Abstract
Objectives
We compared the interobserver agreement for the recently introduced contrast-enhanced ultrasound (CEUS)-based algorithm CEUS-LI-RADS (Liver Imaging Reporting and Data System) versus the well-established magnetic resonance imaging (MRI)-LI-RADS for non-invasive diagnosis of hepatocellular carcinoma (HCC) in high-risk patients.
Methods
Focal liver lesions in 50 high-risk patients (mean age 66.2 ± 11.8 years; 39 male) were assessed retrospectively with CEUS and MRI. Two independent observers reviewed CEUS and MRI examinations, separately, classifying observations according to CEUS-LI-RADSv.2016 and MRI-LI-RADSv.2014. Interobserver agreement was assessed with Cohen’s kappa.
Results
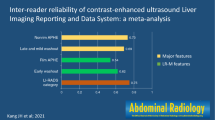
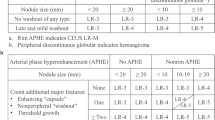
Forty-three lesions were HCCs; two were intrahepatic cholangiocarcinomas; five were benign lesions. Arterial phase hyperenhancement was perceived less frequently with CEUS than with MRI (37/50 / 38/50 lesions = 74%/78% [CEUS; observer 1/observer 2] versus 46/50 / 44/50 lesions = 92%/88% [MRI; observer 1/observer 2]). Washout appearance was observed in 34/50 / 20/50 lesions = 68%/40% with CEUS and 31/50 / 31/50 lesions = 62%/62%) with MRI. Interobserver agreement was moderate for arterial hyperenhancement (ĸ = 0.511/0.565 [CEUS/MRI]) and “washout” (ĸ = 0.490/0.582 [CEUS/MRI]), fair for CEUS-LI-RADS category (ĸ = 0.309) and substantial for MRI-LI-RADS category (ĸ = 0.609). Intermodality agreement was fair for arterial hyperenhancement (ĸ = 0.329), slight to fair for “washout” (ĸ = 0.202) and LI-RADS category (ĸ = 0.218)
Conclusion
Interobserver agreement is substantial for MRI-LI-RADS and only fair for CEUS-LI-RADS. This is mostly because interobserver agreement in the perception of washout appearance is better in MRI than in CEUS. Further refinement of the LI-RADS algorithms and increasing education and practice may be necessary to improve the concordance between CEUS and MRI for the final LI-RADS categorization.
Key Points
• CEUS-LI-RADS and MRI-LIRADS enable standardized non-invasive diagnosis of HCC in high-risk patients.
• With CEUS, interobserver agreement is better for arterial hyperenhancement than for “washout”.
• Interobserver agreement for major features is moderate for both CEUS and MRI.
• Interobserver agreement for LI-RADS category is substantial for MRI, and fair for CEUS.
• Interobserver-agreement for CEUS-LI-RADS will presumably improve with ongoing use of the algorithm.




Similar content being viewed by others
Abbreviations
- ACR:
-
American College of Radiology
- bh:
-
Breath-hold
- BMI:
-
Body mass index
- CE-CT:
-
Contrast-enhanced computed tomography
- CE-MRI:
-
Contrast-enhanced magnetic resonance imaging
- CEUS:
-
Contrast-enhanced Ultrasound
- cor:
-
Coronal
- CT:
-
Computed tomography
- DWI:
-
Diffusion-weighted image
- fs:
-
Fat saturation
- GRE:
-
Gradient echo
- HASTE:
-
Half-Fourier acquisition single-shot turbo spin echo
- HCC:
-
Hepatocellular carcinoma
- ICC:
-
Intrahepatic cholangiocellular carcinoma
- LI-RADS:
-
Liver Imaging Reporting and Data System
- LR:
-
LI-RADS category
- MRI:
-
Magnetic resonance imaging
- T:
-
Tesla
- T1w:
-
T1-weighted
- T2w:
-
T2-weighted
- TE:
-
Echo time
- TR:
-
Repetition time
- tra:
-
Transversal
- TSE:
-
Turbo spin echo
- VIBE:
-
Volumetric-interpolated breath-hold examination
References
Westwood M, Joore M, Grutters J et al (2013) Contrast-enhanced ultrasound using SonoVue(R) (sulphur hexafluoride microbubbles) compared with contrast-enhanced computed tomography and contrast-enhanced magnetic resonance imaging for the characterisation of focal liver lesions and detection of liver metastases: a systematic review and cost-effectiveness analysis. Health Technol Assess 17:1–243
Claudon M, Dietrich CF, Choi BI et al (2013) Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver - update 2012: a WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultrasound Med Biol 39:187–210
Bota S, Piscaglia F, Marinelli S, Pecorelli A, Terzi E, Bolondi L (2012) Comparison of international guidelines for noninvasive diagnosis of hepatocellular carcinoma. Liver Cancer 1:190–200
Bruix J, Sherman M (2011) Management of hepatocellular carcinoma: an update. Hepatology 53:1020–1022
Kokudo N, Hasegawa K, Akahane M et al (2015) Evidence-based clinical practice guidelines for hepatocellular carcinoma: The Japan Society of Hepatology 2013 update (3rd JSH-HCC guidelines). Hepatol Res 45. https://doi.org/10.1111/hepr.12464
Friedrich-Rust M, Klopffleisch T, Nierhoff J et al (2013) Contrast-enhanced ultrasound for the differentiation of benign and malignant focal liver lesions: a meta-analysis. Liver Int 33:739–755
Shah S, Shukla A, Paunipagar B (2014) Radiological features of hepatocellular carcinoma. J Clin Exp Hepatol 4:S63–S66
Leoni S, Piscaglia F, Granito A et al (2013) Characterization of primary and recurrent nodules in liver cirrhosis using contrast-enhanced ultrasound: which vascular criteria should be adopted? Ultraschall Med 34:280–287
Mitchell DG, Bruix J, Sherman M, Sirlin CB (2015) LI-RADS (Liver Imaging Reporting and Data System): summary, discussion, and consensus of the LI-RADS Management Working Group and future directions. Hepatology 61:1056–1065
Elsayes KM, Kielar AZ, Agrons MM et al (2017) Liver Imaging Reporting and Data System: an expert consensus statement. J Hepatocell Carcinoma 4:29–39
AWMF-Leitlinie S3 - Leitlinie Deutschland: “Hepatozelluläres Karzinom”, Registernummer 032/053OL Stand: 01.05.2013 , gültig bis 30.04.2018; http://www.awmf.org/uploads/tx_szleitlinien/032-053OLl_S3_Hepatozellul%C3%A4res_Karzinom_Diagnostik_Therapie_2013-verlaengert.pdf accessed: May 19 2017. Available via http://www.awmf.org/uploads/tx_szleitlinien/032-053OLl_S3_Hepatozellul%C3%A4res_Karzinom_Diagnostik_Therapie_2013-verlaengert.pdf. Accessed May 19 2017
Claudon M, Dietrich CF, Choi BI et al (2013) Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver–update 2012: a WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultraschall Med 34:11–29
Strobel D, Bernatik T, Blank W et al (2011) Diagnostic accuracy of CEUS in the differential diagnosis of small (</ = 20 mm) and subcentimetric (</ = 10 mm) focal liver lesions in comparison with histology. Results of the DEGUM multicenter trial. Ultraschall Med 32:593–597
Strobel D, Seitz K, Blank W et al (2009) Tumor-specific vascularization pattern of liver metastasis, hepatocellular carcinoma, hemangioma and focal nodular hyperplasia in the differential diagnosis of 1,349 liver lesions in contrast-enhanced ultrasound (CEUS). Ultraschall Med 30:376–382
Seitz K, Greis C, Schuler A et al (2011) Frequency of tumor entities among liver tumors of unclear etiology initially detected by sonography in the noncirrhotic or cirrhotic livers of 1349 patients. Results of the DEGUM multicenter study. Ultraschall Med 32:598–603
Darnell A, Forner A, Rimola J et al (2015) Liver Imaging Reporting and Data System with MR imaging: evaluation in nodules 20 mm or smaller detected in cirrhosis at screening US. Radiology 275:698–707
Seitz K, Piscaglia F (2013) Ultrasound: the only "one stop shop" for modern management of liver disease. Ultraschall Med 34:500–503
Wildner D, Bernatik T, Greis C, Seitz K, Neurath MF, Strobel D (2015) CEUS in hepatocellular carcinoma and intrahepatic cholangiocellular carcinoma in 320 patients - early or late washout matters: a subanalysis of the DEGUM multicenter trial. Ultraschall Med 36:132–139
Wildner D, Pfeifer L, Goertz RS et al (2014) Dynamic contrast-enhanced ultrasound (DCE-US) for the characterization of hepatocellular carcinoma and cholangiocellular carcinoma. Ultraschall Med 35:522–527
McEvoy SH, McCarthy CJ, Lavelle LP et al (2013) Hepatocellular carcinoma: illustrated guide to systematic radiologic diagnosis and staging according to guidelines of the American Association for the Study of Liver Diseases. Radiographics 33:1653–1668
Seitz K, Bernatik T, Strobel D et al (2010) Contrast-enhanced ultrasound (CEUS) for the characterization of focal liver lesions in clinical practice (DEGUM Multicenter Trial): CEUS vs. MRI–a prospective comparison in 269 patients. Ultraschall Med 31:492–499
Schellhaas B, Wildner D, Pfeifer L et al (2016) LI-RADS-CEUS - proposal for a contrast-enhanced ultrasound algorithm for the diagnosis of hepatocellular carcinoma in high-risk populations. Ultraschall Med 37:627–634
Karlas T (2017) LI-RADS-CEUS for the classification of HCC risk in liver lesions. Z Gastroenterol 55:507–508
Piscaglia F, Wilson SR, Lyshchik A et al (2017) American College of Radiology Contrast Enhanced Ultrasound Liver Imaging Reporting and Data System (CEUS LI-RADS) for the diagnosis of hepatocellular carcinoma: a pictorial essay. Ultraschall Med. https://doi.org/10.1055/s-0042-124661
ACR American College of Radiology: Liver Imaging Reporting and Data System https://www.acr.org/Quality-Safety/Resources/LIRADS. Accessed 12 Sep 2017
Zhang YD, Zhu FP, Xu X et al (2016) Liver Imaging Reporting and Data System: substantial discordance between CT and MR for imaging classification of hepatic nodules. Acad Radiol 23:344–352
Corwin MT, Fananapazir G, Jin M, Lamba R, Bashir MR (2016) Differences in liver imaging and reporting data system categorization between MRI and CT. AJR Am J Roentgenol 206:307–312
Chernyak V, Flusberg M, Law A, Kobi M, Paroder V, Rozenblit AM (2017) Liver Imaging Reporting and Data System: discordance between computed tomography and gadoxetate-enhanced magnetic resonance imaging for detection of hepatocellular carcinoma major features. J Comput Assist Tomogr. https://doi.org/10.1097/rct.0000000000000642
Hope TA, Aslam R, Weinstein S et al (2017) Change in Liver Imaging Reporting and Data System characterization of focal liver lesions using gadoxetate disodium magnetic resonance imaging compared with contrast-enhanced computed tomography. J Comput Assist Tomogr 41:376–381
Barth BK, Donati OF, Fischer MA et al (2016) Reliability, validity, and reader acceptance of LI-RADS-An in-depth analysis. Acad Radiol 23:1145–1153
Bashir MR, Huang R, Mayes N et al (2015) Concordance of hypervascular liver nodule characterization between the organ procurement and transplant network and liver imaging reporting and data system classifications. J Magn Reson Imaging 42:305–314
Davenport MS, Khalatbari S, Liu PS et al (2014) Repeatability of diagnostic features and scoring systems for hepatocellular carcinoma by using MR imaging. Radiology 272:132–142
Giorgio A, Montesarchio L, Gatti P et al (2016) Contrast-enhanced ultrasound: a simple and effective tool in defining a rapid diagnostic work-up for small nodules detected in cirrhotic patients during surveillance. J Gastrointestin Liver Dis 25:205–211
Quaia E, Alaimo V, Baratella E et al (2010) Effect of observer experience in the differentiation between benign and malignant liver tumors after ultrasound contrast agent injection. J Ultrasound Med 29:25–36
Berg WA, D'Orsi CJ, Jackson VP et al (2002) Does training in the Breast Imaging Reporting and Data System (BI-RADS) improve biopsy recommendations or feature analysis agreement with experienced breast imagers at mammography? Radiology 224:871–880
Zhang YD, Zhu FP, Xu X et al (2016) Classifying CT/MR findings in patients with suspicion of hepatocellular carcinoma: comparison of liver imaging reporting and data system and criteria-free Likert scale reporting models. J Magn Reson Imaging 43:373–383
Ehman EC, Behr SC, Umetsu SE et al (2016) Rate of observation and inter-observer agreement for LI-RADS major features at CT and MRI in 184 pathology proven hepatocellular carcinomas. Abdom Radiol (NY) 41:963–969
McHugh ML (2012) Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 22:276–282
Acknowledgements
We thank the editors of European Radiology and those who reviewed this article.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Hannes Seuss.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the institutional review board.
Ethical approval
Institutional review board approval was obtained.
Methodology
• retrospective
• diagnostic study
• performed at one institution
Electronic supplementary material
ESM 1
(DOCX 164 kb)
Rights and permissions
About this article
Cite this article
Schellhaas, B., Hammon, M., Strobel, D. et al. Interobserver and intermodality agreement of standardized algorithms for non-invasive diagnosis of hepatocellular carcinoma in high-risk patients: CEUS-LI-RADS versus MRI-LI-RADS. Eur Radiol 28, 4254–4264 (2018). https://doi.org/10.1007/s00330-018-5379-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5379-1