Abstract
Objectives
To assess the value of the MR-based radiomics signature in differentiating ocular adnexal lymphoma (OAL) and idiopathic orbital inflammation (IOI).
Methods
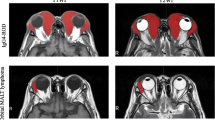
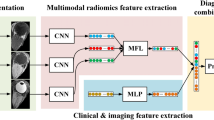
One hundred fifty-seven patients with pathology-proven OAL (84 patients) and IOI (73 patients) were divided into primary and validation cohorts. Eight hundred six radiomics features were extracted from morphological MR images. The least absolute shrinkage and selection operator (LASSO) procedure and linear combination were used to select features and build radiomics signature for discriminating OAL from IOI. Discriminating performance was assessed by the area under the receiver-operating characteristic curve (AUC). The predictive results were compared with the assessment of radiologists by chi-square test.
Results
Five radiomics features were included in the radiomics signature, which differentiated OAL from IOI with an AUC of 0.74 and 0.73 in the primary and validation cohorts respectively. There was a significant difference between the classification results of the radiomics signature and those of a radiology resident (p < 0.05), although there was no significant difference between the results of the radiomics signature and those of a more experienced radiologist (p > 0.05).
Conclusions
Radiomics features have the potential to differentiate OAL from IOI.
Key Points
• Clinical and imaging findings of OAL and IOI often overlap, which makes diagnosis difficult.
• Radiomics features can potentially differentiate OAL from IOI non invasively.
• The radiomics signature discriminates OAL from IOI at the same level as an experienced radiologist.




Similar content being viewed by others
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- AUC:
-
Area under the ROC curve
- DCE:
-
Dynamic contrast enhanced
- DWI:
-
Diffusion-weighted imaging
- ETL:
-
Echo train length
- FS:
-
Fat saturation
- FSE:
-
Fast spin echo
- GLCM:
-
Grey level co-occurrence matrix
- GLRLM:
-
Grey level run length matrix
- ICC:
-
Intraclass correlation coefficient
- IOI:
-
Idiopathic orbital inflammation
- LASSO:
-
Least absolute shrinkage and selection operators procedure
- MRI:
-
Magnetic resonance imaging
- NEX:
-
Number of excitations
- OAL:
-
Ocular adnexal lymphoma
- ROC:
-
Receiver-operating characteristic
- SRHGE:
-
Short-run high-grey emphasis
- T1WI:
-
T1-weighted images
- T2WI:
-
T2-weighted image
- TE:
-
Echo time
- TR:
-
Repetition time
References
Rosado MF, Byrne GE, Ding F et al (2006) Ocular adnexal lymphoma: a clinicopathologic study of a large cohort of patients with no evidence for an association with Chlamydia psittaci. Blood 107:467–472
Sjö LD (2009) Ophthalmic lymphoma: epidemiology and pathogenesis. Acta Ophthalmologica 87:1–20
Shields JA, Shields CL, Scartozzi R (2004) Survey of 1264 patients with orbital tumors and simulating lesions: The 2002 Montgomery Lecture, part 1. Ophthalmology 111:997–1008
Ferreri AJ, Dolcetti R, Du MQ et al (2008) Ocular adnexal MALT lymphoma: an intriguing model for antigen-driven lymphomagenesis and microbial-targeted therapy. Ann Oncol 19:835–846
Woolf DK, Ahmed M, Plowman PN (2012) Primary lymphoma of the ocular adnexa (orbital lymphoma) and primary intraocular lymphoma. Clin Oncol (R Coll Radiol) 24:339–344
Kharod SM, Herman MP, Morris CG, Lightsey J, Mendenhall WM, Mendenhall NP (2018) Radiotherapy in the management of orbital lymphoma: a single institution's experience over 4 decades. Am J Clin Oncol 41:100–106
Shikishima K, Kawai K, Kitahara K (2006) Pathological evaluation of orbital tumours in Japan: analysis of a large case series and 1379 cases reported in the Japanese literature. Clin Exp Ophthalmol 34:239–244
Rubin PA, Foster CS (2004) Etiology and management of idiopathic orbital inflammation. Am J Ophthalmol 138:1041–1043
Swamy BN, McCluskey P, Nemet A et al (2007) Idiopathic orbital inflammatory syndrome: clinical features and treatment outcomes. Br J Ophthalmol 91:1667–1670
Dagi Glass LR, Freitag SK (2016) Orbital inflammation: Corticosteroids first. Survey of Ophthalmology 61:670–673
Mombaerts I, Rose GE, Garrity JA (2016) Orbital Inflammation: Biopsy first. Survey of Ophthalmology 61:664-669
Cytryn AS, Putterman AM, Schneck GL, Beckman E, Valvassori GE (1997) Predictability of magnetic resonance imaging in differentiation of orbital lymphoma from orbital inflammatory syndrome. Ophthal Plast Reconstr Surg 13:129–134
Haradome K, Haradome H, Usui Y et al (2014) Orbital lymphoproliferative disorders (OLPDs): value of MR imaging for differentiating orbital lymphoma from benign OPLDs. AJNR Am J Neuroradiol 35:1976–1982
Xian J, Zhang Z, Wang Z et al (2010) Value of MR imaging in the differentiation of benign and malignant orbital tumors in adults. Eur Radiol 20:1692–1702
Warner MA, Weber AL, Jakobiec FA (1996) Benign and malignant tumors of the orbital cavity including the lacrimal gland. Neuroimaging Clin N Am 6:123–142
Roshdy N, Shahin M, Kishk H et al (2010) MRI in diagnosis of orbital masses. Curr Eye Res 35:986–991
Sullivan TJ, Valenzuela AA (2006) Imaging features of ocular adnexal lymphoproliferative disease. Eye 20:1189–1195
Uehara F, Ohba N (2002) Diagnostic imaging in patients with orbital cellulitis and inflammatory pseudotumor. Int Ophthalmol Clin 42:133–142
Politi LS, Forghani R, Godi C et al (2010) Ocular adnexal lymphoma: diffusion-weighted MR imaging for differential diagnosis and therapeutic monitoring. Radiology 256:565–574
Fatima Z, Ichikawa T, Ishigame K et al (2014) Orbital masses: the usefulness of diffusion-weighted imaging in lesion categorization. Clin Neuroradiol 24:129–134
Kapur R, Sepahdari AR, Mafee MF et al (2009) MR imaging of orbital inflammatory syndrome, orbital cellulitis, and orbital lymphoid lesions: the role of diffusion-weighted imaging. AJNR Am J Neuroradiol 30:64–70
Sepahdari AR, Aakalu VK, Setabutr P, Shiehmorteza M, Naheedy JH, Mafee MF (2010) Indeterminate orbital masses: restricted diffusion at MR imaging with echo-planar diffusion-weighted imaging predicts malignancy. Radiology 256:554–564
Purohit BS, Vargas MI, Ailianou A et al (2016) Orbital tumours and tumour-like lesions: exploring the armamentarium of multiparametric imaging. Insights Imaging 7:43–68
Sun B, Song L, Wang X et al (2017) Lymphoma and inflammation in the orbit: Diagnostic performance with diffusion-weighted imaging and dynamic contrast-enhanced MRI. J Magn Reson Imaging 45:1438–1445
Xu XQ, Hu H, Liu H et al (2017) Benign and malignant orbital lymphoproliferative disorders: differentiating using multiparametric MRI at 3.0T. J Magn Reson Imaging 45:167–176
Lambin P, Riosvelazquez E, Leijenaar RTH et al (2012) Radiomics: Extracting more information from medical images using advanced feature analysis. Eur J Cancer 48:441–446
Kumar V, Gu Y, Basu S et al (2012) Radiomics: the process and the challenges. Magn Reson Imaging 30:1234–1248
Huang Y, Liu Z, He L et al (2016) Radiomics signature: a potential biomarker for the prediction of disease-free survival in early-stage (I or II) non-small cell lung cancer. Radiology 281:947–957
Huang YQ, Liang CH, He L et al (2016) Development and validation of a radiomics nomogram for preoperative prediction of lymph node metastasis in colorectal cancer. J Clin Oncol 34:2157–2164
Parmar C, Leijenaar RT, Grossmann P et al (2015) Radiomic feature clusters and prognostic signatures specific for lung and head & neck cancer. Sci Rep 5:11044
Wang J, Kato F, Oyama-Manabe N et al (2015) Identifying triple-negative breast cancer using background parenchymal enhancement heterogeneity on dynamic contrast-enhanced MRI: A pilot radiomics study. PLOS ONE 10. https://doi.org/10.1371/journal.pone.0143308
Nie K, Shi L, Chen Q et al (2016) Rectal cancer: assessment of neoadjuvant chemoradiation outcome based on radiomics of multiparametric MRI. Clin Cancer Res 22:5256–5264
Aerts HJ, Velazquez ER, Leijenaar RT et al (2014) Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nat Commun 5:4006
Bayanati H, Thornhill RE, Souza CA et al (2014) Quantitative CT texture and shape analysis: Can it differentiate benign and malignant mediastinal lymph nodes in patients with primary lung cancer? Eur Radiol 25:480–487
Nie K, Chen JH, Yu HJ, Chu Y, Nalcioglu O, Su MY (2008) Quantitative analysis of lesion morphology and texture features for diagnostic prediction in breast MRI. Acad Radiol 15:1513–1525
Juntu J, Sijbers J, De Backer S, Rajan J, Van Dyck D (2010) Machine learning study of several classifiers trained with texture analysis features to differentiate benign from malignant soft-tissue tumors in T1-MRI images. J Magn Reson Imaging 31:680–689
Thornhill RE, Golfam M, Sheikh A et al (2014) Differentiation of lipoma from liposarcoma on MRI using texture and shape analysis. Acad Radiol 21:1185–1194
Fruehwald-Pallamar J, Hesselink JR, Mafee MF, Holzer-Fruehwald L, Czerny C, Mayerhoefer ME (2016) Texture-based analysis of 100 MR examinations of head and neck tumors - Is it possible to discriminate between benign and malignant masses in a multicenter trial? Rofo 188:195–202
Ding ZX, Lip G, Chong V (2011) Idiopathic orbital pseudotumour. Clin Radiol 66:886–892
Li Z, Mao Y, Li H, Yu G, Wan H, Li B (2015) Differentiating brain metastases from different pathological types of lung cancers using texture analysis of T1 postcontrast MR. Magne Reson Med 76:1410–1419
Zhang B, Tian J, Dong D et al (2017) Radiomics features of multiparametric MRI as novel prognostic factors in advanced nasopharyngeal carcinoma. Clin Cancer Res 23:4259–4269
Ganeshan B, Abaleke S, Young RC, Chatwin CR, Miles KA (2010) Texture analysis of non-small cell lung cancer on unenhanced computed tomography: initial evidence for a relationship with tumour glucose metabolism and stage. Cancer Imaging 10:137–143
Ganeshan B, Miles KA, Young RC, Chatwin CR (2007) In search of biologic correlates for liver texture on portal-phase CT. Acad Radiol 14:1058–1068
Ganeshan B, Skogen K, Pressney I, Coutroubis D, Miles K (2012) Tumour heterogeneity in oesophageal cancer assessed by CT texture analysis: preliminary evidence of an association with tumour metabolism, stage, and survival. Clin Radiol 67:157–164
Ganeshan B, Panayiotou E, Burnand K, Dizdarevic S, Miles K (2012) Tumour heterogeneity in non-small cell lung carcinoma assessed by CT texture analysis: a potential marker of survival. Eur Radiol 22:796–802
Skogen K, Ganeshan B, Good C, Critchley G, Miles K (2013) Measurements of heterogeneity in gliomas on computed tomography relationship to tumour grade. J Neurooncol 111:213–219
Frighetto-Pereira L, Rangayyan RM, Metzner GA (2016) Shape, texture and statistical features for classification of benign and malignant vertebral compression fractures in magnetic resonance images. Computers in Biology & Medicine 73:147–156
Woods BJ, Clymer BD, Kurc T et al (2007) Malignant-lesion segmentation using 4D co-occurrence texture analysis applied to dynamic contrast-enhanced magnetic resonance breast image data. J Magn Reson Imaging 25:495–501
Sasaguri K, Takahashi N, Takeuchi M, Carter RE, Leibovich BC, Kawashima A (2016) Differentiation of benign from metastatic adrenal masses in patients with renal cell carcinoma on contrast-enhanced CT. AJR Am J Roentgenol 207:1031–1038
Fruehwald-Pallamar J, Czerny C, Holzer-Fruehwald L et al (2013) Texture-based and diffusion-weighted discrimination of parotid gland lesions on MR images at 3.0 Tesla. NMR Biomed 26:1372–1379
Mueller-Using S, Feldt T, Sarfo FS, Eberhardt KA (2016) Factors associated with performing tuberculosis screening of HIV-positive patients in Ghana: LASSO-based predictor selection in a large public health data set. BMC Public Health 16:563
Gibbs P, Turnbull LW (2003) Textural analysis of contrast-enhanced MR images of the breast. Magn Reson Med 50:92–98
Xu R, Kido S, Suga K et al (2014) Texture analysis on (18)F-FDG PET/CT images to differentiate malignant and benign bone and soft-tissue lesions. Ann Nucl Med 28:926–935
Way TW, Hadjiiski LM, Sahiner B et al (2006) Computer-aided diagnosis of pulmonary nodules on CT scans: segmentation and classification using 3D active contours. Medical Physics 33:2323–2337
Sepahdari AR, Politi LS, Aakalu VK, Kim HJ, Razek AA (2014) Diffusion-weighted imaging of orbital masses: multi-institutional data support a 2-ADC threshold model to categorize lesions as benign, malignant, or indeterminate. AJNR Am J Neuroradiol 35:170–175
Acknowledgements
The authors would like to express their sincere appreciation to all reviewers for their kind comments.
This work was presented in part at the 2017 International Society of Magnetic Resonance Imaging in Medicine Annual Meeting.
Funding
This study has received funding from the High Level Health Technical Personnel of Bureau of Health in Beijing under grant no. 2014-2-005; Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support under grant no. ZYLX201704; Key Talent Project of Beijing under Grant no. 2014001; The Priming Scientific Research Foundation for the Senior Researcher in Beijing Tongren Hospital, Capital Medical University, under grant no. 2016-YJJ-GGL-011.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Junfang Xian.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic study
• performed at one institution
Rights and permissions
About this article
Cite this article
Guo, J., Liu, Z., Shen, C. et al. MR-based radiomics signature in differentiating ocular adnexal lymphoma from idiopathic orbital inflammation. Eur Radiol 28, 3872–3881 (2018). https://doi.org/10.1007/s00330-018-5381-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5381-7