Abstract
Purpose
Understand the variables that could interfere with diagnosis and prompt treatment in CNS childhood cancer in Brazil, a developing country with continental dimensions.
Methods
From 2005 to 2010, we retrospectively evaluated factors, which could represent a negative influence on the time period elapsing from the onset of symptoms until the diagnosis of the central nervous system (CNS) neoplasia in children and adolescents attended in our service.
Results
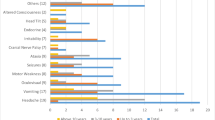
Two hundred seventeen records were analyzed retrospectively. Factors of the households were evaluated, and this data was related to the time period elapsing from presentation of the first symptoms until the diagnosis of CNS neoplasia. The average time elapsed from the onset of the symptoms until seeking medical assistance was 96 days, and from medical assistance to patient referral to a reference service was 33 days. The symptoms which most contributed to a shorter delay in diagnosis were changes in gait and paresis, mother’s occupation, father’s education level, patient gender, and living in the state of São Paulo. Besides that, variables such as male gender, mother’s education level, and lower patient age were associated with an early diagnosis time.
Conclusion
There is great difficulty in performing early diagnosis of CNS tumors, partly due to parent’s inability to recognize signs and symptoms, and in part due to an educational deficit among healthcare professionals. Identification of measures that can minimize these causes of delay is fundamental to increasing the chance of cure and survival of these patients.





Similar content being viewed by others
References
da BM, INCA S (2014) Monitoramento das ações de controle do câncer em crianças e adolescentes. Inf Detecção Precoce 5:1–8
Instituto Nacional de Câncer José Alencar Gomes da Silva C de P e V (2014) Estimate/ 2014- Cancer Incidence in Brazil
Miller TPWCMJLWAWSMD (2016) Childohood leukemia and primary prevention. HHS Public Access 317–52 . doi: https://doi.org/10.1016/j.cppeds.2016.08.004.Childhood
Ribeiro KB, Buffler PA, Metayer C (2008) Socioeconomic status and childhood acute lymphocytic leukemia incidence in São Paulo, Brazil. Int J Cancer 123:1907–1912. https://doi.org/10.1002/ijc.23738
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
Buckner JC, Brown PD, O’Neill BP et al (2007) Central nervous system tumors. Mayo Clin Proc 82:1271–1286. https://doi.org/10.4065/82.10.1271
Levy AS (2005) Brain tumors in children: evaluation. Curr Probl Pediatr Adolesc Heal Care 35:230–245. https://doi.org/10.1016/j.cppeds.2005.04.001
Puccini RF, Hilário MOE (2008) Sinais e sintomas em Oncologia. In: Petrilli AS, Caran EM, Cypriano M (eds) Semiologia da criança e do adolescente. Guanabara Koogan, Rio de Janeiro, pp 280–289
Dang-Tan T, Franco EL (2007) Diagnosis delays in childhood cancer: a review. Cancer 110:703–713
Dobrovoljac M, Hengartner H, Boltshauser E, Grotzer M (2002) Delay in the diagnosis of paediatric brain tumours. Eur J Pediatr 161:663–667. https://doi.org/10.1007/s00431-002-1088-4
IBGE (2010) Censo Demográfico 2010. Características da População e dos Domicílios. Inst Bras Geogr e Estatística 48 . doi: 0104–3145
Sillanpää M, Piekkala P, Kero P (1991) Prevalence of headache at preschool age in an unselected child population. Cephalalgia 11:239–242. https://doi.org/10.1046/j.1468-2982.1991.1105239
Ahrensberg JM, Olesen F, Hansen RP, Schrøder H, Vedsted P (2013) Childhood cancer and factors related to prolonged diagnostic intervals: a Danish population-based study. Br J Cancer 108:1280–1287. https://doi.org/10.1038/bjc.2013.88
Chu TPC, Shah A, Walker D, Coleman MP (2015) Pattern of symptoms and signs of primary intracranial tumours in children and young adults: a record linkage study. Arch Dis Child 100:1115–1122. https://doi.org/10.1136/archdischild-2014-307578
Reulecke BC, Erker CG, Fiedler BJ, Niederstadt TU, Kurlemann G (2008) Brain tumors in children: initial symptoms and their influence on the time span between symptom onset and diagnosis. J Child Neurol 23:178–183. https://doi.org/10.1177/0883073807308692
Wilne SH, Ferris RC, Nathwani A, Kennedy CR (2006) The presenting features of brain tumours: a review of 200 cases. Arch Dis Child 91:502–506. https://doi.org/10.1136/adc.2005.090266
Hayashi N, Kidokoro H, Miyajima Y, Fukazawa T, Natsume J, Kubota T, Kojima S (2010) How do the clinical features of brain tumours in childhood progress before diagnosis? Brain and Development 32:636–641. https://doi.org/10.1016/j.braindev.2009.10.001
Zalewska-Szewczyk B, Zielińska E, Zakrzewski K et al Prognosis of clinical course of primary brain tumours in children in relationship to the duration and characteristic features of initial clinical symptoms. Med Wieku Rozwoj 9:567–578
Kukal K, Dobrovoljac M, Boltshauser E, Ammann RA, Grotzer MA (2009) Does diagnostic delay result in decreased survival in paediatric brain tumours? Eur J Pediatr 168:303–310. https://doi.org/10.1007/s00431-008-0755-5
van Berlaer G, Mortelmans K, Hubloue I (2014) PO-0297 children presenting to the emergency department with headache as primary complaint are not likely to have a brain tumour. Arch Dis Child 99:A341.2–A3A341. https://doi.org/10.1136/archdischild-2014-307384.948
Løhmann DJA, Sørensen P, Jørgensen J, Rosthøj S (2014) Most central nervous system tumours in children are diagnosed with little delay after admission. Dan Med J 61:A4886
NICE Guideline (2015) Suspected Cancer: Recognition and Referral NICE Guidel 25
Walker D, Grundy R, Kennedy C, et al (2013) The Brain Pathways Guideline : A Guideline To Assist Healthcare Professionals in the Assessment of Children Who May Have a Brain Tumour 2017:0–127
Brownstein K, Stevenson E (2007) The essential guide to brain tumors. National B, San Francisco
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Gilli, I.O., Joaquim, A.F., Tedeschi, H. et al. Factors affecting diagnosis of primary pediatric central nervous system neoplasias in a developing country. Childs Nerv Syst 35, 91–96 (2019). https://doi.org/10.1007/s00381-018-3958-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-3958-8