Abstract
Introduction
Complications following cranioplasty with either autografts or cranial implants are commonly reported in pediatric patients. However, data regarding cranioplasty strategies, complications and long-term outcomes are not well described. This study systematically reviews the literature for an overview of current cranioplasty practice in children.
Methods
A systematic review of articles published from inception to July 2018 was performed. Studies were included if they reported the specific use of cranioplasty materials following craniectomy in patients younger than 18 years of age, and had a minimum follow-up of at least 1 year.
Results
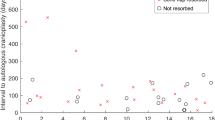
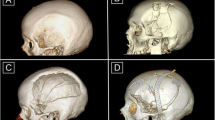
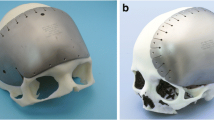
Twenty-four manuscripts, describing a total of 864 cranioplasty procedures, met the inclusion criteria. The age of patients in this aggregate ranged from 1 month to 20 years and the weighted average was 8.0 years. The follow-up ranged from 0.4 months to 18 years and had a weighted average of 40.4 months. Autologous bone grafts were used in 484 cases (56.0%). Resorption, infection and/or hydrocephalus were the most frequently mentioned complications. In this aggregate group, 61 patients needed a revision cranioplasty. However, in 6/13 (46%) papers studying autologous cranioplasties, no data was provided on resorption, infection and revision cranioplasty rates. Cranial implants were used in 380 cases (44.0%), with custom-made porous hydroxyapatite being the most commonly used material (100/380, 26.3%). Infection and migration/fracturing/loosening were the most frequently documented complications. Eleven revision cranioplasties were reported. Again, no data was reported on infection and revision cranioplasty rates, in 7/16 (44%) and 9/16 (56%) of papers, respectively.
Conclusion
Our systematic review illuminates that whether autografts or cranial implants are used, postcranioplasty complications are quite common. Beyond this, the existing literature does not contain well documented and comparable outcome parameters, suggesting that prospective, long-term multicenter cohort studies are needed to be able to optimize cranioplasty strategies in children who will undergo cranioplasty following craniectomy.

Similar content being viewed by others
References
Arnaud E (2000) Advances in cranioplasty with osteoinductive biomaterials: summary of experimental studies and clinical prospects. Childs Nerv Syst 16:659–668. https://doi.org/10.1007/s003810000321
Artico M, Ferrante L, Pastore FS, Ramundo EO, Cantarelli D, Scopelliti D (2003) Bone autografting of the calvaria and craniofacial skeleton: historical background, surgical results in a series of 15 patients, and review of the literature. Surg Neurol 60:71–79
Aydin S, Kucukyuruk B, Abuzayed B, Aydin S, Sanus GZ (2011) Cranioplasty: review of materials and techniques. J Neurosci Rural Pract 2:162–167. https://doi.org/10.4103/0976-3147.83584
Blum KS, Schneider SJ, Rosenthal AD (1997) Methyl methacrylate cranioplasty in children: long-term results. Pediatr Neurosurg 26:33–35. https://doi.org/10.1159/000121158
Bowers CA, McMullin JH, Brimley C, Etherington L, Siddigi FA, Riva-Cambrin J (2015) Minimizing bone gaps when using custom pediatric cranial implants is associated with implant success. J Neurosurg Pediatr 16:439–444. https://doi.org/10.3171/2015.2.PEDS14536
Bowers CA, Riva-Cambrin J, Hertzler DA 2nd, Walker ML (2013) Risk factors and rates of bone flap resorption in pediatric patients after decompressive craniectomy for traumatic brain injury. J Neurosurg Pediatr 11:526–532. https://doi.org/10.3171/2013.1.PEDS12483
Chang V, Hartzfeld P, Langlois M, Mahmood A, Seyfried D (2010) Outcomes of cranial repair after craniectomy. J Neurosurg 112:1120–1124. https://doi.org/10.3171/2009.6.JNS09133
Chao MT, Jiang S, Smith D, DeCesare GE, Cooper GM, Pollack IF, Girotto J, Losee JE (2009) Demineralized bone matrix and resorbable mesh bilaminate cranioplasty: a novel method for reconstruction of large-scale defects in the pediatric calvaria. Plast Reconstr Surg 123:976–982. https://doi.org/10.1097/PRS.0b013e31819ba46f
Choi SH, Levy ML, McComb JG (1998) A method of cranioplasty using coralline hydroxyapatite. Pediatr Neurosurg 29:324–327. https://doi.org/10.1159/000028747
Cohen AJ, Dickerman RD, Schneider SJ (2004) New method of pediatric cranioplasty for skull defect utilizing polyactic acid absorbable plates and carbonated apatite bone cement. J Craniofac Surg 15:469–472
Costantino PD, Chaplin JM, Wolpoe ME, Catalano PJ, Sen C, Bederson JB, Govindaraj S (2000) Applications of fast-setting hydroxyapatite cement: cranioplasty. Otolaryngol Head Neck Surg 123:409–412. https://doi.org/10.1067/mhn.2000.107679
Ducic Y (2002) Titanium mesh and hydroxyapatite cement cranioplasty: a report of 20 cases. J Oral Maxillofac Surg 60:272–276
Edwards MSB, Ousterhout DK (1987) Autogeneic skull bone grafts to reconstruct large or complex skull defects in children and adolescents. Neurosurgery 20:273–280
Eppley BL, Hollier L, Stal S (2003) Hydroxyapatite cranioplasty: II. Clinical experience with a new quick-setting material. J Craniofac Surg 14:209–214
Feroze AH, Walmsley GG, Choudhri O, Lorenz HP, Grant GA, Edwards MS (2015) Evolution of cranioplasty techniques in neurosurgery: historical review, pediatric considerations, and current trends. J Neurosurg 123:1098–1107. https://doi.org/10.3171/2014.11.JNS14622
Fiaschi P, Pavanello M, Imperato A, Dallolio V, Accogli A, Capra V, Consales A, Cama A, Piatelli G (2016) Surgical results of cranioplasty with a polymethylmethacrylate customized cranial implant in pediatric patients: a single-center experience. J Neurosurg Pediatr 17:705–710. https://doi.org/10.3171/2015.10.PEDS15489
Frassanito P, Massimi L, Caldarelli M, Tamburrini G, Di Rocco C (2012) Complications of delayed cranial repair after decompressive craniectomy in children less than 1 year old. Acta Neurochir 154:927–933. https://doi.org/10.1007/s00701-011-1253-5
Frassanito P, Massimi L, Caldarelli M, Tamburrini G, Di Rocco C (2014) Bone flap resorption in infants. J Neurosurg Pediatr 13:243–244. https://doi.org/10.3171/2013.6.PEDS13312
Frassanito P, Massimi L, Tamburrini G, Bianchi F, Nataloni A, Canella V, Caldarelli M (2018) Custom-made hydroxyapatite for cranial repair in a specific pediatric age group (7-13 years old): a multicenter post-marketing surveillance study. Childs Nerv Syst 34:2283–2289. https://doi.org/10.1007/s00381-018-3905-8
Frassanito P, Tamburrini G, Massimi L, Di Rocco C, Nataloni A, Fabbri G, Caldarelli M (2015) Post-marketing surveillance of CustomBone Service implanted in children under 7 years old. Acta Neurochir 157:115–121. https://doi.org/10.1007/s00701-014-2254-y
Frassanito P, Tamburrini G, Massimi L, Peraio S, Caldarelli M, Di Rocco C (2017) Problems of reconstructive cranioplasty after traumatic brain injury in children. Childs Nerv Syst 33:1759–1768. https://doi.org/10.1007/s00381-017-3541-8
Fu KJ, Barr RM, Kerr ML, Shah MN, Fletcher SA, Sandberg DI, Teichgraeber JF, Greives MR (2016) An outcome comparison between autologous and alloplastic cranioplasty in the pediatric population. J Craniofac Surg 27:593–597. https://doi.org/10.1097/SCS.0000000000002491
Gilardino MS, Cabiling DS, Bartlett SP (2009) Long-term follow-up experience with carbonated calcium phosphate cement (Norian) for cranioplasty in children and adults. Plast Reconstr Surg 123:983–994. https://doi.org/10.1097/PRS.0b013e318199f6ad
Gilardino MS, Karunanayake M, Al-Humsi T, Izadpanah A, Al-Ajmi H, Marcoux J, Atkinson J, Farmer JP (2015) A comparison and cost analysis of cranioplasty techniques: autologous bone versus custom computer-generated implants. J Craniofac Surg 26:113–117. https://doi.org/10.1097/SCS.0000000000001305
Goldstein JA, Paliga JT, Bartlett SP (2013) Cranioplasty: indications and advances. Curr Opin Otolaryngol Head Neck Surg 21:400–409. https://doi.org/10.1097/MOO.0b013e328363003e
Goodrich JT, Sandler AL, Tepper O (2012) A review of reconstructive materials for use in craniofacial surgery bone fixation materials, bone substitutes and distractors. Childs Nerv Syst 28:1577–1588. https://doi.org/10.1007/s00381-012-1776-y
Grant GA, Jolley M, Ellenbogen RG, Roberts TS, Gruss JR, Loeser JD (2004) Failure of autologous bone-assisted cranioplasty following decompressive craniectomy in children and adolescents. J Neurosurg 100:163–168. https://doi.org/10.3171/ped.2004.100.2.0163
Greene AK, Mulliken JB, Proctor MR, Rogers GF (2008) Pediatric cranioplasty using particulate calvarial bone graft. Plast Reconstr Surg 122:563–571. https://doi.org/10.1097/PRS.0b013e31817d61c1
Josan VA, Sgouros S, Walsh AR, Dover MS, Nishikawa H, Hockley AD (2005) Cranioplasty in children. Childs Nerv Syst 21:200–204. https://doi.org/10.1007/s00381-004-1068-2
Lam S, Kuether J, Fong A, Reid R (2015) Cranioplasty for large-sized calvarial defects in the pediatric population: a review. Craniomaxillofac Trauma Reconstr 8:159–170. https://doi.org/10.1055/s-0034-1395880
Laurie SW, Kaban LB, Mulliken JB (1984) Donor-site morbidity after harvesting rib and iliac bone. Plast Reconstr Surg 73:933–938
Lin AY, Kinsella CR Jr, Rottgers SA, Smith DM, Grunwaldt LJ, Cooper GM, Losee JE (2012) Custom porous polyethylene implants for large-scale pediatric skull reconstruction: early outcomes. J Craniofac Surg 23:67–70. https://doi.org/10.1097/SCS.0b013e318240c876
Ma IT, Symon MR, Bristol RE, Beals SP, Joganic EF, Adelson PD, Shafron DH, Singh DJ (2018) Outcomes of titanium mesh cranioplasty in pediatric patients. J Craniofac Surg 29:99–104. https://doi.org/10.1097/SCS.0000000000004045
Martin KD, Franz B, Kirsch M, Polanski W, Von der Hagen M, Schackert G, Sobottka SB (2014) Autologous bone flap cranioplasty following decompressive craniectomy is combined with a high complication rate in pediatric traumatic brain injury patients. Acta Neurochir 156:813–824. https://doi.org/10.1007/s00701-014-2021-0
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151:264–269
Moreira-Gonzalez A, Jackson IT, Miyawaki T, Barakat K, DiNick V (2003) Clinical outcome in cranioplasty: critital review in long-term follow-up. J Craniofac Surg 14:144–153
Morice A, Kolb F, Picard A, Kadlub N, Puget S (2017) Reconstruction of a large calvarial traumatic defect using a custom-made porous hydroxyapatite implant covered by a free latissimus dorsi muscle flap in an 11-year-old patient. J Neurosurg Pediatr 19:51–55. https://doi.org/10.3171/2016.8.PEDS1653
Ozerdem OR, Sen O, Anlatici R, Erdoğan B, Aydin V (2002) Osteogaleal flaps in pediatric cranioplasty. Ann Plast Surg 49:127–132
Pang D, Tse HH, Zwienenberg-Lee M, Smith M, Zovickian J (2005) The combined use of hydroxyapatite and bioresorbable plates to repair cranial defects in children. J Neurosurg 102:36–43. https://doi.org/10.3171/ped.2005.102.1.0036
Piedra MP, Thompson EM, Selden NR, Ragel BT, Guillaume DJ (2012) Optimal timing of autologous cranioplasty after decompressive craniectomy in children. J Neurosurg Pediatr 10:268–272. https://doi.org/10.3171/2012.6.PEDS1268
Piittulainen JM, Posti JP, Aitasalo KM, Vuorinen V, Vallittu PK, Serlo W (2015) Paediatric cranial defect reconstruction using bioactive fibre-reinforced composite implant: early outcomes. Acta Neurochir 157:681–687. https://doi.org/10.1007/s00701-015-2363-2
Plum AW, Tatum SA (2015) A comparison between autograft alone, bone cement, and demineralized bone matrix in cranioplasty. Laryngoscope 125:1322–1327. https://doi.org/10.1002/lary.25158
Posnick JC, Goldstein JA, Armstrong D, Rutka JT (1993) Reconstruction of skull defects in children and adolescents by the use of fixed cranial bone grafts: long-term results. Neurosurgery 32:785-791
Rocque BG, Agee BS, Thompson EM, Piedra M, Baird LC, Selden NR, Greene S, Deibert CP, Hankinson TC, Lew SM, Iskandar BJ, Bragg TM, Frim D, Grant G, Gupta N, Auguste KI, Nikas DC, Vassilyadi M, Muh CR, Wetjen NM, Lam SK (2018) Complications following pediatric cranioplasty after decompressive craniectomy: a multicenter retrospective study. J Neurosurg Pediatr 8:1–8. https://doi.org/10.3171/2018.3.PEDS17234
Rocque BG, Amancherla K, Lew SM, Lam S (2013) Outcomes of cranioplasty following decompressive craniectomy in the pediatric population. J Neurosurg Pediatr 12:120–125. https://doi.org/10.3171/2013.4.PEDS12605
Sanan A, Haines SJ (1997) Repairing holes in the head: a history of cranioplasty. Neurosurgery 40:588–603
Schuss P, Vatter H, Marquardt G, Imöhl L, Ulrich CT, Seifert V, Güresir E (2012) Cranioplasty after decompressive craniectomy: the effect of timing on postoperative complications. J Neurotrauma 29:1090–1095. https://doi.org/10.1089/neu.2011.2176
Taggard DA, Menezes AH (2001) Successful use of rib grafts for cranioplasty in children. Pediatr Neurosurg 34:149–155. https://doi.org/10.1159/000056010
Vignes JR, Jeelani NU, Dautheribes M, San-Galli F, Liguoro D (2007) Cranioplasty for repair of a large bone defect in a growing skull fracture in children. J Craniomaxillofac Surg 35:185–188. https://doi.org/10.1016/j.jcms.2007.04.002
Waqas M, Ujjan B, Hadi YB, Najmuddin F, Laghari AA, Khalid S, Bari ME, Bhatti UF (2017) Cranioplasty after craniectomy in a pediatric population: single-center experience from a developing country. Pediatr Neurosurg 52:77–79. https://doi.org/10.1159/000452808
Williams L, Fan K, Bentley R (2016) Titanium cranioplasty in children and adolescents. J Craniomaxillofac Surg 44:789–794. https://doi.org/10.1016/j.jcms.2016.03.010
Zaccaria L, Tharakan SJ, Altermatt S (2017) Hydroxyapatite ceramic implants for cranioplasty in children: a single-center experience. Childs Nerv Syst 33:343–348. https://doi.org/10.1007/s00381-016-3327-4
Acknowledgements
KJM is supported by the Van Wagenen Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
With the submission of this manuscript, I would like to state that the authors report no conflict of interest concerning the materials and methods used or the findings specified in this paper. Furthermore, the authors declare that this study was performed in accordance with the research ethical guidelines.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Klieverik, V.M., Miller, K.J., Singhal, A. et al. Cranioplasty after craniectomy in pediatric patients—a systematic review. Childs Nerv Syst 35, 1481–1490 (2019). https://doi.org/10.1007/s00381-018-4025-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-4025-1