Abstract
Objectives
To assess the clinical feasibility of US-US image overlay fusion with evaluation of the ablative margin in radiofrequency ablation (RFA) for hepatocellular carcinoma (HCC).
Methods
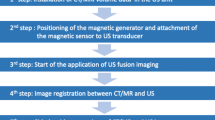
Fifty-three patients with 68 HCCs measuring 0.9–4.0 cm who underwent RFA guided by US-US overlay image fusion were included in this retrospective study. By an overlay of pre-/postoperative US, the tumor image could be projected onto the ablative hyperechoic zone. Therefore, the ablative margin three-dimensionally could be shown during the RFA procedure. US-US image overlay was compared to dynamic CT a few days after RFA for assessment of early treatment response. Accuracy of graded response was calculated, and the performance of US-US image overlay fusion was compared with that of CT using a Kappa agreement test.
Results
Technically effective ablation was achieved in a single session, and 59 HCCs (86.8 %) succeeded in obtaining a 5-mm margin on CT. The response with US-US image overlay correctly predicted early CT evaluation with an accuracy of 92.6 % (63/68) (k = 0.67; 95 % CI: 0.39–0.95).
Conclusion
US-US image overlay fusion can be proposed as a feasible guidance in RFA with a safety margin and predicts early response of treatment assessment with high accuracy.
Key points
• US-US image overlay fusion visualizes the ablative margin during RFA procedure.
• Visualizing the margin during the procedure can prompt immediate complementary treatment.
• US image fusion correlates with the results of early evaluation CT.



Similar content being viewed by others
Abbreviations
- 3D:
-
Three-dimensional
- BCLC:
-
Barcelona clinic liver cancer
- CEUS:
-
Contrast-enhanced ultrasonography
- HCC:
-
Hepatocellular carcinoma
- MDCT:
-
Multidetector CT
- MPR:
-
Multiplanar reconstruction
- RFA:
-
Radiofrequency ablation
- ROI:
-
Region of interest
- SD:
-
Standard deviation
- US:
-
Ultrasound
References
Chen MS, Li JQ, Zheng Y et al (2006) A prospective randomized trial comparing percutaneous local ablative therapy and partial hepatectomy for small hepatocellular carcinoma. Ann Surg 243:321–328
Takayama T, Makuuchi M, Hasegawa K (2010) Single HCC smaller than 2 cm: surgery or ablation? a surgeon's perspective. J Hepatobiliary Pancreat Sci 17(4):422–424
Wang JH, Wang CC, Hung CH, Chen CL, Lu SN (2012) Survival comparison between surgical resection and radiofrequency ablation for patients in BCLC very early/early stage hepatocellular carcinoma. J Hepatol 56(2):412–418
Peng ZW, Lin XJ, Zhang YJ et al (2012) Radiofrequency ablation versus hepatic resection for the treatment of hepatocellular carcinomas 2 cm or smaller: a retrospective comparative study. Radiology 262(3):1022–1033
Huang J, Yan L, Cheng Z et al (2010) A randomized trial comparing radiofrequency ablation and surgical resection for HCC conforming to the Milan criteria. Ann Surg 252(6):903–912
Feng K, Yan J, Li X et al (2012) A randomized controlled trial of radiofrequency ablation and surgical resection in the treatment of small hepatocellular carcinoma. J Hepatol 57(4):794–802
Imai K, Beppu T, Chikamoto A et al (2013) Comparison between hepatic resection and radiofrequency ablation as first-line treatment for solitary small-sized hepatocellular carcinoma of 3 cm or less. Hepatol Res 43(8):853–864
Liu PH, Hsu CY, Hsia CY et al (2016) Surgical Resection Versus Radiofrequency Ablation for Single Hepatocellular Carcinoma ≤ 2 cm in a Propensity Score Model. Ann Surg 263(3):538–545
Liu CH, Arellano RS, Uppot RN, Samir AE, Gervais DA, Mueller PR (2010) Radiofrequency ablation of hepatic tumours: effect of post-ablation margin on local tumour progression. Eur Radiol 20(4):877–885
Minami Y, Kudo M (2010) Radiofrequency ablation of hepatocellular carcinoma: Current status. World J Radiol 2(11):417–424
Minami Y, Nishida N, Kudo M (2014) Therapeutic response assessment of RFA for HCC: contrast-enhanced US, CT and MRI. World J Gastroenterol 20(15):4160–4166
Goldberg SN, Grassi CJ, Cardella JF et al (2005) Image-guided tumor ablation: standardization of terminology and reporting criteria. J Vasc Interv Radiol 16:765–778
Nishikawa H, Inuzuka T, Takeda H et al (2011) Percutaneous radiofrequency ablation therapy for hepatocellular carcinoma: a proposed new grading system for the ablative margin and prediction of local tumor progression and its validation. J Gastroenterol 46(12):1418–1426
Nishikawa H, Osaki Y, Iguchi E et al (2013) Radiofrequency ablation for hepatocellular carcinoma: the relationship between a new grading system for the ablative margin and clinical outcomes. J Gastroenterol 48(8):951–965
Leyendecker JR, Dodd GD 3rd, Halff GA et al (2002) Sonographically observed echogenic response during intraoperative radiofrequency ablation of cirrhotic livers: pathologic correlation. AJR Am J Roentgenol 178(5):1147–1151
Zytoon AA, Ishii H, Murakami K et al (2007) Recurrence-free survival after radiofrequency ablation of hepatocellular carcinoma. A registry report of the impact of risk factors on outcome. Jpn J Clin Oncol 37(9):658–672
Minami Y, Chung H, Kudo M, at al. (2008) Radiofrequency ablation of hepatocellular carcinoma: value of virtual CT sonography with magnetic navigation. AJR Am J Roentgenol 190(6):W335–W341
Kitada T, Murakami T, Kuzushita N et al (2008) Effectiveness of real-time virtual sonography-guided radiofrequency ablation treatment for patients with hepatocellular carcinomas. Hepatol Res 38(6):565–571
Song KD, Lee MW, Rhim H, Cha DI, Chong Y, Lim HK (2013) Fusion imaging-guided radiofrequency ablation for hepatocellular carcinomas not visible on conventional ultrasound. AJR Am J Roentgenol 201(5):1141–1147
Makino Y, Imai Y, Igura T et al (2016) Feasibility of Extracted-Overlay Fusion Imaging for Intraoperative Treatment Evaluation of Radiofrequency Ablation for Hepatocellular Carcinoma. Liver Cancer 5(4):269–279
Minami Y, Minami T, Chishina H et al (2016) US-US Fusion Imaging in Radiofrequency Ablation for Liver Metastases. Dig Dis 34(6):687–691
Bruix J, Sherman M, Practice Guidelines Committee, American Association for the Study of Liver Diseases (2005) Management of hepatocellular carcinoma. Hepatology 42(5):1208–1236
Kim YS, Rhim H, Lim HK, Choi D, Lee MW, Park MJ (2011) Coagulation necrosis induced by radiofrequency ablation in the liver: histopathologic and radiologic review of usual to extremely rare changes. Radiographics 31(2):377–390
Orth RC, Guillerman RP, Zhang W, Masand P, Bisset GS 3rd (2014) Prospective comparison of MR imaging and US for the diagnosis of pediatric appendicitis. Radiology 272(1):233–240
Martin ML, Tay KH, Flak B et al (2003) Multidetector CT angiography of the aortoiliac system and lower extremities: a prospective comparison with digital subtraction angiography. AJR Am J Roentgenol 180(4):1085–1091
Viera AJ, Garrett JM (2005) Understanding interobserver agreement: the kappa statistic. Fam Med 37(5):360–363
Costa AF, Kajal D, Pereira A, Atri M (2017) Should fat in the radiofrequency ablation zone of hepatocellular adenomas raise suspicion for residual tumour? Eur Radiol 27(4):1704–1712
Germani G, Pleguezuelo M, Gurusamy K et al (2010) Clinical outcomes of radiofrequency ablation, percutaneous alcohol and acetic acid injection for hepatocelullar carcinoma: a meta-analysis. J Hepatol 52(3):380–388
Tanis E, Nordlinger B, Mauer M et al (2014) Local recurrence rates after radiofrequency ablation or resection of colorectal liver metastases. Analysis of the European Organisation for Research and Treatment of Cancer #40004 and #40983. Eur J Cancer 50(5):912–919
Donadon M, Solbiati L, Dawson L et al (2016) Hepatocellular Carcinoma: The Role of Interventional Oncology. Liver Cancer 6(1):34–43
Granata V, Petrillo M, Fusco R et al (2013) Surveillance of HCC Patients after Liver RFA: Role of MRI with Hepatospecific Contrast versus Three-Phase CT Scan-Experience of High Volume Oncologic Institute. Gastroenterol Res Pract 2013:469097. https://doi.org/10.1155/2013/469097
Kang TW, Rhim H, Lee J et al (2016) Magnetic resonance imaging with gadoxetic acid for local tumour progression after radiofrequency ablation in patients with hepatocellular carcinoma. Eur Radiol 26(10):3437–3446
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Prof. Masatoshi Kudo.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• case-control study
• performed at one institution
Rights and permissions
About this article
Cite this article
Minami, Y., Minami, T., Hagiwara, S. et al. Ultrasound-ultrasound image overlay fusion improves real-time control of radiofrequency ablation margin in the treatment of hepatocellular carcinoma. Eur Radiol 28, 1986–1993 (2018). https://doi.org/10.1007/s00330-017-5162-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-5162-8