Abstract
N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels prior to transcatheter aortic valve implantation (TAVI) are known to be associated with outcomes of patients undergoing TAVI. However, little has been known about the NT-proBNP response after TAVI. Therefore, we aimed to clarify the role of the NT-proBNP response and identify the determinants of the NT-proBNP nonresponse among patients with severe aortic stenosis (AS) and heart failure (HF) undergoing TAVI. We examined 717 patients with severe AS and HF undergoing TAVI. NT-proBNP nonresponders were defined as patients whose NT-proBNP levels decreased by ≤ 30%. Mean NT-proBNP levels decreased from 7698 ± 7853 pg/mL (baseline) to 4523 ± 5173 pg/mL (post-TAVI); 269 patients (38%) were nonresponders. Female gender and prevalence of diabetes mellitus (DM), chronic kidney disease (CKD), atrial fibrillation (AF), and history of coronary artery revascularization were more common for NT-proBNP nonresponders. Permanent pacemaker implantation rate was higher for NT-proBNP nonresponders. In addition to the baseline NT-proBNP level > 7500 pg/smL (hazard ratio [HR], 1.8; p = 0.03), NT-proBNP nonresponse (HR 2.3; p = 0.001) was associated with lower survival rates. Baseline NT-proBNP level ≤ 7500 pg/mL (OR 3.2; p < 0.001), female gender (odds ratio [OR], 1.5; p = 0.049), DM (OR 1.6; p = 0.016), CKD (OR 1.8; p = 0.001), AF (OR 2.4; p < 0.001), history of coronary revascularization (OR 1.7; p = 0.003), and permanent pacemaker implantation after TAVI (OR 1.7; p = 0.034) were independent determinants of NT-proBNP nonresponse. In “conclusion”, NT-proBNP response is important for long-term survival after TAVI. We should consider the aforementioned determinants, particularly permanent pacemaker implantation, as risk factors for NT-proBNP nonresponse.
Similar content being viewed by others
Introduction
Transcatheter aortic valve implantation (TAVI) is a novel and reliable therapeutic option for high-risk or inoperable patients with severe symptomatic aortic stenosis (AS) [1,2,3,4]. Heart failure (HF) is complicated for most candidates for TAVI [2,5,6]. Natriuretic peptide (NP) is a cardiac hormone mainly produced by cardiac myocytes in response to pressure and volume overload, and serum NP levels are useful for the diagnosis and management of patients with HF [7,8,9,10]. Previous studies reported that elevated NP levels at baseline were associated with outcomes of patients with AS undergoing not only surgical aortic valve replacement [11,12] but also TAVI [13,14,15]. In association with the improvement in acute phase outcomes of TAVI (because of the evolution of device and technique), chronic phase outcomes after TAVI have attracted clinical interests. Because TAVI leads to the resolution of pressure overload of the left ventricle, NP levels can decrease after the procedure, and the NP response after TAVI may affect the long-term prognosis of patients undergoing TAVI. However, little is known about the response of NP levels after TAVI; therefore, determinants of the NP response after the procedure remain unclear. We sought to clarify the role of the NP response after TAVI and to identify the determinants of the NP nonresponse among patients with severe AS and HF undergoing TAVI.
Patients and methods
Study population
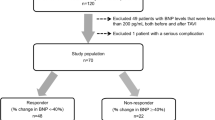
We examined 1497 patients who underwent transfemoral TAVI at the Heart Center Brandenburg between July 2008 and May 2017. AS was diagnosed based on the mean transvalvular pressure gradient and aortic valve area calculated using the continuity equation. Left ventricular ejection fraction (LVEF) was measured using Simpson’s method. We excluded 43 patients who died during hospitalization, 187 patients whose serum NT-proBNP levels were not available, 541 patients due to low baseline NT-proBNP levels according to rule-in cutoff values for heart failure [16] (450 pg/mL for those younger than 50 years, 900 pg/mL for those aged 50–75 years, and 1800 pg/mL for those older than 75 years), and 9 patients requiring hemodialysis. We examined the remaining 717 patients in this study (Fig. 1).
Flowchart of study patients [16]
Ethics
We performed this study as a part of a retrospective analysis from a single-center TAVI registry according to the ethical guidelines of our institution. All patients were informed about specific risks and alternative treatments and all of them provided informed consent regarding the use of general data for the scientific activity in future. This study was performed in accordance with the Declaration of Helsinki.
Definition
The primary endpoint was all-cause death. The estimated glomerular filtration rate (eGFR) was calculated using the Modification of Diet in Renal Disease equation: eGFR (mL/min/1.73 m2) = 186 × (serum creatinine)−1.1544 × (age)−0.203 × (0.742, if female) [17,18]. Chronic kidney disease (CKD) was defined as eGFR < 60 mL/min/1.73 m2. We determined the cutoff value of NT-proBNP at baseline as 7500 pg/mL based on its average value. We defined responders to NT-proBNP as patients whose NT-proBNP levels had decreased from baseline by > 30% at the time of hospital discharge [19,20,21].
Transfemoral TAVI
Indications for TAVI were decided by a discussion among members of our multidisciplinary heart team, including experienced cardiologists, cardiovascular surgeons, and anesthesiologists. If iliofemoral access was anatomically and technically possible, then patients underwent transfemoral TAVI. We performed transfemoral TAVI as previously described [22].
Statistical analysis
Categorical and consecutive data regarding patient backgrounds are presented as percentage and mean values ± standard deviation, respectively. The Chi-square test was used for comparisons between NT-proBNP responders and nonresponders, and the unpaired t test was used for comparison of consecutive variables. The paired t test was used for comparison between serum NT-proBNP levels at baseline and at hospital discharge. Long-term survival after hospital discharge was estimated using Kaplan–Meier curves and the log-rank test to assess the significance of differences between NT-pro BNP responders and nonresponders. We performed the multivariable Cox regression analysis to identify prognostic determinants after hospital discharge using factors potentially associated with patient survival, including NT-proBNP nonresponse, NT-proBNP > 7500 pg/mL at baseline, female gender, age ≥ 80 years, LVEF ≤ 40%, history of coronary artery revascularization, history of heart surgery, diabetes mellitus (DM), history of myocardial infarction, hypertension, dyslipidemia, atrial fibrillation (AF), chronic obstructive pulmonary disease, peripheral artery disease, history of stroke, and CKD. To identify the determinants of NT-proBNP nonresponse, we performed a multivariable logistic regression analysis using the following covariates selected from factors that were significantly different between NT-proBNP responders and nonresponders: NT-pro BNP ≤ 7500 pg/mL female gender, DM, CKD, AF, history of coronary revascularization, LVEF ≤ 40%, and permanent pacemaker implantation after TAVI. A p value of < 0.05 indicated a statistically significant difference. We conducted statistical analyzes using SPSS version 19.0 software (SPSS Inc, Chicago, IL, USA).
Results
NT-pro BNP response after TAVI
The paired t test demonstrated that the mean NT-proBNP levels significantly decreased from 7698 ± 7853 pg/mL at baseline to 4523 ± 5173 pg/mL at hospital discharge (p < 0.001) (Fig. 2). Among a total of 717 patients, 448 patients (62%) were NT-proBNP responders and 269 patients (38%) were NT-proBNP nonresponders. NT-proBNP decreased from 8853 ± 8335 pg/mL at baseline to 3106 ± 3149 pg/mL at discharge in NT-proBNP responders, whereas NT-proBNP increased from 5773 ± 6552 pg/mL at baseline to 6884 ± 6783 pg/mL at discharge in NT-proBNP nonresponders.
Characteristics and echocardiographic findings
Table 1 shows the characteristics and echocardiographic findings of study patients. NT-proBNP nonresponders were more likely to be female, and age was not significantly different between NT-proBNP responders and nonresponders. Serum NT-proBNP levels at baseline were higher for NT-proBNP responders. DM, CKD, and AF were more common for NT-proBNP nonresponders than for responders. History of coronary artery revascularization was more common for NT-proBNP nonresponders. Left ventricular (LV) diastolic dimension (Dd) was smaller and LVEF was higher for NT-proBNP nonresponders. The prevalence of moderate or higher grades of tricuspid regurgitation (TR) and tricuspid annular plane systolic excursion were not different between the two groups.
TAVI procedure and outcome
On average, peak and mean aortic valve pressure gradients decreased from 71 ± 28 and 47 ± 19 mmHg at baseline to 20 ± 9 and 12 ± 8 mmHg after the procedure, respectively (both p < 0.001). The following devices were implanted in 717 patients: Sapien (Edwards Lifesciences, Irvine, CA) in 9 patients; Sapien XT (Edwards Lifesciences, Irvine, CA) in 96 patients; Sapien 3 (Edwards Lifesciences, Irvine, CA) in 383 patients; CoreValve (Medtronic, Inc., Minneapolis, MN) in 109 patients; CoreValve Evolut R (Medtronic, Inc., Minneapolis, MN) in 55 patients; Lotus (Boston Scientific, Marlborough, MA) in 10 patients; Boston Acurate neo (Boston Scientific, Marlborough, MA) in 8 patients; Portico (Abbott, Menlo Park, CA) in 20 patients, Direct Flow (Direct Flow Medical, Santa Rosa, CA) in 26 patients; and NVT Allegla (New Valve Technology, Hechingen, Germany) in 1 patient. Prevalence of moderate or higher grades of aortic regurgitation after TAVI was not different between NT-proBNP responders and nonresponders (3.5% vs. 3.3%; p = 0.864). Permanent pacemaker implantation rate was higher for NT-proBNP nonresponders than for responders (18% vs. 12%; p = 0.030).
Survival after TAVI
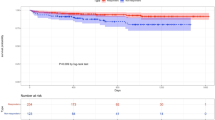
Kaplan–Meier curves showed that NT-proBNP nonresponders had lower survival rates after hospital discharge (log-rank p < 0.001) (Fig. 3). Multivariable Cox regression analysis revealed that NT-proBNP > 7500 pg/mL (hazard ratio [HR], 1.8; p = 0.020; 95% confidence interval (CI) 1.1–3.1) and NT-proBNP nonresponse (HR 2.3; p = 0.001; 95% CI 1.4–3.9) were independently associated with higher mortality after hospital discharge (Table 2).
Predictors of NT-pro BNP nonresponse
Multivariable logistic regression analysis revealed that baseline NT-pro BNP≤ 7500 pg/mL (OR 3.2; p < 0.001), female gender (odds ratio [OR], 1.5; p = 0.049), DM (OR 1.6; p = 0.016), CKD (OR 1.8; p = 0.001), AF (OR 2.4; p < 0.001), history of coronary artery revascularization (OR 1.7; p = 0.003), and permanent pacemaker implantation after TAVI (OR 1.7; p = 0.034) were independent determinants of NT-proBNP nonresponse after TAVI (Table 3). LVEF ≤ 40% was not statically significant (p = 0.363).
Discussion
The key findings of the present study were as follows: mean NT-proBNP levels decreased from 7698 ± 7853 pg/mL (baseline) at baseline to 4523 ± 5173 pg/mL at discharge; 38% of study patients were nonresponders; baseline NT-proBNP level > 7500 pg/mL and NT-proBNP nonresponse were independently associated with lower survival rates after hospital discharge; and female gender, baseline NT-proBNP level > 7500 pg/mL, DM, CKD, AF, history of coronary artery revascularization, and permanent pacemaker implantation after TAVI were independent determinants of NT-proBNP nonresponse.
In accordance with previous studies [13,14,15], higher NT-proBNP levels at baseline were associated with worse survival rates of patients treated with TAVI. Interestingly, higher NT-proBNP levels negatively affected the outcomes of patients undergoing TAVI, even after hospital discharge. NP is mainly released by cardiac monocytes of the left ventricle in response to pressure and volume overload [9]. Therefore, it was shown that NT-proBNP levels were associated with AS severity and symptoms [23,24]. From this point of view, it is reasonable that NT-proBNP levels immediately decreased at hospital discharge after a rapid release of pressure overload by TAVI. Overall, NT-proBNP levels significantly decreased at hospital discharge. Nevertheless, nearly 40% of study patients were categorized as nonresponders. Moreover, NT-proBNP nonresponders independently had worse survival rates after hospital discharge. This result is partially in line with the results of the study by Mizutani et al., which showed an association between BNP elevation at discharge and higher mortality after TAVI [25].
It should be noted that the NT-proBNP response was associated with outcomes of patients undergoing TAVI independent of baseline NT-proBNP levels. Accordingly, it is important to consider determinants of NT-proBNP nonresponse, including gender, DM, CKD, AF, history of coronary artery revascularization, and permanent pacemaker implantation. However, for most of these, intervention is not possible; therefore, permanent pacemaker implantation may have an essential role as a modifiable factor. Subsequent conduction disturbance requiring permanent pacemaker implantation is the most frequent adverse event [26] and could limit the clinical benefits of TAVI. This complication was associated with prolonged hospital stay and increased procedural costs [27]. Nazif et al. reported that permanent pacemaker implantation was associated with a longer duration of hospitalization and higher rates of repeat hospitalization and mortality or repeat hospitalization [28]. Those findings are in agreement with the results of the present study. Therefore, we need to focus attention on this complication to improve long-term outcomes of patients undergoing TAVI from the perspective of HF recovery.
Study limitations
There were several limitations to this study. Because of the limited sample size, the statistical power may not be strong enough for any negative data to be conclusive. Furthermore, we did not have data regarding rehospitalization due to HF after TAVI. Paradoxically, NT-proBNP responses were more commonly observed in those with higher baseline NT-proBNP levels, suggesting that some degree of HF would remain even after TAVI. Therefore, the proportion of nonresponders defined by the degree of decline of NT-proBNP would be relatively higher for those with lower baseline NT-proBNP levels. The time interval between the TAVI procedure and timing of NT-pro BNP measurement before discharge is not assessed in this study. Periprocedural factors including volume overload and myocardial injury can influence the NT-proBNP response. Further study is required to clarify the association between these factors.
Conclusion
NT-proBNP nonresponse is independently associated with lower long-term survival rates after TAVI. Female gender, DM, CKD, AF, history of coronary artery revascularization, and permanent pacemaker implantation after TAVI were determinants of the NT-proBNP nonresponse. Therefore, we should consider these determinants, particularly permanent pacemaker implantation, as a modifiable target as risk factors for NT-proBNP nonresponse.
References
Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Brown DL, Block PC, Guyton RA, Pichard AD, Bavaria JE, Herrmann HC, Douglas PS, Petersen JL, Akin JJ, Anderson WN, Wang D, Pocock S (2010) Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 363:1597–1607
Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Williams M, Dewey T, Kapadia S, Babaliaros V, Thourani VH, Corso P, Pichard AD, Bavaria JE, Herrmann HC, Akin JJ, Anderson WN, Wang D, Pocock SJ (2011) Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 364:2187–2198
Biancari F, D'Errigo P, Rosato S, Pol M, Tamburino C, Ranucci M, Seccareccia F (2017) Transcatheter aortic valve replacement in nonagenarians: early and intermediate outcome from the OBSERVANT study and meta-analysis of the literature. Heart Vessels 32:157–165
Higuchi R, Tobaru T, Hagiya K, Saji M, Mahara K, Takamisawa I, Shimizu J, Takanashi S, Takayama M (2017) Transcatheter aortic valve implantation in patients on corticosteroid therapy. Heart Vessels 32:1236–1243
Leon MB, Smith CR, Mack MJ, Makkar RR, Svensson LG, Kodali SK, Thourani VH, Tuzcu EM, Miller DC, Herrmann HC, Doshi D, Cohen DJ, Pichard AD, Kapadia S, Dewey T, Babaliaros V, Szeto WY, Williams MR, Kereiakes D, Zajarias A, Greason KL, Whisenant BK, Hodson RW, Moses JW, Trento A, Brown DL, Fearon WF, Pibarot P, Hahn RT, Jaber WA, Anderson WN, Alu MC, Webb JG; PARTNER 2 Investigators (2016) Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med 374(17):1609–1620
Walther T, Hamm CW, Schuler G, Berkowitsch A, Kotting J, Mangner N, Mudra H, Beckmann A, Cremer J, Welz A, Lange R, Kuck KH, Mohr FW, Mollmann H (2015) Perioperative results and complications in 15,964 transcatheter aortic valve replacements: prospective data from the GARY registry. J Am Coll Cardiol 65:2173–2180
Seino Y, Ogawa A, Yamashita T, Fukushima M, Ogata K, Fukumoto H, Takano T (2004) Application of NT-proBNP and BNP measurements in cardiac care: a more discerning marker for the detection and evaluation of heart failure. Eur J Heart Fail 6:295–300
Groenning BA, Raymond I, Hildebrandt PR, Nilsson JC, Baumann M, Pedersen F (2004) Diagnostic and prognostic evaluation of left ventricular systolic heart failure by plasma N-terminal pro-brain natriuretic peptide concentrations in a large sample of the general population. Heart 90:297–303
Daniels LB, Maisel AS (2007) Natriuretic peptides. J Am Coll Cardiol 50:2357–2368
Felker GM, Hasselblad V, Hernandez AF, O'Connor CM (2009) Biomarker-guided therapy in chronic heart failure: a meta-analysis of randomized controlled trials. Am Heart J 158:422–430
Bergler-Klein J, Klaar U, Heger M, Rosenhek R, Mundigler G, Gabriel H, Binder T, Pacher R, Maurer G, Baumgartner H (2004) Natriuretic peptides predict symptom-free survival and postoperative outcome in severe aortic stenosis. Circulation 109:2302–2308
Pedrazzini GB, Masson S, Latini R, Klersy C, Rossi MG, Pasotti E, Faletra FF, Siclari F, Minervini F, Moccetti T, Auricchio A (2008) Comparison of brain natriuretic peptide plasma levels versus logistic EuroSCORE in predicting in-hospital and late postoperative mortality in patients undergoing aortic valve replacement for symptomatic aortic stenosis. Am J Cardiol 102:749–754
Kefer J, Beauloye C, Astarci P, Renkin J, Glineur D, Dekleermaeker A, Vanoverschelde JL (2010) Usefulness of B-type natriuretic peptide to predict outcome of patients treated by transcatheter aortic valve implantation. Am J Cardiol 106:1782–1786
Koskinas KC, O'Sullivan CJ, Heg D, Praz F, Stortecky S, Pilgrim T, Buellesfeld L, Juni P, Windecker S, Wenaweser P (2015) Effect of B-type natriuretic peptides on long-term outcomes after transcatheter aortic valve implantation. Am J Cardiol 116:1560–1565
Abramowitz Y, Chakravarty T, Jilaihawi H, Lee C, Cox J, Sharma RP, Mangat G, Cheng W, Makkar RR (2015) Impact of PREPROCEdural B-type natriuretic peptide levels on the outcomes after transcatheter aortic valve implantation. Am J Cardiol 116:1904–1909
Januzzi JL, van Kimmenade R, Lainchbury J, Bayes-Genis A, Ordonez-Llanos J, Santalo-Bel M, Pinto YM, Richards M (2006) NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: The International Collaborative of NT-proBNP Study. Eur Heart J 27:330–337
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130:461–470
Kaneko H, Neuss M, Schau T, Weissenborn J, Butter C (2017) Interaction between renal function and percutaneous edge-to-edge mitral valve repair using MitraClip. J Cardiol 69:476–482
Karlstrom P, Alehagen U, Boman K, Dahlstrom U (2011) Brain natriuretic peptide-guided treatment does not improve morbidity and mortality in extensively treated patients with chronic heart failure: responders to treatment have a significantly better outcome. Eur J Heart Fail 13:1096–1103
Ribeiro A, Lourenco P, Silva S, Cunha F, Vilaca J, Gomes F, Araujo JP, Bettencourt P (2015) Predictors of natriuretic peptide non-response in patients hospitalized with acute heart failure. Am J Cardiol 115:69–74
Kaneko H, Neuss M, Weissenborn J, Butter C (2017) Role of right ventricular dysfunction and diabetes mellitus in N-terminal pro-B-type natriuretic peptide response of patients with severe mitral regurgitation and heart failure after MitraClip. Int Heart J 58:225–231
Kaneko H, Hoelschermann F, Schau T, Tambor G, Neuss M, Butter C (2017) Different impact of aortic regurgitation assessed by aortic root angiography after transcatheter aortic valve implantation according to baseline left ventricular ejection fraction and N-terminal pro-B-type natriuretic peptide. Cardiovasc Interv Ther. https://doi.org/10.1007/s12928-017-0473-x
Weber M, Arnold R, Rau M, Brandt R, Berkovitsch A, Mitrovic V, Hamm C (2004) Relation of N-terminal pro-B-type natriuretic peptide to severity of valvular aortic stenosis. Am J Cardiol 94:740–745
Gerber IL, Stewart RA, Legget ME, West TM, French RL, Sutton TM, Yandle TG, French JK, Richards AM, White HD (2003) Increased plasma natriuretic peptide levels reflect symptom onset in aortic stenosis. Circulation 107:1884–1890
Mizutani K, Hara M, Iwata S, Murakami T, Shibata T, Yoshiyama M, Naganuma T, Yamanaka F, Tada N, Takagi K, Araki M, Ueno H, Tabata M, Shirai S, Watanabe Y, Yamamoto M, Hayashida K (2017) Elevation of B-type natriuretic peptide at discharge is associated with 2-year mortality after transcatheter aortic valve replacement in patients with severe aortic stenosis: insights from a multicenter prospective OCEAN-TAVI (optimized transcatheter valvular intervention-transcatheter aortic valve implantation) registry. J Am Heart Assoc 6:e006112
Khatri PJ, Webb JG, Rodes-Cabau J, Fremes SE, Ruel M, Lau K, Guo H, Wijeysundera HC, Ko DT (2013) Adverse effects associated with transcatheter aortic valve implantation: a meta-analysis of contemporary studies. Ann Intern Med 158:35–46
Chevreul K, Brunn M, Cadier B, Haour G, Eltchaninoff H, Prat A, Leguerrier A, Blanchard D, Fournial G, Iung B, Donzeau-Gouge P, Tribouilloy C, Debrux JL, Pavie A, Gilard M, Gueret P (2013) Cost of transcatheter aortic valve implantation and factors associated with higher hospital stay cost in patients of the FRANCE (FRench Aortic National CoreValve and Edwards) registry. Arch Cardiovasc Dis 106:209–219
Nazif TM, Dizon JM, Hahn RT, Xu K, Babaliaros V, Douglas PS, El-Chami MF, Herrmann HC, Mack M, Makkar RR, Miller DC, Pichard A, Tuzcu EM, Szeto WY, Webb JG, Moses JW, Smith CR, Williams MR, Leon MB, Kodali SK (2015) Predictors and clinical outcomes of permanent pacemaker implantation after transcatheter aortic valve replacement: the PARTNER (Placement of AoRtic TraNscathetER Valves) trial and registry. JACC Cardiovasc Interv 8:60–69
Acknowledgements
We thank all staff of the intervention laboratory in our institute.
Funding
This work was supported by the Japan Society for the Promotion of Science (Hidehiro Kaneko).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflict of interest for this study.
Rights and permissions
About this article
Cite this article
Kaneko, H., Hoelschermann, F., Tambor, G. et al. Impact of N-terminal pro-B-type natriuretic peptide response on long-term prognosis after transcatheter aortic valve implantation for severe aortic stenosis and heart failure. Heart Vessels 34, 777–783 (2019). https://doi.org/10.1007/s00380-018-1297-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-018-1297-z