Abstract
Purpose
The purpose of this study was to assess the prevalence of FFT as an additional tethering element in children operated for closed spinal dysraphism, where FFT was not the primary tethering pathology.
Methods
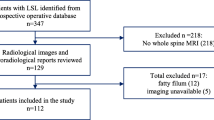
This is a retrospective study of 195 children (< 18 years of age) who underwent surgery for closed spinal dysraphism and did not have FFT as the primary diagnosis. All patients were operated during the period 2005–2017 by a single surgeon. The commonest diagnosis was a lipomyelomeningocele (LMMC, n = 81, 41.5%), followed by split cord malformations (SCM, types I and II, n = 61, 31.3%), dermal sinus (n = 28, 14.4%), and dermoid cyst (n = 10, 5.1%). Factors such as age and sex, presenting symptoms, intraoperative findings, and radiological presence of a FFT on a magnetic resonance imaging (MRI) were documented, and the relationship between the primary diagnoses and presence of FFT was analyzed.
Results
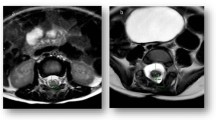
FFT as a secondary finding was seen in 63 patients (32.3%). The mean age of the cohort was 54 months (4.5 years) and the sex distribution was relatively even (51.8% girls). The commonest symptom at presentation was a swelling in the back, followed by lower limb weakness. The mean duration of symptoms was nearly 30 months. FFT was seen on the MRI and confirmed intraoperatively in 55 patients (28.2%). There were 8 patients (4.1%) where a FFT was seen intraoperatively, but was not diagnosed on the preoperative MRI. In 16 patients, FFT was seen > 2 segments away from the primary tethering pathology, 8 of which mandated a second skin incision for sectioning of the FFT. Secondary FFT was most commonly associated with a SCM (types I and II combined) and was seen in 42.6% of those patients. It was least commonly associated with intradural dermoid cysts.
Conclusion
The presence of a secondary FFT should be considered and actively sought on preoperative thin-slice T1W axial MR images in the sacral region in all patients with spinal dysraphism. Even if a FFT is not seen on preoperative MR images, the filum should be explored and sectioned if it is in the vicinity of the primary surgical field, especially in patients with SCM.




Similar content being viewed by others
References
Abel TJ, Chowdhary A, Gabikian P, Ellenbogen RG, Avellino AM (2006) Acquired Chiari malformation type I associated with a fatty terminal filum. J Neurosurg Pediatr 105(4):329–332. https://doi.org/10.3171/ped.2006.105.4.329
Agrawal A, Sampley S (2014) Spinal dysraphism: a challenge continued to be faced by neurosurgeons in developing countries. Asian J Neurosurg 9(2):68–71. https://doi.org/10.4103/1793-5482.136713
Ak H, Atalay T, Gülşen I (2014) The association of the epidermoid cyst of the filum terminale, intradural spinal lipoma, tethered cord, dermal sinus tract, and type I diastematomyelia in a child. World Neurosurg 82(6):e836–e837. https://doi.org/10.1016/j.wneu.2014.08.040
Kumar R, Garg P, Kalra SK, Mahapatra AK (2010) Management of multiple tethering in spinal dysraphism. Childs Nerv Syst 26(12):1743–1747. https://doi.org/10.1007/s00381-010-1148-4
Kumar R, Singh SN (2003) Spinal dysraphism: trends in northern India. Pediatr Neurosurg 38(3):133–145. https://doi.org/10.1159/000068819
Patnaik A, Mahapatra AK (2013) Complex forms of spinal dysraphism. Childs Nerv Syst 29(9):1527–1532. https://doi.org/10.1007/s00381-013-2161-1
Barutcuoglu M, Selcuki M, Selcuki D, Umur S, Mete M, Gurgen SG, Umur (2015) Cutting filum terminale is very important in split cord malformation cases to achieve total release. Childs Nerv Syst 31(3):425–432. https://doi.org/10.1007/s00381-014-2586-1
James CC, Lassman LP (1970) Diastematomyelia and the tight filum terminale. J Neurol Sci 10(2):193–196. https://doi.org/10.1016/0022-510X(70)90019-5
Pang D (1992) Split cord malformation: part II: clinical syndrome. Neurosurgery 31(3):481–500. https://doi.org/10.1227/00006123-199209000-00011
Bao N, Chen Z-H, Gu S, Chen QM, Jin HM, Shi CR (2007) Tight filum terminale syndrome in children: analysis based on positioning of the conus and absence or presence of lumbosacral lipoma. Childs Nerv Syst 23(10):1129–1134. https://doi.org/10.1007/s00381-007-0376-8
Bui CJ, Tubbs RS, Oakes WJ (2007) Tethered cord syndrome in children: a review. Neurosurg Focus 23:E2
De Vloo P, Monea AG, Sciot R, van Loon J, van Calenbergh F (2016) The filum terminale: a cadaver study of anatomy, histology, and elastic properties. World Neurosurg 90:565–573.e1. https://doi.org/10.1016/j.wneu.2015.12.103
Pinto FCG, Fontes RB, Leonhardt Mde C et al (2002) Anatomic study of the filum terminale and its correlations with the tethered cord syndrome. Neurosurgery 51:725–729; discussion 729– 30, 3. https://doi.org/10.1227/00006123-200209000-00019
Filippidis AS, Kalani MY, Theodore N, Rekate HL (2010) Spinal cord traction, vascular compromise, hypoxia, and metabolic derangements in the pathophysiology of tethered cord syndrome. Neurosurg Focus 29(1):E9. https://doi.org/10.3171/2010.3.FOCUS1085
Hertzler DA, DePowell JJ, Stevenson CB, Mangano FT (2010) Tethered cord syndrome: a review of the literature from embryology to adult presentation. Neurosurg Focus 29(1):E1. https://doi.org/10.3171/2010.3.FOCUS1079
Yamada S, Zinke DE, Sanders D (1981) Pathophysiology of “tethered cord syndrome”. J Neurosurg 54(4):494–503. https://doi.org/10.3171/jns.1981.54.4.0494
Selçuki M, Vatansever S, Inan S, Erdemli E, Bağdatoğlu C, Polat A (2003) Is a filum terminale with a normal appearance really normal? Childs Nerv Syst 19(1):3–10. https://doi.org/10.1007/s00381-002-0665-1
Durdağ E, Börcek PB, Öcal Ö, Börcek AÖ, Emmez H, Baykaner MK (2015) Pathological evaluation of the filum terminale tissue after surgical excision. Childs Nerv Syst 31(5):759–763. https://doi.org/10.1007/s00381-015-2627-4
Hansasuta A, Tubbs RS, Oakes WJ (1999) Filum terminale fusion and dural sac termination: study in 27 cadavers. Pediatr Neurosurg 30(4):176–179. https://doi.org/10.1159/000028790
Hendson G, Dunham C, Steinbok P (2016) Histopathology of the filum terminale in children with and without tethered cord syndrome with attention to the elastic tissue within the filum. Childs Nerv Syst 32(9):1683–1692. https://doi.org/10.1007/s00381-016-3123-1
Jang HS, Cho KH, Chang H, Jin ZW, Rodriguez-Vazquez JF, Murakami G (2016) The filum terminale revisited: a histological study in human fetuses. Pediatr Neurosurg 51(1):9–19. https://doi.org/10.1159/000439284
Yundt KD, Park TS, Kaufman BA (1997) Normal diameter of filum terminale in children: in vivo measurement. Pediatr Neurosurg 27(5):257–259. https://doi.org/10.1159/000121263
Pang D, Dias MS, Ahab-Barmada M (1992) Split cord malformation: part I: a unified theory of embryogenesis for double spinal cord malformations. Neurosurgery 31(3):451–480. https://doi.org/10.1227/00006123-199209000-00010
Gaddam SSK, Santhi V, Babu S, Chacko G, Baddukonda RA, Rajshekhar V (2012) Gross and microscopic study of the filum terminale: does the filum contain functional neural elements? J Neurosurg Pediatr 9(1):86–92. https://doi.org/10.3171/2011.10.PEDS11102
Kumar GSS, Rajshekhar V, Babu KS (2006) Intraoperative mapping of sacral nervous system (S2–4). Br J Neurosurg 20(6):396–402. https://doi.org/10.1080/02688690601101481
Legatt AD, Schroeder CE, Gill B, Goodrich JT (1992) Electrical stimulation and multichannel EMG recording for identification of functional neural tissue during cauda equina surgery. Childs Nerv Syst 8(4):185–189. https://doi.org/10.1007/BF00262842
Steinbok P, Kariyattil R, MacNeily AE (2007) Comparison of section of filum terminale and non-neurosurgical management for urinary incontinence in patients with normal conus position and possible occult tethered cord syndrome. Neurosurgery 61(3):550–555; discussion 555–556. https://doi.org/10.1227/01.NEU.0000290902.07943.E6
Drake JM (2006) Occult tethered cord syndrome: not an indication for surgery. J Neurosurg Pediatr 104(5):305–308. https://doi.org/10.3171/ped.2006.104.5.305
Steinbok P, MacNeily AE, Hengel AR, Afshar K, Landgraf JM, Hader W, Pugh J (2016) Filum section for urinary incontinence in children with occult tethered cord syndrome: a randomized, controlled pilot study. J Urol 195(4):1183–1188. https://doi.org/10.1016/j.juro.2015.09.082
Mahapatra AK, Gupta DK (2005) Split cord malformations: a clinical study of 254 patients and a proposal for a new clinical—imaging classification. J Neurosurg Pediatr 103(6):531–536. https://doi.org/10.3171/ped.2005.103.6.0531
Borkar SA, Mahapatra AK (2012) Split cord malformations: a two years experience at AIIMS. Asian J Neurosurg 7(2):56–60. https://doi.org/10.4103/1793-5482.98643
Mahapatra AK (2011) Split cord malformation—a study of 300 cases at AIIMS 1990-2006. J Pediatr Neurosci 6(Suppl 1):S41–S45. https://doi.org/10.4103/1817-1745.85708
Sinha S, Agarwal D, Mahapatra AK (2006) Split cord malformations: an experience of 203 cases. Childs Nerv Syst 22(1):3–7. https://doi.org/10.1007/s00381-005-1145-1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee. For this type of study, formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Gupta, A., Rajshekhar, V. Fatty filum terminale (FFT) as a secondary tethering element in children with closed spinal dysraphism. Childs Nerv Syst 34, 925–932 (2018). https://doi.org/10.1007/s00381-017-3700-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-017-3700-y