Early feeding in pediatric patients following stoma closure in a resource limited environment. J Pediatr Surg 48:977–982. https://doi.org/10.1016/j.jpedsurg.2013.02.013
Funding
This study was funded by the Naccarato Foundation.
Author information
Authors and Affiliations
Contributions
SC, MY, and AP contributed to the study conception and design. Literature search and data analysis were performed by SC and MY. The first draft of the manuscript was written by SC, MY, NG, PV and AP. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chusilp, S., Yamoto, M., Vejchapipat, P. et al. Nasogastric decompression after intestinal surgery in children: a systematic review and meta-analysis. Pediatr Surg Int 37, 377–388 (2021). https://doi.org/10.1007/s00383-020-04818-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-020-04818-6