Abstract
Introduction
Recent studies suggest that some of the post-surgical morbidity in Hirschsprung disease (HSCR) is due to enteric nervous system structural defects in the proximal, ganglionated bowel that remains after surgery. We hypothesized that resection margin histology would predict intermediate-term outcomes in HSCR patients.
Methods
Following IRB approval, HSCR patients with rectosigmoid disease born between 2009 and 2016 were reviewed and tissue blocks were obtained for new analyses. Proximal resection margins were analyzed for ganglion size, Hu + neurons/ganglion, and % nitric oxide synthase (NOS) neurons/ganglion as compared to control (non-HSCR) patient samples. Chart reviews were performed for 1- and 2-year outcomes. Patients were contacted for survey to determine Rintala bowel function score.
Results
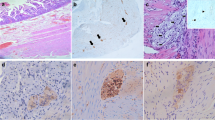
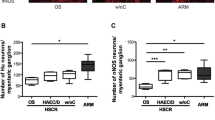
45 patients had recto-sigmoid disease and were further analyzed. HSCR patients had significantly smaller individual ganglion size (4533 μm2, range 1744–16,287 vs. 6492 μm2, range 1932–30,838, p = 0.0192) and fewer HuC/D + neurons per ganglion (15, range 5.2–34 vs. 21, range 5.2–6.7, p = 0.0214). HSCR patients demonstrated a markedly increased percentage of NOS (relaxation neurotransmitter) neurons (50, range 22–85 vs. 37, range 16–80, p = 0.0266). None of the histology measures correlated with presence/absence of constipation at 1–2 year follow-up (p = NS). However, smaller ganglion size and higher percentage of NOS neurons correlated with decreased patient-reported quality of life (r = 0.3838, r = − 0.1809).
Conclusion
1–2 year follow-up may be insufficient to determine if resection margin histology correlates with outcomes. Patient-reported quality of life surveys, although limited in number, suggest that neurotransmitter imbalance at the resection margin may predict poor outcomes in HSCR patients. This study supports the concept that the ganglionated portion of the remaining colon post-surgery may not sustain normal bowel function.



Similar content being viewed by others
References
Furness JB (2008) The enteric nervous system: normal functions and enteric neuropathies. Neurogastroenterol Motil 20(Suppl 1):32–38
Heuckeroth RO (2018) Hirschsprung disease—integrating basic science and clinical medicine to improve outcomes. Nat Rev Gastroenterol Hepatol 27:1
Swenson O, Bill AH (1948) Resection of rectum and rectosigmoid with preservation of the sphincter for benign spastic lesions producing megacolon; an experimental study. Surgery 24:212–220
Jarvi K, Laitakari EM, Koivusalo A, Rintala RJ, Pakarinen MP (2010) Bowel function and gastrointestinal quality of life among adults operated for Hirschsprung disease during childhood: a population-based study. Ann Surg 252:977–981
Zaitoun I, Erickson CS, Barlow AJ, Klein TR, Heneghan AF, Pierre JF, Epstein ML, Gosain A (2013) Altered neuronal density and neurotransmitter expression in the ganglionated region of Ednrb null mice: implications for Hirschsprung's disease. Neurogastroenterol Motil 25:e233–244
Cheng LS, Schwartz DM, Hotta R, Graham HK, Goldstein AM (2016) Bowel dysfunction following pullthrough surgery is associated with an overabundance of nitrergic neurons in Hirschsprung disease. J Pediatr Surg 51:1834–1838
Coyle D, O'Donnell AM, Gillick J, Puri P (2016) Altered neurotransmitter expression profile in the ganglionic bowel in Hirschsprung's disease. J Pediatr Surg 51:762–769
Veras LV, Arnold M, Avansino JR, Bove K, Cowles RA, Durham MM, Goldstein AM, Krishnan C, Langer JC, Levitt M, Monforte-Munoz H, Rabah R, Reyes-Mugica M, Rollins MD 2nd, Kapur RP, Gosain A; American Pediatric Surgical Association Hirschsprung Disease Interest Group (2019) Guidelines for synoptic reporting of surgery and pathology in Hirschsprung disease. J Pediatr Surg. 54(10):2017–2023
Rintala RJ, Lindahl H (1995) Is normal bowel function possible after repair of intermediate and high anorectal malformations? J Pediatr Surg 30:491–494
Zhang J, Ma T, Peng Y, Huang G, Liu F (2017) A 5-year follow-up study of neonates with Hirschsprung's disease undergoing transanal Soave or Swenson surgery. Patient Prefer Adherence 11:1957–1961
Kyrklund K, Neuvonen MI, Pakarinen MP, Rintala RJ (2018) Social morbidity in relation to bowel functional outcomes and quality of life in anorectal malformations and Hirschsprung's disease. Eur J Pediatr Surg 28:522–528
McKenna SP (2011) Measuring patient-reported outcomes: moving beyond misplaced common sense to hard science. BMC Med 9:86
Acknowledgements
The authors would like to thank Cindy Lazar (Histology Manager, Methodist Le Bonheur Healthcare, Memphis, TN) for her assistance in obtaining archived specimens for our analysis.
Funding
This work was supported by grants from the National Institutes of Health, USA (K08DK098271 to AG, R03DK114543 to AG, R01DK125047 to AG, T35DK113964 to LB and KLF), American College of Surgeons, USA (George H.A. Clowes Career Development Award to AG), and the Alpha Omega Alpha Carolyn L. Kuckein Student Research Fellowship (to KLF).
Author information
Authors and Affiliations
Contributions
Conception and design of the study: LVV, MF, AG; Acquisition of data: LB, KLF, LVV, MF; Analysis and interpretation of data: LB, KLF, LVV, MF, AG; Drafting/Revision the article: LB, KLF, AG; Final approval: all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the University of Tennessee Health Science Center Institutional Review Board approval (16-04806-XP) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
The University of Tennessee Health Science Center Institutional Review Board granted waiver of informed consent and HIPAA authorization for the collection of data for the study in accord with the criteria and review procedures specified at 45 CFR 164.512(i)(2).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brooks, L.A., Fowler, K.L., Veras, L.V. et al. Resection margin histology may predict intermediate-term outcomes in children with rectosigmoid Hirschsprung disease. Pediatr Surg Int 36, 875–882 (2020). https://doi.org/10.1007/s00383-020-04689-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-020-04689-x