Abstract
Purpose
To identify clinical and stone-related factors predicting the need for surgical intervention in patients who were clinically considered appropriate for non-surgical intervention.
Patients and methods
We conducted a retrospective review of a contemporary cohort of patients who were selected for surveillance following presentation with acute ureteric colic. Data on patient demographic and stone variables, inpatient management and long-term outcomes were evaluated. Multivariate logistic regression was used to generate a nomogram predicting need for surgical intervention. The accuracy of the nomogram was subsequently validated with an independent cohort of patients presenting with ureteric colic.
Results
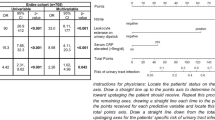
Of 870 study eligible patients presenting with acute ureteric colic, 527 were initially treated non-surgically and included in the analysis. 113 of these eventually required surgical intervention. Median time from first presentation to acute surgery was 11 (IQR 4–82) days. In our final MVA analysis, duration of symptoms more than 3 days, not receiving alpha-blockers, positive history of previous renal calculi and stone location, burden and density were independent predictors of need for surgical intervention. Patients who required opioid analgesia were more likely to have surgical intervention; however, this did not reach statistical significance. The area under the curve (AUC) of the final model was 0.802. The nomogram was validated with a cohort of 210 consecutive colic patients with AUC of 0.833 (SE 0.041, p < 0.001).
Conclusions
We have identified independent predictors of the need for surgical intervention during an episode of renal colic and formulated a nomogram. Combined with the diligent use of acute ureteroscopy at our centre, this nomogram may have clinical utility when making decisions regarding treatment options with potential healthcare cost savings.

Similar content being viewed by others
References
Curhan GC (2007) Epidemiology of stone disease. Urol Clin N Am 34(3):287–293. https://doi.org/10.1016/j.ucl.2007.04.003
Scales CD Jr, Smith AC, Hanley JM, Saigal CS, Urologic Diseases in America P (2012) Prevalence of kidney stones in the United States. Eur Urol 62(1):160–165. https://doi.org/10.1016/j.eururo.2012.03.052
Romero V, Akpinar H, Assimos DG (2010) Kidney stones: a global picture of prevalence, incidence, and associated risk factors. Rev Urol 12(2–3):e86–e96
Du J, Johnston R, Rice M (2009) Temporal trends of acute nephrolithiasis in Auckland, New Zealand. NZ Med J 122(1299):13–20
Acland G, Zargar-Shoshtari K, Rice M (2016) Contemporary trends in urinary tract stone surgery, a regional perspective: Auckland, New Zealand. ANZ J Surg 86(4):244–248. https://doi.org/10.1111/ans.13205
Lotan Y (2009) Economics and cost of care of stone disease. Adv Chronic Kidney Dis 16(1):5–10. https://doi.org/10.1053/j.ackd.2008.10.002
Saigal CS, Joyce G, Timilsina AR, Urologic Diseases in America P (2005) Direct and indirect costs of nephrolithiasis in an employed population: opportunity for disease management? Kidney Int 68(4):1808–1814. https://doi.org/10.1111/j.1523-1755.2005.00599.x
Coll DM, Varanelli MJ, Smith RC (2002) Relationship of spontaneous passage of ureteral calculi to stone size and location as revealed by unenhanced helical CT. AJR Am J Roentgenol 178(1):101–103. https://doi.org/10.2214/ajr.178.1.1780101
Parekattil SJ, White MD, Moran ME, Kogan BA (2004) A computer model to predict the outcome and duration of ureteral or renal calculous passage. J Urol 171(4):1436–1439. https://doi.org/10.1097/01.ju.0000116327.29170.0b
Sfoungaristos S, Kavouras A, Perimenis P (2012) Predictors for spontaneous stone passage in patients with renal colic secondary to ureteral calculi. Int Urol Nephrol 44(1):71–79. https://doi.org/10.1007/s11255-011-9971-4
Zargar-Shoshtari K, Anderson W, Rice M (2015) Role of emergency ureteroscopy in the management of ureteric stones: analysis of 394 cases. BJU Int 115(6):946–950. https://doi.org/10.1111/bju.12841
Castro EP, Osther PJ, Jinga V, Razvi H, Stravodimos KG, Parikh K, Kural AR, de la Rosette JJ, Group CUGS (2014) Differences in ureteroscopic stone treatment and outcomes for distal, mid-, proximal, or multiple ureteral locations: the Clinical Research Office of the Endourological Society ureteroscopy global study. Eur Urol 66(1):102–109. https://doi.org/10.1016/j.eururo.2014.01.011
Ozcan C, Aydogdu O, Senocak C, Damar E, Eraslan A, Oztuna D, Bozkurt OF (2015) Predictive factors for spontaneous stone passage and the potential role of serum C-reactive protein in patients with 4–10 mm distal ureteral stones: a prospective clinical study. J Urol 194(4):1009–1013. https://doi.org/10.1016/j.juro.2015.04.104
Aldaqadossi HA (2013) Stone expulsion rate of small distal ureteric calculi could be predicted with plasma C-reactive protein. Urolithiasis 41(3):235–239. https://doi.org/10.1007/s00240-013-0551-1
Park CH, Ha JY, Park CH, Kim CI, Kim KS, Kim BH (2013) Relationship between spontaneous passage rates of ureteral stones less than 8 mm and serum C-reactive protein levels and neutrophil percentages. Korean J Urol 54(9):615–618. https://doi.org/10.4111/kju.2013.54.9.615
Papa L, Stiell IG, Wells GA, Ball I, Battram E, Mahoney JE (2005) Predicting intervention in renal colic patients after emergency department evaluation. CJEM 7(2):78–86
Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck C, Gallucci M, Knoll T, Lingeman JE, Nakada SY, Pearle MS, Sarica K, Turk C, Wolf JS Jr., Panel EANG (2007) 2017 guideline for the management of ureteral calculi. J Urol 178(6):2418–2434. https://doi.org/10.1016/j.juro.2007.09.107
Hubner WA, Irby P, Stoller ML (1993) Natural history and current concepts for the treatment of small ureteral calculi. Eur Urol 24(2):172–176
Ordon M, Andonian S, Blew B, Schuler T, Chew B, Pace KT (2015) CUA guideline: management of ureteral calculi. Cann Urol Assoc J 9(11–12):E837–E851. https://doi.org/10.5489/cuaj.3483
Macneil F, Bariol S (2011) Urinary stone disease—assessment and management. Aust Fam Phys 40(10):772–775
Dal Moro F, Abate A, Lanckriet GR, Arandjelovic G, Gasparella P, Bassi P, Mancini M, Pagano F (2006) A novel approach for accurate prediction of spontaneous passage of ureteral stones: support vector machines. Kidney Int 69(1):157–160. https://doi.org/10.1038/sj.ki.5000010
Sfoungaristos S, Kavouras A, Kanatas P, Duvdevani M, Perimenis P (2014) Early hospital admission and treatment onset may positively affect spontaneous passage of ureteral stones in patients with renal colic. Urology 84(1):16–21. https://doi.org/10.1016/j.urology.2014.01.005
Hollingsworth JM, Rogers MA, Kaufman SR, Bradford TJ, Saint S, Wei JT, Hollenbeck BK (2006) Medical therapy to facilitate urinary stone passage: a meta-analysis. Lancet 368(9542):1171–1179. https://doi.org/10.1016/S0140-6736(06)69474-9
Ye Z, Zeng G, Yang H, Tang K, Zhang X, Li H, Li W, Wu Z, Chen L, Chen X (2017) Efficacy and safety of tamsulosin in medical expulsive therapy for distal ureteral stones with renal colic: a multicenter, randomized, double-blind, placebo-controlled trial. Eur Urol 73:385
Pickard R, Starr K, MacLennan G, Lam T, Thomas R, Burr J, McPherson G, McDonald A, Anson K, N’Dow J, Burgess N, Clark T, Kilonzo M, Gillies K, Shearer K, Boachie C, Cameron S, Norrie J, McClinton S (2015) Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. Lancet 386(9991):341–349. https://doi.org/10.1016/S0140-6736(15)60933-3
Zargar-Shoshtari K, Sharma P, Zargar H (2015) Re: medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled Trial. Eur Urol 68(5):910–911. https://doi.org/10.1016/j.eururo.2015.07.069
Funding
This study was partly funded from Counties Manukau Health Summer Studentship to Miss Lauren C Holmes.
Author information
Authors and Affiliations
Contributions
Mohit Bajaj: Manuscript writing, Lance Yuan: Data collection, Lauren C. Holmes: Data collection, Michael Rice: Protocol/project development, Kamran Zargar-Shoshtari: Protocol/project development, Analysis, Manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
No other sources of funding or conflicts of interest to disclose.
Informed consent
This is a retrospective study and a formal consent is not required. Institutional ethical approval was obtained for this retrospective study.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Bajaj, M., Yuan, L., Holmes, L.C. et al. Predictors of surgical intervention following initial surveillance for acute ureteric colic. World J Urol 36, 1477–1483 (2018). https://doi.org/10.1007/s00345-018-2279-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-018-2279-6