Abstract
Introduction
Even though shunt surgery has been an established and widely accepted treatment for congenital hydrocephalus for five decades, long-term follow-up and functional outcome data is rare.
Patients and methods
Sixty-nine patients were examined after congenital hydrocephalus had been treated between 1971 and 1987 at the Department of Pediatric Surgery (University of Leipzig) within the first 12 months of life. Median age of patients was 32 years (range 25–42 years). Patients agreed to undergo a contemporary hydrocephalus assessment.
Results
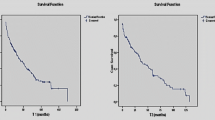
Seven patients (10.1 %) became shunt-independent before adulthood. By the age of 20, 82 % of the patients had needed at least one shunt revision, 100 % by the age of 30. 21.7 % of the primary valves (Spitz-Holter) remained intact without revision until today up to 35 years (mean functional intactness 23 years). Shunt infections occurred in 4.3 % of primary implantations.
48 % of the patients had a good functional outcome (mRS = 0–1). 40.9 % of the patients attended regular school. In summary, 75 % patients work on a daily basis. 44.6 % live an independent life, 35.4 % rely on parental supervision, and 20 % depend on professional care institutions.
Conclusion
Compared to the pre-shunt era, surgery within the first year of life is advantageous regarding visual function, educational progress, and social results. The outcome achieved throughout childhood remains stable during adult life as long as catastrophic events of shunt malfunction can be prevented.
Epilepsy, motor deficits, acute shunt dysfunction, and problems of social integration as well as aging parental caregivers seem to be prominent factors of morbidity in adulthood.





Similar content being viewed by others
References
Eliasson AC, Krumlinde-Sundholm L, Rösblad B, Beckung E, Arner M, Ohrvall AM, Rosenbaum P (2006) The manual ability classification system (MACS) for children with cerebral palsy: scale development and evidence of validity and reliability. Dev Med Child Neurol 48(7):549–554
Farrell B, Godwin J, Richards S, Warlow C (1991) The United Kingdom transient ischaemic attack (UK-TIA) aspirin trial: final results. J Neurol Neurosurg Psychiatry 54:1044–1054
Hirsch JF (1994) Consensus: long-term outcome in hydrocephalus. Childs Nerv Syst 10:64–69
Laurence KM, Coates S (1962) The natural history of hydrocephalus. Detailed analysis of 182 unoperated cases. Arch Dis Child 37:345–362
Lemcke J, Meier U, Müller C, Fritsch MJ, Kehler U, Langer N, Kiefer M, Eymann R, Schuhmann MU, Speil A, Weber F, Remenez V, Rohde V, Ludwig HC, Stengel D (2013) Safety and efficacy of gravitational shunt valves in patients with idiopathic normal pressure hydrocephalus: a pragmatic, randomised, open label, multicentre trial (SVASONA). J Neurol Neurosurg Psychiatry 84(8):850–857
Palisano R, Rosenbaum P, Walter S, Russel D, Wood E, Galuppi B (1997) Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 39(4):214–223
Rankin J (1953) Cerebral vascular accidents in patients over the age of 60. II. Prognosis. Scott Med J 2:200–215
Reddy GK, Bollam P, Caldito G, Guthikonda B, Nanda A (2012) Ventriculoperitoneal shunt surgery outcome in adult transition patients with pediatric-onset hydrocephalus. Neurosurgery 70(2):380–388
Simon TD, Lamb S, Murphy NA, Hom B, Walker ML, Clark EB (2009) Who will care for me next? Transitioning to adulthood with hydrocephalus. Pediatrics 124(5):1431–1437
Stein SC, Langfitt TW (1974) Normal-pressure hydrocephalus. Predicting the results of cerebrospinal fluid shunting. J Neurosurg 41:463–470
Stone JJ, Walker CT, Jacobson M, Phillips V, Silberstein HJ (2013) Revision rate of pediatric ventriculoperitoneal shunts after 15 years. J Neurosurg Pediatr 11(1):15–19
Vinchon M, Baroncini M, Delestret I (2012) Adult outcome of pediatric hydrocephalus. Childs Nerv Syst 28(6):847–854
Acknowledgments
We acknowledge the huge and highly esteemed contribution of the pediatric surgical staff and surgeons, who diagnosed, treated, and operated the many children under very different technical circumstances at their time at University Leipzig, compared to today. Many of them are only known to us by their thorough and detailed history taking and archiving of the medical records, in this way enabling us to analyze the long-term results.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Preuss, M., Kutscher, A., Wachowiak, R. et al. Adult long-term outcome of patients after congenital hydrocephalus shunt therapy. Childs Nerv Syst 31, 49–56 (2015). https://doi.org/10.1007/s00381-014-2571-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-014-2571-8