Abstract
Background
Preoperative factors have been correlated with pre-incision hypotension (PIH) in children undergoing surgery, suggesting that PIH can be predicted through preoperative screening. We studied blood pressure (BP) changes in the 12 min following the induction of anesthesia to study the incidence of post-induction hypotension and to assess the feasibility of predicting PIH in low-risk children without preoperative hypotension or comorbid features.
Methods
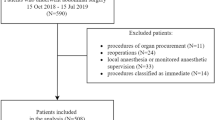
We retrospectively evaluated 200 patients ranging in age from 2 to 8 years with American Society of Anesthesiologists’ (ASA) physical status I or II, undergoing non-cardiac surgery. Patients were excluded if they had preoperative (baseline) hypotension (systolic blood pressure (SBP) < 5th percentile for age). BP and heart rate (HR) were recorded at 3 min intervals for 12 min after the induction of anesthesia. Pre-incision hypotension (PIH) was initially defined as SBP < 5th percentile for age: (1) at any timepoint within 12 min of induction; (2) for the median SBP obtained during the 12 min study period; or (3) at 2 or more timepoints including the final point at 12 min after the induction of anesthesia (sustained hypotension). In addition, we examined PIH defined as > 20% decrease in SBP from baseline: (4) at any timepoint within 12 min of the induction of anesthesia; (5) for the median SBP obtained during the 12 min study period; or (6) at two or more timepoints including the final point at 12 min after the induction of anesthesia. Agreement among the six definitions was analyzed, in addition to the effects of age, gender, type of anesthetic induction, use of premedication, preoperative BP, preoperative HR, and body mass index on the incidence of PIH according to each definition.
Results
Five patients were excluded due to baseline hypotension and six were excluded for missing data. In the remaining cohort, estimated PIH prevalence ranged from 4% [definition (Stewart et al., in Paediatr Anaesth 26:844–851, 2016), sustained PIH according to SBP percentile-for-age] to 57% [definition (Task Force on Blood Pressure Control in Children, in Pediatrics 79:1–25, 1987), at least one timepoint where SBP was > 20% lower than baseline]. Pairwise agreement among the six definitions ranged from 49 to 91% agreement. No sequelae of PIH were noted during subsequent anesthetic or postoperative care. On multivariable analysis, no covariates were consistently associated with PIH risk across all six definitions of PIH.
Conclusion
The present study describes the incidence and prediction of PIH in a cohort of relatively healthy children. In this setting, accurate prediction of PIH appears to be hampered by lack of agreement between definitions of PIH. Overall, there was a low PIH incidence when the threshold of SBP < 5th percentile for age was used.
Level of evidence
II.
Similar content being viewed by others
References
Nafiu OO, Kheterpal S, Morris M, Reynolds PI, Malviya S, Tremper KK (2009) Incidence and risk factors for preincision hypotension in a noncardiac pediatric surgical population. Paediatr Anaesth 19:232–239
Nafiu OO, Maclean S, Blum J, Kheterpal S, Cowan A, Tremper KK (2010) High BMI in children as a risk factor for intraoperative hypotension. Eur J Anaesthesiol 27:1065–1068
Stewart M, Scattoloni J, Tazhibi G, Nafiu OO (2016) Association of elevated preoperative blood pressure with preincision hypotension in pediatric surgical patients. Paediatr Anaesth 26:844–851
Task Force on Blood Pressure Control in Children (1987) Report of the second task force on blood pressure control in children—1987. National Heart, Lung, and Blood Institute, Bethesda, Maryland. Pediatrics 79:1–25
Coates BM, Vavilala MS, Mack CD, Muangman S, Suz P, Sharar SR, Bulger E, Lam AM (2005) Influence of definition and location of hypotension on outcome following severe pediatric traumatic brain injury. Crit Care Med 33:2645–2650
Nafiu OO, Voepel-Lewis T, Morris M, Chimbra WT, Malviya S, Reynolds PI, Tremper KK (2009) How do pediatric anesthesiologists define intraoperative hypotension. Paediatr Anaesth 19:1048–1053
Guidelines for Prehospital Management of TBI. 2nd edn. http://braintrauma.org/uploads/Prehospital_Guidelines_2nd_Edition_2.pdf
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114(2 Suppl 4th Report):555–576
Child growth standards. http://www.who.int/childgrowth/standards/weight for age/en
Viera AJ, Garrett JM (2005) Understanding interobserver agreement: the kappa statistic. Fam Med 37:360–363
Feigl EO, Neat GW, Huang AH (1990) Interrelations between coronary artery pressure, myocardial metabolism and coronary blood flow. J Mol Cell Cardiol 22:375–390
Bonventre JV, Weinberg JM (2003) Recent advances in the pathophysiology of ischemic acute renal failure. J Am Soc Nephrol 14:2199–2210
Munshi R, Hsu C, Himmelfarb J (2011) Advances in understanding ischemic acute kidney injury. BMC Med 9:11–13
McCann ME, Schouten ANJ, Dobija N (2014) Infantile postoperative encephalopathy: perioperative factors as a cause for concern. Pediatrics 133:751–757
Brady K, Hogue CW (2013) Intraoperative hypotension and patient outcome: Does “one size fit all?” Anesthesiology 119:495–497
Horan MJ (1987) Task force on blood pressure control in children, report of the second task force on blood pressure in children. Pediatrics 79:1–7
Bijker JB, van Klei WA, Kappen TH, Wolfswinkel LV, Moons KG, Kalkman CJ (2007) Incidence of Intraoperative hypotension as a function of the chosen definition: Literature definitions applied to a retrospective cohort using automated data collection. Anesthesiology 107:213–220
Davis PJ, Galinkin J, McGowan FX, Lynn AM, Yaster M, Rabb MF, Krane EJ, Kurth CD, Blum RH, Maxwell L, Orr R (2001) A randomized multicenter study of remifentanil compared with halothane in neonates and infants undergoing pyloromyotomy: Emergence and recovery profiles. Anesth Analg 93:1380–1386
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author Tariq M. Wani declares he has no conflict of interest. Author Mohammed Hakim declares he has no conflict of interest. Author Archana Ramesh declares she has no conflict of interest. Author Shabina Rehman declares he has no conflict of interest. Yaseer Majid declares he has no conflict of interest. Rebecca Miller declares she has no conflict of interest. Dmitry Tumin declares he has no conflict of interest. Joseph D. Tobias declares he has no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Wani, T.M., Hakim, M., Ramesh, A. et al. Risk factors for post-induction hypotension in children presenting for surgery. Pediatr Surg Int 34, 1333–1338 (2018). https://doi.org/10.1007/s00383-018-4359-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-018-4359-5