Abstract
Purpose
The aim of the study was to evaluate established risk factors and define new inflammation-associated factors associated with postoperative ventriculoperitoneal shunt placement.
Methods
The electronic medical records of children who underwent surgery for a tumor in the posterior fossa between January 2009 and January 2018 were retrospectively analyzed. Factors evaluated include age, clinical symptoms, tumor type, extent of surgical tumor resection, treatment with EVD and/or ETV, radiological findings, postoperative serum CRP, and leucocyte levels. Tumor tissue was stained immunohistochemically with antibodies against CD3, and leucocyte counts were performed. Patients with pre- or postoperative signs of infection or confirmation of a concurrent infection were excluded from some analyses.
Results
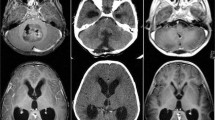
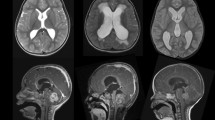
Seventy patients ages 0.4–20.8 years (median, 8.2) were included. Forty-five of 70 (65.3%) presented postoperative radiological signs of hydrocephalus. Fifteen of 70 (21.4%) patients required shunt placement postoperatively. Shunt placement was significantly associated with age < 3 years at diagnosis (p = 0.013), perioperative EVD placement (p < 0.001), signs of hydrocephalus in postoperative imaging (p = 0.047), a frontooccipital horn ratio (FOHR) > 0.46 within the first 72 h postoperatively (p < 0.001), and the presence of intraventricular blood postoperatively (p = 0.007). Six patients who underwent shunting had serum CRP levels > 40 mg/l (p = 0.030) within the first 48 h postoperatively. Tumor type or extent of resection did not correlate with shunt placement.
Conclusions
Several established and new factors associated with shunt placement after posterior fossa tumor surgery could be identified. Additional studies are needed to explore the aseptic inflammation pathways involved with increased CRP levels and shunt placement.



Similar content being viewed by others
References
Ahmann PA, Lazzara A, Dykes FD, Brann AW Jr, Schwartz JF (1980) Intraventricular hemorrhage in the high-risk preterm infant: incidence and outcome. Ann Neurol 7:118–124. https://doi.org/10.1002/ana.410070205
Bhatia R, Tahir M, Chandler CL (2009) The management of hydrocephalus in children with posterior fossa tumours: the role of pre-resectional endoscopic third ventriculostomy. Pediatr Neurosurg 45:186–191. https://doi.org/10.1159/000222668
Bognar L, Borgulya G, Benke P, Madarassy G (2003) Analysis of CSF shunting procedure requirement in children with posterior fossa tumors. Childs Nerv Syst 19:332–336. https://doi.org/10.1007/s00381-003-0745-x
Chaplin ER, Goldstein GW, Myerberg DZ, Hunt JV, Tooley WH (1980) Posthemorrhagic hydrocephalus in the preterm infant. Pediatrics 65:901–909
Chaudhry SR, Stoffel-Wagner B, Kinfe TM, Guresir E, Vatter H, Dietrich D, Lamprecht A, Muhammad S (2017) Elevated systemic IL-6 levels in patients with aneurysmal subarachnoid hemorrhage is an unspecific marker for post-SAH complications. Int J Mol Sci 18. https://doi.org/10.3390/ijms18122580
Chen Q, Feng Z, Tan Q, Guo J, Tang J, Tan L, Feng H, Chen Z (2017) Post-hemorrhagic hydrocephalus: recent advances and new therapeutic insights. J Neurol Sci 375:220–230. https://doi.org/10.1016/j.jns.2017.01.072
Culley DJ, Berger MS, Shaw D, Geyer R (1994) An analysis of factors determining the need for ventriculoperitoneal shunts after posterior fossa tumor surgery in children. Neurosurgery 34:402–407 discussion 407-408
de Ribaupierre S, Rilliet B, Vernet O, Regli L, Villemure JG (2007) Third ventriculostomy vs ventriculoperitoneal shunt in pediatric obstructive hydrocephalus: results from a Swiss series and literature review. Childs Nerv Syst 23:527–533. https://doi.org/10.1007/s00381-006-0283-4
Dewan MC, Lim J, Shannon CN, Wellons JC 3rd (2017) The durability of endoscopic third ventriculostomy and ventriculoperitoneal shunts in children with hydrocephalus following posterior fossa tumor resection: a systematic review and time-to-failure analysis. J Neurosurg Pediatr 19:1–7. https://doi.org/10.3171/2017.1.peds16536
Di Rocco F, Jucá CE, Zerah M, Sainte-Rose C (2013) Endoscopic third ventriculostomy and posterior fossa tumors. World Neurosurg 79(2 Suppl):15–19
Dias MS, Albright AL (1989) Management of hydrocephalus complicating childhood posterior fossa tumors. Pediatr Neurosci 15:283–289; discussion 290
Due-Tonnessen BJ, Helseth E (2007) Management of hydrocephalus in children with posterior fossa tumors: role of tumor surgery. Pediatr Neurosurg 43:92–96. https://doi.org/10.1159/000098379
El Beltagy MA, Kamal HM, Taha H, Awad M, El Khateeb N (2010) Endoscopic third ventriculostomy before tumor surgery in children with posterior fossa tumors, CCHE experience. Childs Nerv Syst 26:1699–1704
Foreman P, Mc-Clugage S 3rd, Naftel R, Griessenauer CJ, Ditty BJ, Agee BS, Riva-Cambrin J, Wellons J 3rd (2013) Validation and modification of a predictive model of postresection hydrocephalus in pediatric patients with posterior fossa tumors. J Neurosurg Pediatr 12:220–226. https://doi.org/10.3171/2013.5.peds1371
Gopalakrishnan CV, Dhakoji A, Menon G, Nair S (2012) Factors predicting the need for cerebrospinal fluid diversion following posterior fossa tumor surgery in children. Pediatr Neurosurg 48:93–101. https://doi.org/10.1159/000343009
Gram M, Sveinsdottir S, Cinthio M, Sveinsdottir K, Hansson SR, Morgelin M, Akerstrom B, Ley D (2014) Extracellular hemoglobin - mediator of inflammation and cell death in the choroid plexus following preterm intraventricular hemorrhage. J Neuroinflammation 11:200. https://doi.org/10.1186/s12974-014-0200-9
Habiyaremye G, Morales DM, Morgan CD, McAllister JP, CreveCoeur TS, Han RH, Gabir M, Baksh B, Mercer D, Limbrick DD Jr (2017) Chemokine and cytokine levels in the lumbar cerebrospinal fluid of preterm infants with post-hemorrhagic hydrocephalus. Fluids Barriers CNS 14:35. https://doi.org/10.1186/s12987-017-0083-0
Juvela S, Kuhmonen J, Siironen J (2012) C-reactive protein as predictor for poor outcome after aneurysmal subarachnoid haemorrhage. Acta Neurochir 154:397–404. https://doi.org/10.1007/s00701-011-1243-7
Karimy JK, Zhang J, Kurland DB, Theriault BC, Duran D, Stokum JA, Furey CG, Zhou X, Mansuri MS, Montejo J, Vera A, DiLuna ML, Delpire E, Alper SL, Gunel M, Gerzanich V, Medzhitov R, Simard JM, Kahle KT (2017) Inflammation-dependent cerebrospinal fluid hypersecretion by the choroid plexus epithelium in posthemorrhagic hydrocephalus. Nat Med 23:997–1003. https://doi.org/10.1038/nm.4361
Kestle JR, Riva-Cambrin J, Wellons JC 3rd, Kulkarni AV, Whitehead WE, Walker ML, Oakes WJ, Drake JM, Luerssen TG, Simon TD, Holubkov R, Hydrocephalus Clinical Research N (2011) A standardized protocol to reduce cerebrospinal fluid shunt infection: the Hydrocephalus Clinical Research Network Quality Improvement Initiative. J Neurosurg Pediatr 8:22–29. https://doi.org/10.3171/2011.4.PEDS10551
Killer M, Arthur A, Al-Schameri AR, Barr J, Elbert D, Ladurner G, Shum J, Cruise G (2010) Cytokine and growth factor concentration in cerebrospinal fluid from patients with hydrocephalus following endovascular embolization of unruptured aneurysms in comparison with other types of hydrocephalus. Neurochem Res 35:1652–1658. https://doi.org/10.1007/s11064-010-0226-z
Kulkarni AV, Riva-Cambrin J, Butler J, Browd SR, Drake JM, Holubkov R, Kestle JR, Limbrick DD, Simon TD, Tamber MS, Wellons JC 3rd, Whitehead WE, Hydrocephalus Clinical Research N (2013) Outcomes of CSF shunting in children: comparison of Hydrocephalus Clinical Research Network cohort with historical controls. clinical article J Neurosurg Pediatr 12:334–338. https://doi.org/10.3171/2013.7.PEDS12637
Kulkarni AV, Riva-Cambrin J, Holubkov R, Browd SR, Cochrane DD, Drake JM, Limbrick DD, Rozzelle CJ, Simon TD, Tamber MS, Wellons JC 3rd, Whitehead WE, Kestle JR (2016) Endoscopic third ventriculostomy in children: prospective, multicenter results from the Hydrocephalus Clinical Research Network. J Neurosurg Pediatr 18:423–429. https://doi.org/10.3171/2016.4.peds163
Kumar V, Phipps K, Harkness W, Hayward RD (1996) Ventriculo-peritoneal shunt requirement in children with posterior fossa tumours: an 11-year audit. Br J Neurosurg 10:467–470
Lee M, Wisoff JH, Abbott R, Freed D, Epstein FJ (1994) Management of hydrocephalus in children with medulloblastoma: prognostic factors for shunting. Pediatr Neurosurg 20:240–247. https://doi.org/10.1159/000120797
Merchant TE, Fouladi M (2005) Ependymoma: new therapeutic approaches including radiation and chemotherapy. J Neuro-Oncol 75:287–299. https://doi.org/10.1007/s11060-005-6753-9
Morelli D, Pirotte B, Lubansu A, Detemmerman D, Aeby A, Fricx C, Berre J, David P, Brotchi J (2005) Persistent hydrocephalus after early surgical management of posterior fossa tumors in children: is routine preoperative endoscopic third ventriculostomy justified? J Neurosurg 103:247–252. https://doi.org/10.3171/ped.2005.103.3.0247
Naureen I, Waheed Kh A, Rathore AW, Victor S, Mallucci C, Goodden JR, Chohan SN, Miyan JA (2014) Fingerprint changes in CSF composition associated with different aetiologies in human neonatal hydrocephalus: inflammatory cytokines. Childs Nerv Syst 30:1155–1164. https://doi.org/10.1007/s00381-014-2415-6
O’Hayon BB, Drake JM, Ossip MG, Tuli S, Clarke M (1998) Frontal and occipital horn ratio: a linear estimate of ventricular size for multiple imaging modalities in pediatric hydrocephalus. Pediatr Neurosurg 29:245–249 doi:28730
Papo I, Caruselli G, Luongo A (1982) External ventricular drainage in the management of posterior fossa tumors in children and adolescents. Neurosurgery 10:13–15
Rekate HL (2008) Shunt-related headaches: the slit ventricle syndromes. Childs Nerv Syst 24:423–430. https://doi.org/10.1007/s00381-008-0579-7
Riva-Cambrin J, Detsky AS, Lamberti-Pasculli M, Sargent MA, Armstrong D, Moineddin R, Cochrane DD, Drake JM (2009) Predicting postresection hydrocephalus in pediatric patients with posterior fossa tumors. J Neurosurg Pediatr 3:378–385. https://doi.org/10.3171/2009.1.PEDS08298
Ruggiero C, Cinalli G, Spennato P, Aliberti F, Cianciulli E, Trischitta V, Maggi G (2004) Endoscopic third ventriculostomy in the treatment of hydrocephalus in posterior fossa tumors in children. Childs Nerv Syst 20:828–833. https://doi.org/10.1007/s00381-004-0938-y
Sainte-Rose C, Cinalli G, Roux FE, Maixner R, Chumas PD, Mansour M, Carpentier A, Bourgeois M, Zerah M, Pierre-Kahn A, Renier D (2001) Management of hydrocephalus in pediatric patients with posterior fossa tumors: the role of endoscopic third ventriculostomy. J Neurosurg 95:791–797
Santos de Oliveira R, Barros Juca CE, Valera ET, Machado HR (2008) Hydrocephalus in posterior fossa tumors in children. Are there factors that determine a need for permanent cerebrospinal fluid diversion? Childs Nerv Syst 24:1397–1403. https://doi.org/10.1007/s00381-008-0649-x
Savman K, Blennow M, Hagberg H, Tarkowski E, Thoresen M, Whitelaw A (2002) Cytokine response in cerebrospinal fluid from preterm infants with posthaemorrhagic ventricular dilatation. Acta Paediatr 91:1357–1363
Schmid UD, Seiler RW (1986) Management of obstructive hydrocephalus secondary to posterior fossa tumors by steroids and subcutaneous ventricular catheter reservoir. J Neurosurg 65:649–653. https://doi.org/10.3171/jns.1986.65.5.0649
Schneider C, Ramaswamy V, Kulkarni AV, Rutka JT, Remke M, Tabori U, Hawkins C, Bouffet E, Taylor MD (2015) Clinical implications of medulloblastoma subgroups: incidence of CSF diversion surgery. J Neurosurg Pediatr 15:236–242. https://doi.org/10.3171/2014.9.PEDS14280
Tamburrini G, Pettorini BL, Massimi L, Caldarelli M, Di Rocco C (2008) Endoscopic third ventriculostomy: the best option in the treatment of persistent hydrocephalus after posterior cranial fossa tumour removal? Childs Nerv Syst 24:1405–1412. https://doi.org/10.1007/s00381-008-0699-0
Wang L, Gao Z (2018) Expression of MMP-9 and IL-6 in patients with subarachnoid hemorrhage and the clinical significance. Exp Ther Med 15:1510–1514. https://doi.org/10.3892/etm.2017.5553
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Helmbold, L.J., Kammler, G., Regelsberger, J. et al. Predictive factors associated with ventriculoperitoneal shunting after posterior fossa tumor surgery in children. Childs Nerv Syst 35, 779–788 (2019). https://doi.org/10.1007/s00381-019-04136-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-019-04136-w