Abstract
Objectives
To develop and compare several machine learning models to predict occult cervical lymph node (LN) metastasis in early-stage oral tongue squamous cell cancer (OTSCC) from preoperative MRI texture features.
Materials and methods
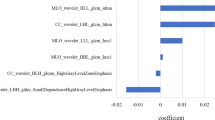
We retrospectively enrolled 116 patients with early-stage OTSCC (cT1-2N0) who had been surgically treated by tumor excision and elective neck dissection (END). For each patient, we extracted 86 texture features from T2-weighted imaging (T2WI) and contrast-enhanced T1-weighted imaging (ceT1WI), respectively. Dimension reduction was performed in three consecutive steps: reproducibility analysis, collinearity analysis, and information gain algorithm. Models were created using six machine learning methods, including logistic regression (LR), random forest (RF), naïve Bayes (NB), support vector machine (SVM), AdaBoost, and neural network (NN). Their performance was assessed using tenfold cross-validation.
Results
Occult LN metastasis was pathologically detected in 42.2% (49/116) of the patients. No significant association was identified between node status and patients’ gender, age, or clinical T stage. Dimension reduction steps selected 6 texture features. The NB model gave the best overall performance, which correctly classified the nodal status in 74.1% (86/116) of the carcinomas, with an AUC of 0.802.
Conclusion
Machine learning–based MRI texture analysis offers a feasible tool for preoperative prediction of occult cervical node metastasis in early-stage OTSCC.
Key Points
• A machine learning–based MRI texture analysis approach was adopted to predict occult cervical node metastasis in early-stage OTSCC with no evidence of node involvement on conventional images.
• Six texture features from T2WI and ceT1WI of preoperative MRI were selected to construct the predictive model.
• After comparing six machine learning methods, naïve Bayes (NB) achieved the best performance by correctly identifying the node status in 74.1% of the patients, using tenfold cross-validation.





Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- ceT1WI:
-
Contrast-enhanced T1-weighted imaging
- DOI:
-
Depth of invasion
- END:
-
Elective neck dissection
- GLCM:
-
Gray-level co-occurrence matrix
- GLDM:
-
Gray-level dependence matrix
- GLRLM:
-
Gray-level run-length matrix
- GLSZM:
-
Gray-level size zone matrix
- HNSCC:
-
Head and neck squamous cell carcinoma
- ICCs:
-
Intraclass correlation coefficients
- LN:
-
Lymph node
- LR:
-
Logistic regression
- MRI:
-
Magnetic resonance imaging
- NB:
-
Naïve Bayes
- NN:
-
Neural network
- OTSCC:
-
Oral tongue squamous cell carcinoma
- RF:
-
Random forest
- ROC:
-
Receiver operator characteristic
- ROI:
-
Region of interests
- SVM:
-
Support vector machine
- T2WI:
-
T2-Weighted imaging
- TE:
-
Echo time
- TR:
-
Repetition time
- VOI:
-
Volume of interest
References
Chen W, Zheng R, Baade PD et al (2016) Cancer statistics in China, 2015. CA Cancer J Clin 66:115–132
Greenberg JS, El Naggar AK, Mo V, Roberts D, Myers JN (2003) Disparity in pathologic and clinical lymph node staging in oral tongue carcinoma. Implication for therapeutic decision making. Cancer 98:508–515
Oh LJ, Phan K, Kim SW et al (2020) Elective neck dissection versus observation for early-stage oral squamous cell carcinoma: systematic review and meta-analysis. Oral Oncol 105:104661
Kelner N, Rodrigues PC, Bufalino A et al (2015) Activin A immunoexpression as predictor of occult lymph node metastasis and overall survival in oral tongue squamous cell carcinoma. Head Neck 37:479–486
Yuen AP, Ho CM, Chow TL et al (2009) Prospective randomized study of selective neck dissection versus observation for N0 neck of early tongue carcinoma. Head Neck 31:765–772
Kelly HR, Curtin HD (2017) Chapter 2 Squamous cell carcinoma of the head and neck-imaging evaluation of regional lymph nodes and implications for management. Semin Ultrasound CT MR 38:466–478
Goel V, Parihar PS, Parihar A et al (2016) Accuracy of MRI in prediction of tumour thickness and nodal stage in oral tongue and gingivobuccal cancer with clinical correlation and staging. J Clin Diagn Res 10:Tc01–Tc05
Liang L, Luo X, Lian Z et al (2017) Lymph node metastasis in head and neck squamous carcinoma: efficacy of intravoxel incoherent motion magnetic resonance imaging for the differential diagnosis. Eur J Radiol 90:159–165
Noij DP, Pouwels PJW, Ljumanovic R et al (2015) Predictive value of diffusion-weighted imaging without and with including contrast-enhanced magnetic resonance imaging in image analysis of head and neck squamous cell carcinoma. Eur J Radiol 84:108–116
Connolly M, Srinivasan A (2018) Diffusion-weighted imaging in head and neck cancer: technique, limitations, and applications. Magn Reson Imaging Clin N Am 26:121–133
Yamada I, Yoshino N, Hikishima K et al (2018) Oral carcinoma: clinical evaluation using diffusion kurtosis imaging and its correlation with histopathologic findings. Magn Reson Imaging 51:69–78
Romeo V, Cuocolo R, Ricciardi C et al (2020) Prediction of tumor grade and nodal status in oropharyngeal and oral cavity squamous-cell carcinoma using a radiomic approach. Anticancer Res 40:271–280
Park JH, Bae YJ, Choi BS et al (2019) Texture analysis of multi-shot echo-planar diffusion-weighted imaging in head and neck squamous cell carcinoma: the diagnostic value for nodal metastasis. J Clin Med 8:1767
Huang YQ, Liang CH, He L et al (2016) Development and validation of a radiomics nomogram for preoperative prediction of lymph node metastasis in colorectal cancer. J Clin Oncol 34:2157–2164
Wu S, Zheng J, Li Y et al (2018) Development and validation of an MRI-based radiomics signature for the preoperative prediction of lymph node metastasis in bladder cancer. EBioMedicine 34:76–84
Forghani R, Chatterjee A, Reinhold C et al (2019) Head and neck squamous cell carcinoma: prediction of cervical lymph node metastasis by dual-energy CT texture analysis with machine learning. Eur Radiol 29:6172–6181
Kocak B, Durmaz ES, Ates E, Kaya OK, Kilickesmez O (2019) Unenhanced CT texture analysis of clear cell renal cell carcinomas: a machine learning-based study for predicting histopathologic nuclear grade. AJR Am J Roentgenol W1–W8. https://doi.org/10.2214/AJR.18.20742
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86:420–428
Daghistani TA, Elshawi R, Sakr S et al (2019) Predictors of in-hospital length of stay among cardiac patients: a machine learning approach. Int J Cardiol 288:140–147
Lambin P, Leijenaar RTH, Deist TM et al (2017) Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol 14:749–762
Bayanati H, Thornhill RE, Souza CA et al (2015) Quantitative CT texture and shape analysis: can it differentiate benign and malignant mediastinal lymph nodes in patients with primary lung cancer? Eur Radiol 25:480–487
Andersen MB, Harders SW, Ganeshan B et al (2016) CT texture analysis can help differentiate between malignant and benign lymph nodes in the mediastinum in patients suspected for lung cancer. Acta Radiol 57:669–676
Liu S, Shi H, Ji C et al (2018) Preoperative CT texture analysis of gastric cancer: correlations with postoperative TNM staging. Clin Radiol 73:756.e751–756.e759
Kuno H, Garg N (2019) CT texture analysis of cervical lymph nodes on contrast-enhanced [(18)F] FDG-PET/CT images to differentiate nodal metastases from reactive lymphadenopathy in HIV-positive patients with head and neck squamous cell carcinoma. AJNR Am J Neuroradiol 40:543–550
Kan Y, Dong D, Zhang Y et al (2019) Radiomic signature as a predictive factor for lymph node metastasis in early-stage cervical cancer. J Magn Reson Imaging 49:304–310
Wang T, Gao T, Yang J et al (2019) Preoperative prediction of pelvic lymph nodes metastasis in early-stage cervical cancer using radiomics nomogram developed based on T2-weighted MRI and diffusion-weighted imaging. Eur J Radiol 114:128–135
Yu YY, Zhang R, Dong RT et al (2019) Feasibility of an ADC-based radiomics model for predicting pelvic lymph node metastases in patients with stage IB-IIA cervical squamous cell carcinoma. Br J Radiol 92:20180986
Cui X, Wang N, Zhao Y et al (2019) Preoperative prediction of axillary lymph node metastasis in breast cancer using radiomics features of DCE-MRI. Sci Rep 9:2240
Han L, Zhu Y, Liu Z et al (2019) Radiomic nomogram for prediction of axillary lymph node metastasis in breast cancer. Eur Radiol 29:3820–3829
Liu C, Ding J, Spuhler K et al (2019) Preoperative prediction of sentinel lymph node metastasis in breast cancer by radiomic signatures from dynamic contrast-enhanced MRI. J Magn Reson Imaging 49:131–140
Friedman NGD, Goldszmidt M (1997) Bayesian network classifiers. Mach Learn 29:131–163
Rodolico V, Barresi E, Di Lorenzo R et al (2004) Lymph node metastasis in lower lip squamous cell carcinoma in relation to tumour size, histologic variables and p27Kip1 protein expression. Oral Oncol 40:92–98
Okura M, Iida S, Aikawa T et al (2008) Tumor thickness and paralingual distance of coronal MR imaging predicts cervical node metastases in oral tongue carcinoma. AJNR Am J Neuroradiol 29:45–50
Kwon M, Moon H, Nam SY et al (2016) Clinical significance of three-dimensional measurement of tumour thickness on magnetic resonance imaging in patients with oral tongue squamous cell carcinoma. Eur Radiol 26:858–865
Lam P, Au-Yeung KM, Cheng PW et al (2004) Correlating MRI and histologic tumor thickness in the assessment of oral tongue cancer. AJR Am J Roentgenol 182:803–808
Funding
This study has received funding by National Scientific Foundation of China (Grant number: 91859202, 81771901, to Xiaofeng Tao). Youth Medical Talents-Medical Imaging Practitioner Program (to Ying Yuan), Shanghai Municipal Health Commission (Grant number: 20194Y0104 to Jiliang Ren).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Xiaofeng Tao.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• case-control study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yuan, Y., Ren, J. & Tao, X. Machine learning–based MRI texture analysis to predict occult lymph node metastasis in early-stage oral tongue squamous cell carcinoma. Eur Radiol 31, 6429–6437 (2021). https://doi.org/10.1007/s00330-021-07731-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-07731-1