Abstract
Purpose
The literature on histopathological and molecular changes that might underlie secondary tethered cord syndrome (TCS) after myelomeningocele (MMC) repair surgeries remains sparse. To address this problem, we analyzed specimens, which were obtained during untethering surgeries of patients who had a history of MMC repair surgery after birth.
Methods
Specimens of 12 patients were analyzed in this study. Clinical characteristics were obtained retrospectively including pre-operative neurological and bowel/bladder-function, contractures and spasticity of lower extremities, leg and back pain, syringomyelia, and conus position on spinal MRI. Cellular marker expression profiles were established. Further, immunoreactivities (IR) of IL-1ß/IL-1R1, TNF-α/TNF-R1, and HIF-1α/-2α were analyzed qualitatively and semi-quantitatively by densitometry. Co-labeling with cellular markers was determined by multi-fluorescence-labeling. Cytokines were further analyzed on mRNA level. Immunostaining for cleaved PARP and TUNEL was performed to detect apoptotic cells.
Results
Astrocytosis, appearance of monocytes, activated microglia, and apoptotic cells in TCS specimens were one substantial finding of these studies. Besides neurons, these cells co-stained with IL-1ß and TNF-α and their receptors, which were found on significantly elevated IR-level and partially mRNA-level in TCS specimens. Staining for HIF-1α/-2α confirmed induction of hypoxia-related factors in TCS specimens that were co-labeled with IL-1ß. Further, hints for apoptotic cell death became evident by TUNEL and PARP-positive cells in TCS neuroepithelia.
Conclusions
Our studies identified pro-inflammatory and pro-apoptotic mediators that, besides mechanical damaging and along with hypoxia, might promote TCS development. Besides optimizing surgical techniques, these factors should also be taken into account when searching for further options to improve TCS treatment.






Similar content being viewed by others
Abbreviations
- CD3:
-
Cluster of differentiation 3
- CD11b/Integrin αM:
-
Cluster of differentiation 11b
- CD68:
-
Cluster of differentiation 68
- CKPan:
-
Cytokeratin Pan
- CNPase:
-
2′,3′-Cyclic nucleotide 3′-phosphodiesterase
- cPARP:
-
Cleaved poly-ADP-ribose polymerase
- CSF:
-
Cerebrospinal fluid
- CT:
-
Cycle of threshold
- DAB:
-
Diaminobenzidine
- GAPDH:
-
Glyceraldehyde-3-phosphate dehydrogenase
- GFAP:
-
Glial fibrillary acidic protein
- H&E:
-
Hematoxylin-eosin
- HIF:
-
Hypoxia-inducible factor
- IHC:
-
Immunohistochemistry
- IL-1ß:
-
Interleukin-1 beta
- IL-1R1:
-
Interleukin-1 beta receptor type 1
- IR:
-
Immunoreactivity
- MMC:
-
Myelomeningocele
- NeuN:
-
Neuronal nuclear protein
- NF200kD:
-
Neurofilament 200-kD fragment
- RT:
-
Room temperature
- RT-PCR:
-
Reverse transcription polymerase chain reaction
- SD:
-
Standard deviation
- SDS:
-
Sodium dodecyl sulfate
- TCS:
-
Tethered cord syndrome
- TNF-α:
-
Tumor necrosis factor alpha
- TNF-R1:
-
Tumor necrosis factor receptor type 1
- TUNEL:
-
Terminal deoxynucleotidyl transferase-mediated dUTP-biotin nick end labeling
References
Hertzler DA II, DePowell JJ, Stevenson CB, Mangano FT (2010) Tethered cord syndrome: a review of the literature from embryology to adult presentation. Neurosurg Focus 29:E1. https://doi.org/10.3171/2010.3.FOCUS1079
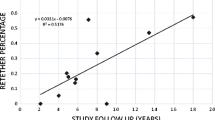
Bowman RM, Mohan A, Ito J, Seibly JM, McLone DG (2009) Tethered cord release: a long-term study in 114 patients. J Neurosurg Pediatr 3:181–187. https://doi.org/10.3171/2008.12.PEDS0874
Bowman RM, McLone DG, Grant JA et al (2001) Spina bifida outcome: a 25-year prospective. Pediatr Neurosurg 34:114–120. https://doi.org/10.1159/000056005
Shurtleff DB, Duguay S, Duguay G, Moskowitz D, Weinberger E, Roberts T, Loeser J (1997) Epidemiology of tethered cord with meningomyelocele. Eur J Pediatr Surg 7(Suppl 1):7–11. https://doi.org/10.1055/s-2008-1071200
Hudgins RJ, Gilreath CL (2004) Tethered spinal cord following repair of myelomeningocele. Neurosurg Focus 16:E7
Lew SM, Kothbauer KF (2007) Tethered cord syndrome: an updated review. Pediatr Neurosurg 43:236–248. https://doi.org/10.1159/000098836
Herman JM, McLone DG, Storrs BB, Dauser RC (1993) Analysis of 153 patients with myelomeningocele or spinal lipoma reoperated upon for a tethered cord. Presentation, management and outcome. Pediatr Neurosurg 19:243–249
Tani S, Yamada S, Knighton RS (1987) Extensibility of the lumbar and sacral cord. Pathophysiology of the tethered spinal cord in cats. J Neurosurg 66:116–123. https://doi.org/10.3171/jns.1987.66.1.0116
Kang JK, Kim MC, Kim DS, Song JU (1987) Effects of tethering on regional spinal cord blood flow and sensory-evoked potentials in growing cats. Childs Nerv Syst 3:35–39
Yamada S, Zinke DE, Sanders D (1981) Pathophysiology of “tethered cord syndrome”. J Neurosurg 54:494–503. https://doi.org/10.3171/jns.1981.54.4.0494
Guthkelch AN, Pang DVJ (1981) Influence of closure technique on results in myelomeningocele. Childs Brain 8:350–355
Samuels R, McGirt MJ, Attenello FJ et al (2009) Incidence of symptomatic retethering after surgical management of pediatric tethered cord syndrome with or without duraplasty. Childs Nerv Syst 25:1085–1089. https://doi.org/10.1007/s00381-009-0895-6
Yamada S, Won DJ, Pezeshkpour G, Yamada BS, Yamada SM, Siddiqi J, Zouros A, Colohan ART (2007) Pathophysiology of tethered cord syndrome and similar complex disorders. Neurosurg Focus 23:1–10. https://doi.org/10.3171/FOC-07/08/E6
Dolan EJ, Transfeldt EE, Tator CH, Simmons EH, Hughes KF (1980) The effect of spinal distraction on regional spinal cord blood flow in cats. J Neurosurg 53:756–764. https://doi.org/10.3171/jns.1980.53.6.0756
Kocak A, Kilic A, Nurlu G et al (1997) A new model for tethered cord syndrome: a biochemical, electrophysiological, and electron microscopic study. Pediatr Neurosurg 26:120–126
Schneider SJ, Rosenthal AD, Greenberg BM, Danto J (1993) A preliminary report on the use of laser-Doppler flowmetry during tethered spinal cord release. Neurosurgery 32:214–218
Yamada S, Knerium DS, Mandybur GM, Schultz RL, Yamada BS (2004) Pathophysiology of tethered cord syndrome and other complex factors. Neurol Res 26:722–726. https://doi.org/10.1179/016164104225018027
Maurya VP, Rajappa M, Wadwekar V, Narayan SK, Barathi D, Madhugiri VS (2016) Tethered cord syndrome—a study of the short term effects of surgical detethering on markers of neuronal injury and electrophysiologic parameters. World Neurosurg. https://doi.org/10.1016/j.wneu.2016.07.005
Kowitzke B, Cohrs G, Leuschner I, Koch A, Synowitz M, Mehdorn HM, Held-Feindt J, Knerlich-Lukoschus F (2016) Cellular profiles and molecular mediators of lesion cascades in the placode in human open spinal neural tube defects. J Neuropathol Exp Neurol 75:827–842. https://doi.org/10.1093/jnen/nlw057
Kwon B, Kim DH, Vaccaro AR (2005) The pathophysiology of tethered cord syndrome: ischemia or apoptosis? Semin Spine Surg 17:8–12. https://doi.org/10.1053/j.semss.2005.01.001
Knerlich-Lukoschus F, Von Der Ropp-Brenner B, Lucius R et al (2010) Chemokine expression in the white matter spinal cord precursor niche after force-defined spinal cord contusion injuries in adult rats. Glia 58:916–931. https://doi.org/10.1002/glia.20974
Knerlich-Lukoschus F, Juraschek M, Blömer U, Lucius R, Mehdorn HM, Held-Feindt J (2008) Force-dependent development of neuropathic central pain and time-related CCL2/CCR2 expression after graded spinal cord contusion injuries of the rat. J Neurotrauma 25:427–448. https://doi.org/10.1089/neu.2007.0431
Qian BJ, You L, Shang FF, Liu J, Dai P, Lin N, He M, Liu R, Zhang Y, Xu Y, Zhang YH, Wang TH (2015) Vimentin regulates neuroplasticity in transected spinal cord rats associated with micRNA138. Mol Neurobiol 51:437–447. https://doi.org/10.1007/s12035-014-8745-2
Pineau I, Sun L, Bastien D, Lacroix S (2010) Astrocytes initiate inflammation in the injured mouse spinal cord by promoting the entry of neutrophils and inflammatory monocytes in an IL-1 receptor/MyD88-dependent fashion. Brain Behav Immun 24:540–553. https://doi.org/10.1016/j.bbi.2009.11.007
Reis JL, Correia-Pinto J, Monteiro MP, Costa M, Hutchins GM (2008) Vascular and apoptotic changes in the placode of myelomeningocele mice during the final stages of in utero development. J Neurosurg Pediatr 2:150–157. https://doi.org/10.3171/PED/2008/2/8/150
Ribotta MGMG, Menet VV, Privat AA (2004) Glial scar and axonal regeneration in the CNS: lessons from GFAP and vimentin transgenic mice. Acta Neurochir Suppl 89:87–92. https://doi.org/10.1007/978-3-7091-0603-7_12
Pekny M, Wilhelmsson U, Pekna M (2014) The dual role of astrocyte activation and reactive gliosis. Neurosci Lett 565:30–38. https://doi.org/10.1016/j.neulet.2013.12.071
Herx LM, Rivest S, Yong VW (2000) Central nervous system-initiated inflammation and neurotrophism in trauma: IL-1 beta is required for the production of ciliary neurotrophic factor. J Immunol 165:2232–2239. https://doi.org/10.4049/jimmunol.165.4.2232
Bastien D, Lacroix S (2014) Cytokine pathways regulating glial and leukocyte function after spinal cord and peripheral nerve injury. Exp Neurol 258:62–77. https://doi.org/10.1016/j.expneurol.2014.04.006
Basu A, Krady JK, Levison SW (2004) Interleukin-1: a master regulator of neuroinflammation. J Neurosci Res 78:151–156. https://doi.org/10.1002/jnr.20266
Giulian D, Woodward J, Young DG, Krebs JF, Lachman LB (1988) Interleukin-1 injected into mammalian brain stimulates astrogliosis and neovascularization. J Neurosci 8:2485–2490
Sato A, Ohtaki H, Tsumuraya T, Song D, Ohara K, Asano M, Iwakura Y, Atsumi T, Shioda S (2012) Interleukin-1 participates in the classical and alternative activation of microglia/macrophages after spinal cord injury. J Neuroinflammation 9:65. https://doi.org/10.1186/1742-2094-9-65
Huang SL, Peng J, Yuan GL, Ding XY, He XJ, Lan BS (2015) A new model of tethered cord syndrome produced by slow traction. Sci Rep 5:9116. https://doi.org/10.1038/srep09116
Imtiyaz HZ, Simon MC (2010) Hypoxia-inducible factors as essential regulators of inflammation. Curr Top Microbiol Immunol 345:105–120. https://doi.org/10.1007/82-2010-74
Basu A, Lazovic J, Krady JK, Mauger DT, Rothstein RP, Smith MB, Levison SW (2005) Interleukin-1 and the interleukin-1 type 1 receptor are essential for the progressive neurodegeneration that ensues subsequent to a mild hypoxic/ischemic injury. J Cereb Blood Flow Metab 25:17–29. https://doi.org/10.1038/sj.jcbfm.9600002
Minami M, Kuraishi Y, Yabuuchi K, Yamazaki A, Satoh M (1992) Induction of interleukin-1 beta mRNA in rat brain after transient forebrain ischemia. J Neurochem 58:390–392
Legos JJ, Whitmore RG, Erhardt JA, Parsons AA, Tuma RF, Barone FC (2000) Quantitative changes in interleukin proteins following focal stroke in the rat. Neurosci Lett 282:189–192. https://doi.org/10.1016/S0304-3940(00)00907-1
Auron PE (1998) The interleukin 1 receptor: ligand interactions and signal transduction. Cytokine Growth Factor Rev 9:221–237. https://doi.org/10.1016/s1359-6101(98)00018-5
Dehne N, Brüne B (2009) HIF-1 in the inflammatory microenvironment. Exp Cell Res 315:1791–1797. https://doi.org/10.1016/j.yexcr.2009.03.019
Chen K-B, Uchida K, Nakajima H, Yayama T, Hirai T, Watanabe S, Guerrero AR, Kobayashi S, Ma WY, Liu SY, Baba H (2011) Tumor necrosis factor-α antagonist reduces apoptosis of neurons and oligodendroglia in rat spinal cord injury. Spine (Phila Pa 1976) 36:1350–1358. https://doi.org/10.1097/BRS.0b013e3181f014ec
Wajant H, Pfizenmaier K, Scheurich P (2003) Tumor necrosis factor signaling. Cell Death Differ 10:45–65. https://doi.org/10.1038/sj.cdd.4401189
Knerlich-Lukoschus F, Noack M, von der Ropp-Brenner B et al (2011) Spinal cord injuries induce changes in CB1 cannabinoid receptor and C-C chemokine expression in brain areas underlying circuitry of chronic pain conditions. J Neurotrauma 28:619–634. https://doi.org/10.1089/neu.2010.1652
Knerlich-Lukoschus F (2015) Chemokines and their receptors: important mediators to be aware of in neuroregenerative approaches for spinal cord injury. Neural Regen Res 10:562–564. https://doi.org/10.4103/1673-5374.155423
Cohrs G, Sürie J-P, Vokuhl C, Held-Feindt J, Synowitz M, Knerlich-Lukoschus F (2018) Establishing a retinoic induced mmc model in rats for investigating molecular lesion cascades during the post-neurulation fetal and perinatal development. Childs Nerv Syst 34:995–1094
Sharma U, Pal K, Pratap A, Gupta DK, Jagannathan NR (2006) Potential of proton magnetic resonance spectroscopy in the evaluation of patients with tethered cord syndrome following surgery. J Neurosurg 105:396–402. https://doi.org/10.3171/ped.2006.105.5.396
Pal K, Sharma U, Gupta DK, Pratap A, Jagannathan NR (2005) Metabolite profile of cerebrospinal fluid in patients with spina bifida: a proton magnetic resonance spectroscopy study. Spine (Phila Pa 1976) 30:E68–E72. https://doi.org/10.1097/01.brs.0000152161.08313.04
Baigrie RJ, Lamont PM, Kwiatkowski D, Dallman MJ, Morris PJ (1992) Systemic cytokine response after major surgery. Br J Surg 79:757–760. https://doi.org/10.1002/bjs.1800790813
Clementsen T, Krohn CD, Reikerås O (2006) Systemic and local cytokine patterns during total hip surgery. Scand J Clin Lab Invest 66:535–542. https://doi.org/10.1080/00365510600889635
Arishima Y, Setoguchi T, Yamaura I, Yone K, Komiya S (2006) Preventive effect of erythropoietin on spinal cord cell apoptosis following acute traumatic injury in rats. Spine (Phila Pa 1976) 31:2432–2438. https://doi.org/10.1097/01.brs.0000239124.41410.7a
Hattermann K, Knerlich-Lukoschus F, Lucius R, Mehdorn M, Held-Feindt J (2015) Erythropoietin and CCL3 antagonise their functional properties during neuroinflammation. Neurol Res 37:1025–1028. https://doi.org/10.1179/1743132815Y.0000000070
Yang L, Yan X, Xu Z, Tan W, Chen Z, Wu B (2016) Delayed administration of recombinant human erythropoietin reduces apoptosis and inflammation and promotes myelin repair and functional recovery following spinal cord compressive injury in rats. Restor Neurol Neurosci 34:647–663. https://doi.org/10.3233/RNN-150498
Acknowledgments
The authors thank Fereshteh Ebrahim, Brigitte Rehmke, and Silvia Iversen for their excellent technical assistance. At this point, we would also like to pay tribute to the memory of Professor Ivo Leuschner who, due to his expertise, cordiality and human warmth, had always been an esteemed discussion and cooperation partner, who passed away too soon in January 2017.
Funding
This work was funded by Familie Mehdorn Stiftung 2015 (to G.C. and F.K.L.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest concerning materials or methods used in this study or the findings specified in this paper exists.
Rights and permissions
About this article
Cite this article
Cohrs, G., Drucks, B., Sürie, JP. et al. Expression profiles of pro-inflammatory and pro-apoptotic mediators in secondary tethered cord syndrome after myelomeningocele repair surgery. Childs Nerv Syst 35, 315–328 (2019). https://doi.org/10.1007/s00381-018-3984-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-3984-6