Abstract
Congenital diaphragmatic hernia (CDH) is a relatively common and life-threatening birth defect, characterized by incomplete formation of the diaphragm. Because CDH herniation occurs at the same time as preacinar airway branching, normal lung development becomes severely disrupted, resulting almost invariably in pulmonary hypoplasia. Despite various research efforts over the past decades, the pathogenesis of CDH and associated lung hypoplasia remains poorly understood. With the advent of molecular techniques, transgenic animal models of CDH have generated a large number of candidate genes, thus providing a novel basis for future research and treatment. This review article offers a comprehensive overview of genes and signaling pathways implicated in CDH etiology, whilst also discussing strengths and limitations of transgenic animal models in relation to the human condition.
Similar content being viewed by others
Introduction
Congenital diaphragmatic hernia (CDH) is a developmental abnormality characterized by the presence of a defect in the integrity of the forming diaphragm, affecting between 1.9 and 2.3 cases per 10,000 newborns in the United States [1] and Europe [2]. Defects in the posterolateral diaphragm, commonly referred to as Bochdalek hernias, comprise approximately 90-95% of all CDH cases with about 80% occurring on the left side, 15% on the right and less than 5% bilaterally [3]. Non-posterolateral CDH manifests as anterior conditions such as Morgagni hernias in the anterior retrosternal or peristernal diaphragm and central hernias in the central tendinous portion of the diaphragm [4]. Posterolateral diaphragmatic defects permit protrusion of the abdominal viscera into the thoracic cavity, thus interfering with normal lung development and frequently leading to severe respiratory distress at birth due to the unfortunate combination of pulmonary hypoplasia and persistent pulmonary hypertension of the newborn [3, 5].
Over the last decade, CDH remained a life-threatening congenital disorder with mortality rates up to 50% [6,7,8,9]. Treatment usually consists of surgical movement of the abdominal viscera out of the thoracic cavity and closure of the diaphragmatic defect. Large defects may be difficult to repair through direct sutures, requiring the use of a prosthetic patch or abdominal muscle flap [10, 11]. Apart from surgical methods, treatment options for CDH are limited due to its poorly understood etiology, thereby motivating the need for better experimental models to elucidate its pathogenesis while also testing new therapeutic approaches. Investigation of novel medical therapies and pharmacological compounds that have the ability to arrest or reverse associated lung hypoplasia in animal models of CDH require the application of standardized research methodologies [12]. In this review article, we discuss the development of and findings associated with transgenic animal models of CDH to highlight the progress made to date in understanding CDH pathogenesis and evolution.
Transgenic animal models of CDH
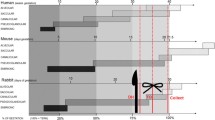
Both environmental and genetic factors are thought to contribute to the etiology of CDH. To date, genetic causes have been identified in approximately 30% of neonates with CDH [13,14,15]. With the advent of innovative molecular techniques in recent years, transgenic animal models of CDH have become more common, offering new candidate genes and signaling pathways implicated in the pathogenesis and etiology of diaphragmatic defects and associated lung abnormalities (Table 1). So far, 18 mouse models with phenotypic similarities to human CDH have been listed in the Mouse Genome Database (http://www.informatics.jax.org).
Retinoid signaling pathway
Several knockout models have originated from gene pathways found to be associated with CDH such as the retinoid signaling pathway [13]. Mice deficient in both subtypes of retinoic acid receptors α and β (Rarα and Rarβ) have been shown to produce offspring with CDH [16,17,18,19,20,21], consistent with the vitamin A-deficient mouse models observed by Anderson [22, 23]. Single Rar null mutation mice did not exhibit the expected anomalies, which were reported in vitamin A-deficient rats [9]. However, when the function of these receptors was suppressed, multiple congenital anomalies were observed, including right-sided CDH in Rarαβ2 mutant mice and left-sided CDH in Rarαβ2+/− animals. In addition, these mice suffer from severe pulmonary hypertension at birth [9]. Unfortunately, these animals demonstrate a relative low rate of diaphragmatic defects and a high incidence of comorbidities including cranial, vertebral, limb, cardiac, foregut and pulmonary malformations that do not accurately reflect human CDH [20, 21]. Nevertheless, mutations in the stimulated by retinoic acid gene 6 (STRA6) and cellular retinoic acid binding protein 1 (CRABP1) on chromosome 15 have been identified in CDH patients [9].
Nr2f2 (Couptf2)
Another gene associated with the retinoid signaling pathway is chickovalbuminupstreampromoter transcription factor II (COUP-TFII), a transcription factor belonging to the steroid/thyroid hormone receptor superfamily, whose DNA-binding site has been found to downregulate hormonal induction of retinoic acid receptors [24,25,26]. Recently, COUP-TFII was renamed as nuclear receptor subfamily 2, group F, member 2 (NR2F2) [13]. Mapping to chromosome 15q26, the NR2F2 gene is located on a well-known CDH hotspot region in humans, making it a strong candidate gene for CDH pathogenesis. Based on this knowledge, You et al. [27] have developed a tissue-specific Nr2f2 null mutant mouse model that exhibits Bochdalek-type CDH. In ablating Nr2f2 in the foregut mesenchyme, diaphragmatic defects occurred due to the failure of the posthepatic mesenchymal plate to attach to the lateral body wall [27].
Wt1
Developing transgenic animal models for various applications has also uncovered genes less likely to be associated with CDH. Originally created as a model to study early urogenital development [28], Wilm’s tumor 1 (Wt1) null mutant mice displayed diaphragmatic defects in addition to urogenital malformations. Mutations of the WT1 gene, which encodes a DNA-binding protein with four zinc fingers, have been identified in two CDH-related cases of Denys-Drash syndrome [29] and in one case of Meacham syndrome [30]. A decade ago, vitamin A-deficient, nitrofen and Wt1 null mutant mouse models of CDH all suggested a common pathogenic mechanism for CDH development with similarities to the human condition [31]. Moreover, Carmona et al. [32] have shown that conditional deletion of Wt1 in the septum transversum mesenchyme causes CDH in mice. It is now established that Wt1 and Couptf2 both interact with retinoid signaling during embryogenesis [33]. Interestingly, Wt1 and Couptf2 are not expressed in the muscle precursors but in the non-muscle mesenchymal component of the pleuroperitoneal folds (PPFs) [33].
Msc (MyoR) and Tcf21 (capsulin)
The double mutant musculin (Msc)−/− and transcription factor 21 (Tcf21)−/− mouse model, initially generated to characterize facial muscle development, features posterior CDH along with facial muscle defects. Although these double mutant mice died shortly after birth, the model’s diaphragmatic defect suggests that both Msc and Tcf21 are required to maintain the integrity of the forming diaphragm. Today, their synonyms are known as myogenic bHLH transcription factor R (MyoR) and capsulin, respectively [34, 35].
Gli2/3, Shh and Kif7
GLI-Kruppel family member 2 (Gli2), Gli3 and sonic hedgehog (Shh) are members of a highly conserved morphogenetic family, which is known as the Shh signaling pathway [9, 36]. Murine models of VACTERL (vertebral, anorectal, cardiac, tracheoesophageal, renal and limb anomalies) syndrome involving Gli2−/−-, Gli3−/−- and Gli2−/−/Gli3+/−-mice developed left-sided CDH in addition to the reported VACTERL anomalies [36]. This is the first model that imitates the human VACTERL association, suggesting that aberations in Shh signaling might be involved in the VACTERL syndrome [37]. Furthermore, as Gli2, Gli3 and Wt1 all encode zinc finger proteins, other zinc finger transcription factors have also been associated with the development of transgenic animal models of CDH. Kinesin family member 7 (Kif7) has recently been identified as an essential component of the Shh signaling pathway as a negative regulator in early embryonic development [38]. Kif7 encodes a motor protein that functions downstream of the G protein-coupled transmembrane receptor smoothened, and interacts with Gli2 and Gli3 [38]. Additionally, Kif7 is required for the patterning and differentiation of the diaphragm in a model of syndromic CDH [38].
Zfpm2, Gata4, Sox7 and Frem1
Zinc finger protein, multitype 2 (ZFPM2), previously known as friend of GATA-binding protein 2 (FOG2), similarly encodes a zinc finger protein that primarily interacts with another zinc finger protein GATA4 to regulate various developmental processes in the diaphragm, lung and heart [39,40,41]. Moreover, ZFPM2 is located on chromosome 8p23 and interacts physically with COUP-TFII [42, 43]. Despite sufficient evidence that certain genes are involved in the pathogenesis of different types of CDH, only one mutation in ZFPM2 has been demonstrated in a single patient with non-syndromic CDH until now [9]. In a cohort of 275 CDH patient exomes, Longoni et al. [44] have estimated the prevalence of damaging ZFPM2 mutations to be almost 5%. Furthermore, genetic analysis of a multi-generational family identified a heritable intragenic ZFPM2 deletion with an estimated penetrance of 37.5% [44]. Mice treated with the chemical mutagen N-ethyl-N-nitrosourea in turn produced Fog2−/− offspring with pulmonary hypoplasia and abnormal diaphragmatic development characteristic of CDH [39], while a double knockout strain of Gata4 mice predisposed inbred mice to comparable physical defects [45]. Using mouse genetics, Merrell et al. [46] have confirmed that Gata4 mosaic mutations in PPF-derived muscle connective tissue fibroblasts result in the formation of localized amuscular regions that are biomechanically weaker and lead to CDH. Both ZFPM2 and GATA4 genes have been reportedly deleted in human CDH patients [40], strengthening their claims as candidate genes for CDH. Recurrent microdeletions of 8p23.1 that include GATA4 and sex determining region Y-box 7 (SOX7) are associated with a high risk of both CDH and cardiac defects [47]. Although Gata4-deficient mice showed both CDH and cardiac defects, humans with cardiac defects attributed to GATA4 mutations have not been reported to have CDH [47]. On the other hand, Wat et al. [47] revealed that haploinsufficiency of Sox7 or Gata4 is sufficient to produce anterior CDH in mice and that haploinsufficiency of SOX7 and GATA4 may each contribute to the development of CDH in patients with 8p23.1 deletions. After identification of a FRAS1-related extracellular matrix 1 (FREM1) deletion in a child with isolated left-sided posterolateral CDH that was covered by a membranous sac, Beck et al. [48] created a Frem1-deficient mouse model that exhibits a similar phenotype including a retrosternal diaphragmatic defect and decreased levels of cell proliferation in the anterior portion of the developing diaphragm, demonstrating that FREM1 deficiency can cause CDH in both humans and mice. Due to phenotypic overlaps between Frem1-deficient mice and mice that are deficient for the retinoic acid-responsive transcription factor Gata4, the authors performed further experiments, proving that Frem1 interacts genetically with Gata4 in the development of lung lobulation defects in this model [49].
c-Met and Fgf10
In addition to ZFPM2 and GATA4, several other candidate genes have been implicated in CDH pathogenesis, yielding more transgenic animal models and thus greater insight into CDH etiology. For instance, the mesenchymal-epithelial transition factor (c-Met) proto-oncogene codes for a receptor tyrosine kinase responsible for migration of muscle precursor cells into the diaphragm [50], while fibroblast growth factor 10 (Fgf10) is critical for early lung development [51]. Oral administration of nitrofen in Met−/− mice with amuscular diaphragms and Fgf10−/− mice with hypoplastic lungs induced CDH in both murine models, suggesting that diaphragmatic defects occur independent of myogenesis and lung formation [52].
Slit3, Lox, Pdgfra, Robo1/2 and Ndst1
As part of the Slit guidance ligand (SLIT) family of proteins responsible for axon crossing at the midline, homozygous Slit3-deficiency in mice causes failure of the central tendon region of the diaphragm to separate from the liver tissue, producing central (i.e. septum transversum) CDH [53, 54]. As a result, this specific model suffers from having the diaphragm defect in the ventral midline portion of the central tendon rather than in the posterolateral diaphragm. Other anomalies include renal and ureteric agenesis along with constant herniation of the liver and the gallbladder [54], which are uncommon in human CDH. Similarly, lysyl oxidase (Lox)−/−-mice were shown to have ruptured diaphragms due to fragmentation in the central tendon [55, 56]. On the other hand, while mice homozygous for null mutations in platelet-derived growth factor receptor α (Pdgfra) develop posterolateral diaphragmatic defects, they also present with a wide range of additional comorbidities including cardiac defects, renal and urogenital anomalies, facial clefts as well as pulmonary hypertension [57]. Roudabout (Robo) genes encode cell-surface receptors that have responsibility of their secreted ligands, Slit proteins, in various cellular processes [58,59,60]. The Slit-Robo signaling pathway has been demonstrated to play several key roles including neural crest cell migration and sensory ganglia morphogenesis, leukocyte chemotaxis, epithelial adhesion, embryonic and heart development as well as diaphragm and kidney formation [53, 54, 58, 61,62,63,64,65]. In fact, inactivation of Robo1 and Robo2 in mice leads to diaphragmatic malformation and mispositioning of the stomach in the thoracic instead of the abdominal cavity, which likely contributes to poor lung inflation and lethality at birth, reminiscent of CDH cases in humans [58]. Zhang et al. [66] have reported that ablation of the heparan sulfate biosynthetic enzyme N-deacetylase-N-sulfotransferase-1 (Ndst1) in mouse endothelium disrupts vascular development in the diaphragm, leading to hypoxia as well as subsequent diaphragmatic hypoplasia and central-type CDH. Interestingly, the phenotypes displayed in these mice resembled the developmental defects observed in Slit3 knockout mice. Furthermore, introduction of a heterozygous mutation in Robo4, the gene encoding the cognate receptor of Slit3, aggravated the defects in vascular development in the diaphragm and CDH [66]. Consequently, these results suggest that loss of Ndst1 causes defective diaphragm vascular development and CDH and that heparan sulfate facilitates the angiogenic Slit3-Robo4 signaling cascade during vascular development.
Conclusion and future directions
Experimental animal models of CDH have not only allowed us to study the pathophysiology and etiology of this relatively complex birth defect, but have also provided new insights into the molecular and biochemical basis, thus contributing to advances in the medical and surgical management. Hence, CDH animals in which this malformation occurs naturally are ideal models to investigate disease pathogenesis and associated pulmonary hypoplasia, as there is little or no interference to the animal prior to the study. Additionally, transgenic animal models of CDH not only mimic the natural occurrence of this condition, but also give a better understanding into the genes involved and how their modification might alter the course of the disease. Teratogen-induced CDH models although useful, have in turn the drawback of exposing the animals to a generalized noxious stimulus, which can result in widespread detrimental effects rather than simply targeting a specific organ system. The combination of transgenic animal models with regenerative tissue engineering and stem cell-based therapy may play a role in future CDH research by developing a myogenic patch capable of restoring muscle fraction in fetal diaphragmatic defects and promoting regeneration of hypoplastic lungs [67,68,69,70].
References
Balayla J, Abenhaim HA (2014) Incidence, predictors and outcomes of congenital diaphragmatic hernia: a population-based study of 32 million births in the United States. J Matern Fetal Neonatal Med 27:1438–1444
McGivern MR, Best KE, Rankin J, Wellesley D, Greenlees R, Addor MC et al (2015) Epidemiology of congenital diaphragmatic hernia in Europe: a register-based study. Arch Dis Child Fetal Neonatal Ed 100:F137–F144
Pober BR, Russell MK, Ackerman KG. (1993) Congenital Diaphragmatic Hernia Overview. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Mefford HC, et al., editors. GeneReviews(R). Seattle (WA)
Chandrasekharan PK, Rawat M, Madappa R, Rothstein DH, Lakshminrusimha S (2017) Congenital diaphragmatic hernia—a review. Matern Health Neonatol Perinatol 3:6
Keijzer R, Puri P (2010) Congenital diaphragmatic hernia. Semin Pediatr Surg 19:180–185
Wynn J, Krishnan U, Aspelund G, Zhang Y, Duong J, Stolar CJ et al (2013) Outcomes of congenital diaphragmatic hernia in the modern era of management. J Pediatr 163(114–119):e111
Zalla JM, Stoddard GJ, Yoder BA (2015) Improved mortality rate for congenital diaphragmatic hernia in the modern era of management: 15 year experience in a single institution. J Pediatr Surg 50:524–527
Kotecha S, Barbato A, Bush A, Claus F, Davenport M, Delacourt C et al (2012) Congenital diaphragmatic hernia. Eur Respir J 39:820–829
van Loenhout RB, Tibboel D, Post M, Keijzer R (2009) Congenital diaphragmatic hernia: comparison of animal models and relevance to the human situation. Neonatology 96:137–149
Barnhart DC, Jacques E, Scaife ER, Yoder BA, Meyers RL, Harman A et al (2012) Split abdominal wall muscle flap repair vs patch repair of large congenital diaphragmatic hernias. J Pediatr Surg 47:81–86
Nasr A, Struijs MC, Ein SH, Langer JC, Chiu PP (2010) Outcomes after muscle flap vs prosthetic patch repair for large congenital diaphragmatic hernias. J Pediatr Surg 45:151–154
Eastwood MP, Russo FM, Toelen J, Deprest J (2015) Medical interventions to reverse pulmonary hypoplasia in the animal model of congenital diaphragmatic hernia: a systematic review. Pediatr Pulmonol 50:820–838
Kardon G, Ackerman KG, McCulley DJ, Shen Y, Wynn J, Shang L et al (2017) Congenital diaphragmatic hernias: from genes to mechanisms to therapies. Dis Model Mech 10:955–970
Yu L, Sawle AD, Wynn J, Aspelund G, Stolar CJ, Arkovitz MS et al (2015) Increased burden of de novo predicted deleterious variants in complex congenital diaphragmatic hernia. Hum Mol Genet 24:4764–4773
Russell MK, Longoni M, Wells J, Maalouf FI, Tracy AA, Loscertales M et al (2012) Congenital diaphragmatic hernia candidate genes derived from embryonic transcriptomes. Proc Natl Acad Sci USA 109:2978–2983
Li E, Sucov HM, Lee KF, Evans RM, Jaenisch R (1993) Normal development and growth of mice carrying a targeted disruption of the alpha 1 retinoic acid receptor gene. Proc Natl Acad Sci USA 90:1590–1594
Lufkin T, Lohnes D, Mark M, Dierich A, Gorry P, Gaub MP et al (1993) High postnatal lethality and testis degeneration in retinoic acid receptor alpha mutant mice. Proc Natl Acad Sci USA 90:7225–7229
Lohnes D, Mark M, Mendelsohn C, Dolle P, Dierich A, Gorry P et al (1994) Function of the retinoic acid receptors (RARs) during development (I). Craniofacial and skeletal abnormalities in RAR double mutants. Development 120:2723–2748
Mendelsohn C, Lohnes D, Decimo D, Lufkin T, LeMeur M, Chambon P et al (1994) Function of the retinoic acid receptors (RARs) during development (II). Multiple abnormalities at various stages of organogenesis in RAR double mutants. Development 120:2749–2771
Mendelsohn C, Mark M, Dolle P, Dierich A, Gaub MP, Krust A et al (1994) Retinoic acid receptor beta 2 (RAR beta 2) null mutant mice appear normal. Dev Biol 166:246–258
Lohnes D, Mark M, Mendelsohn C, Dolle P, Decimo D, LeMeur M et al (1995) Developmental roles of the retinoic acid receptors. J Steroid Biochem Mol Biol 53:475–486
Andersen DH (1949) Effect of diet during pregnancy upon the incidence of congenital hereditary diaphragmatic hernia in the rat: failure to produce cystic fibrosis of the pancreas by maternal vitamin A deficiency. Am J Pathol 25:163–185
Andersen DH (1941) Incidence of congenital diaphragmatic hernia in the young of rats bred on a diet deficient in vitamin A. Am J Dis Child 62:888–889
Cooney AJ, Tsai SY, O’Malley BW, Tsai MJ (1992) Chicken ovalbumin upstream promoter transcription factor (COUP-TF) dimers bind to different GGTCA response elements, allowing COUP-TF to repress hormonal induction of the vitamin D3, thyroid hormone, and retinoic acid receptors. Mol Cell Biol 12:4153–4163
Kliewer SA, Umesono K, Heyman RA, Mangelsdorf DJ, Dyck JA, Evans RM (1992) Retinoid X receptor-COUP-TF interactions modulate retinoic acid signaling. Proc Natl Acad Sci USA 89:1448–1452
Tran P, Zhang XK, Salbert G, Hermann T, Lehmann JM, Pfahl M (1992) COUP orphan receptors are negative regulators of retinoic acid response pathways. Mol Cell Biol 12:4666–4676
You LR, Takamoto N, Yu CT, Tanaka T, Kodama T, Demayo FJ et al (2005) Mouse lacking COUP-TFII as an animal model of Bochdalek-type congenital diaphragmatic hernia. Proc Natl Acad Sci USA 102:16351–16356
Kreidberg JA, Sariola H, Loring JM, Maeda M, Pelletier J, Housman D et al (1993) WT-1 is required for early kidney development. Cell 74:679–691
Antonius T, van Bon B, Eggink A, van der Burgt I, Noordam K, van Heijst A (2008) Denys-Drash syndrome and congenital diaphragmatic hernia: another case with the 1097G > A(Arg366His) mutation. Am J Med Genet A 146A:496–499
Suri M, Kelehan P, O’Neill D, Vadeyar S, Grant J, Ahmed SF et al (2007) WT1 mutations in Meacham syndrome suggest a coelomic mesothelial origin of the cardiac and diaphragmatic malformations. Am J Med Genet A 143A:2312–2320
Clugston RD, Klattig J, Englert C, Clagett-Dame M, Martinovic J, Benachi A et al (2006) Teratogen-induced, dietary and genetic models of congenital diaphragmatic hernia share a common mechanism of pathogenesis. Am J Pathol 169:1541–1549
Carmona R, Cañete A, Cano E, Ariza L, Rojas A, Muñoz-Chápuli R (2016) Conditional deletion of WT1 in the septum transversum mesenchyme causes congenital diaphragmatic hernia in mice. Elife 5:e16009
Greer JJ (2013) Current concepts on the pathogenesis and etiology of congenital diaphragmatic hernia. Respir Physiol Neurobiol 189:232–240
Eppig JT, Blake JA, Bult CJ, Kadin JA, Richardson JE, Mouse Genome Database G (2015) The Mouse Genome Database (MGD): facilitating mouse as a model for human biology and disease. Nucleic Acids Res 43:D726–D736
Lu JR, Bassel-Duby R, Hawkins A, Chang P, Valdez R, Wu H et al (2002) Control of facial muscle development by MyoR and capsulin. Science 298:2378–2381
Villavicencio EH, Walterhouse DO, Iannaccone PM (2000) The sonic hedgehog-patched-gli pathway in human development and disease. Am J Hum Genet 67:1047–1054
Kim PC, Mo R, Hui Cc C (2001) Murine models of VACTERL syndrome: role of sonic hedgehog signaling pathway. J Pediatr Surg 36:381–384
Coles GL, Ackerman KG (2013) Kif7 is required for the patterning and differentiation of the diaphragm in a model of syndromic congenital diaphragmatic hernia. Proc Natl Acad Sci USA 110:E1898–E1905
Ackerman KG, Herron BJ, Vargas SO, Huang H, Tevosian SG, Kochilas L et al (2005) Fog2 is required for normal diaphragm and lung development in mice and humans. PLoS Genet 1:58–65
Holder AM, Klaassens M, Tibboel D, de Klein A, Lee B, Scott DA (2007) Genetic factors in congenital diaphragmatic hernia. Am J Hum Genet 80:825–845
Ackerman KG, Wang J, Luo L, Fujiwara Y, Orkin SH, Beier DR (2007) Gata4 is necessary for normal pulmonary lobar development. Am J Respir Cell Mol Biol 36:391–397
Doi T, Sugimoto K, Puri P (2009) Prenatal retinoic acid up-regulates pulmonary gene expression of COUP-TFII, FOG2, and GATA4 in pulmonary hypoplasia. J Pediatr Surg 44:1933–1937
Huggins GS, Bacani CJ, Boltax J, Aikawa R, Leiden JM (2001) Friend of GATA 2 physically interacts with chicken ovalbumin upstream promoter-TF2 (COUP-TF2) and COUP-TF3 and represses COUP-TF2-dependent activation of the atrial natriuretic factor promoter. J Biol Chem 276:28029–28036
Longoni M, Russell MK, High FA, Darvishi K, Maalouf FI, Kashani A et al (2015) Prevalence and penetrance of ZFPM2 mutations and deletions causing congenital diaphragmatic hernia. Clin Genet 87:362–367
Jay PY, Bielinska M, Erlich JM, Mannisto S, Pu WT, Heikinheimo M et al (2007) Impaired mesenchymal cell function in Gata4 mutant mice leads to diaphragmatic hernias and primary lung defects. Dev Biol 301:602–614
Merrell AJ, Ellis BJ, Fox ZD, Lawson JA, Weiss JA, Kardon G (2015) Muscle connective tissue controls development of the diaphragm and is a source of congenital diaphragmatic hernias. Nat Genet 47:496–504
Wat MJ, Beck TF, Hernandez-Garcia A, Yu Z, Veenma D, Garcia M et al (2012) Mouse model reveals the role of SOX7 in the development of congenital diaphragmatic hernia associated with recurrent deletions of 8p23.1. Hum Mol Genet 21:4115–4125
Beck TF, Veenma D, Shchelochkov OA, Yu Z, Kim BJ, Zaveri HP et al (2013) Deficiency of FRAS1-related extracellular matrix 1 (FREM1) causes congenital diaphragmatic hernia in humans and mice. Hum Mol Genet 22:1026–1038
Beck TF, Shchelochkov OA, Yu Z, Kim BJ, Hernández-García A, Zaveri HP et al (2013) Novel frem1-related mouse phenotypes and evidence of genetic interactions with gata4 and slit3. PLoS ONE 8:e58830
Bladt F, Riethmacher D, Isenmann S, Aguzzi A, Birchmeier C (1995) Essential role for the c-met receptor in the migration of myogenic precursor cells into the limb bud. Nature 376:768–771
Bellusci S, Grindley J, Emoto H, Itoh N, Hogan BL (1997) Fibroblast growth factor 10 (FGF10) and branching morphogenesis in the embryonic mouse lung. Development 124:4867–4878
Babiuk RP, Greer JJ (2002) Diaphragm defects occur in a CDH hernia model independently of myogenesis and lung formation. Am J Physiol Lung Cell Mol Physiol 283:L1310–L1314
Yuan W, Rao Y, Babiuk RP, Greer JJ, Wu JY, Ornitz DM (2003) A genetic model for a central (septum transversum) congenital diaphragmatic hernia in mice lacking Slit3. Proc Natl Acad Sci USA 100:5217–5222
Liu J, Zhang L, Wang D, Shen H, Jiang M, Mei P et al (2003) Congenital diaphragmatic hernia, kidney agenesis and cardiac defects associated with Slit3-deficiency in mice. Mech Dev 120:1059–1070
Hornstra IK, Birge S, Starcher B, Bailey AJ, Mecham RP, Shapiro SD (2003) Lysyl oxidase is required for vascular and diaphragmatic development in mice. J Biol Chem 278:14387–14393
Maki JM, Sormunen R, Lippo S, Kaarteenaho-Wiik R, Soininen R, Myllyharju J (2005) Lysyl oxidase is essential for normal development and function of the respiratory system and for the integrity of elastic and collagen fibers in various tissues. Am J Pathol 167:927–936
Bleyl SB, Moshrefi A, Shaw GM, Saijoh Y, Schoenwolf GC, Pennacchio LA et al (2007) Candidate genes for congenital diaphragmatic hernia from animal models: sequencing of FOG2 and PDGFRalpha reveals rare variants in diaphragmatic hernia patients. Eur J Hum Genet 15:950–958
Domyan ET, Branchfield K, Gibson DA, Naiche LA, Lewandoski M, Tessier-Lavigne M et al (2013) Roundabout receptors are critical for foregut separation from the body wall. Dev Cell 24:52–63
Long H, Sabatier C, Ma L, Plump A, Yuan W, Ornitz DM et al (2004) Conserved roles for Slit and Robo proteins in midline commissural axon guidance. Neuron 42:213–223
Ypsilanti AR, Zagar Y, Chedotal A (2010) Moving away from the midline: new developments for Slit and Robo. Development 137:1939–1952
De Bellard ME, Rao Y, Bronner-Fraser M (2003) Dual function of Slit2 in repulsion and enhanced migration of trunk, but not vagal, neural crest cells. J Cell Biol 162:269–279
Shiau CE, Bronner-Fraser M (2009) N-cadherin acts in concert with Slit1-Robo2 signaling in regulating aggregation of placode-derived cranial sensory neurons. Development 136:4155–4164
Ye BQ, Geng ZH, Ma L, Geng JG (2010) Slit2 regulates attractive eosinophil and repulsive neutrophil chemotaxis through differential srGAP1 expression during lung inflammation. J Immunol 185:6294–6305
Macias H, Moran A, Samara Y, Moreno M, Compton JE, Harburg G et al (2011) SLIT/ROBO1 signaling suppresses mammary branching morphogenesis by limiting basal cell number. Dev Cell 20:827–840
Grieshammer U, Le M, Plump AS, Wang F, Tessier-Lavigne M, Martin GR (2004) SLIT2-mediated ROBO2 signaling restricts kidney induction to a single site. Dev Cell 6:709–717
Zhang B, Xiao W, Qiu H, Zhang F, Moniz HA, Jaworski A et al (2014) Heparan sulfate deficiency disrupts developmental angiogenesis and causes congenital diaphragmatic hernia. J Clin Invest 124:209–221
De Coppi P, Deprest J (2017) Regenerative medicine solutions in congenital diaphragmatic hernia. Semin Pediatr Surg 26:171–177
Shieh HF, Graham CD, Brazzo JA 3rd, Zurakowski D, Fauza DO (2017) Comparisons of human amniotic mesenchymal stem cell viability in FDA-approved collagen-based scaffolds: implications for engineered diaphragmatic replacement. J Pediatr Surg 52:1010–1013
DeKoninck P, Toelen J, Roubliova X, Carter S, Pozzobon M, Russo FM et al (2015) The use of human amniotic fluid stem cells as an adjunct to promote pulmonary development in a rabbit model for congenital diaphragmatic hernia. Prenat Diagn 35:833–840
Jeanty C, Kunisaki SM, MacKenzie TC (2014) Novel non-surgical prenatal approaches to treating congenital diaphragmatic hernia. Semin Fetal Neonatal Med 19:349–356
Acknowledgements
Open Access funding provided by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nakamura, H., Doi, T., Puri, P. et al. Transgenic animal models of congenital diaphragmatic hernia: a comprehensive overview of candidate genes and signaling pathways. Pediatr Surg Int 36, 991–997 (2020). https://doi.org/10.1007/s00383-020-04705-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-020-04705-0