Abstract
Objective
To compare the diagnostic performances of strain elastography (SE) and shear-wave elastography (SWE) for predicting response to neoadjuvant chemotherapy (NACT) in patients with breast cancer.
Methods
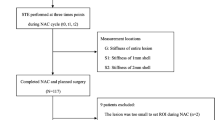
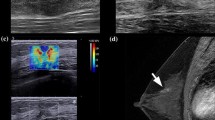
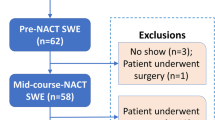
This prospective study recruited 71 eligible patients from June 2014 to May 2016. All patients provided written informed consent. Tumour stiffness was assessed by the SE strain ratio (R), SWE maximum elasticity (Emax) and SWE mean elasticity (Emean). Ultrasonic elastography (UE) assessments were performed at each NACT cycle (t1 − t6). For the purpose of predicting, the relative changes in elastographic parameters after the first and second NACT cycles were considered as the variables [Δ(t1) and Δ(t2)]. The area under the receiver operating characteristics (AUC) curve was compared.
Results
ΔEmean(t2) and R2 displayed the best diagnostic performances within their own modalities (AUC = 0.93 and 0.90 for predicting favourable response to NACT; AUC = 0.92 and 0.78 for predicting NACT resistance, respectively). There were no significant differences in AUCs for ΔEmean(t2) and some UE parameters (P > 0.05). By contrast, ΔEmean(t2) was significantly superior to all other SE parameters for predicting resistance (P < 0.05).
Conclusions
SE and SWE exhibited similar performances for predicting favourable NACT responses; SWE was better than SE for predicting NACT resistance.
Key Points
• Elastography parameters after the second NACT cycle showed the best diagnostic performances.
• SWE and SE yielded similar diagnostic performances in predicting favourable responses.
• SWE performed better than SE in predicting the pathological resistance to NACT.
• Discrepant results may be due to the breast thickness and lesion depth.





Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the ROC
- Emax :
-
Maximum elasticity
- Emean :
-
Mean elasticity
- NACT:
-
Neoadjuvant chemotherapy
- pCR:
-
Pathological complete response
- RCB:
-
Residual cancer burden
- ROC:
-
Receiver operating characteristics
- ROI:
-
Region of interest
- R:
-
Strain ratio
- SE:
-
Strain elastography
- SWE:
-
Shear-wave elastography
- UE:
-
Ultrasounic elastography
References
Barr RG, Nakashima K, Amy D et al (2015) WFUMB guidelines and recommendations for clinical use of ultrasound elastography: part 2: breast. Ultrasound Med Biol 41:1148–1160
Balleyguier C, Ciolovan L, Ammari S et al (2013) Breast elastography: the technical process and its applications. Diagn Interv Imaging 94:503–513
Berg WA, Cosgrove DO, Dore CJ et al (2012) Shear-wave elastography improves the specificity of breast US: the BE1 multinational study of 939 masses. Radiology 262:435–449
Bae JS, Chang JM, Lee SH, Shin SU, Moon WK (2016) Prediction of invasive breast cancer using shear-wave elastography in patients with biopsy-confirmed ductal carcinoma in situ. Eur Radiol. doi:10.1007/s00330-016-4359-6
Berg WA, Mendelson EB, Cosgrove DO et al (2015) Quantitative maximum shear-wave stiffness of breast masses as a predictor of histopathologic severity. AJR Am J Roentgenol 205:448–455
Choi WJ, Kim HH, Cha JH et al (2014) Predicting prognostic factors of breast cancer using shear wave elastography. Ultrasound Med Biol 40:269–274
Evans A, Armstrong S, Whelehan P et al (2013) Can shear-wave elastography predict response to neoadjuvant chemotherapy in women with invasive breast cancer? Br J Cancer 109:2798–2802
Hayashi M, Yamamoto Y, Ibusuki M et al (2012) Evaluation of tumor stiffness by elastography is predictive for pathologic complete response to neoadjuvant chemotherapy in patients with breast cancer. Ann Surg Oncol 19:3042–3049
King TA, Morrow M (2015) Surgical issues in patients with breast cancer receiving neoadjuvant chemotherapy. Nat Rev Clin Oncol 12:335–343
Cho N, Im SA, Kang KW et al (2016) Early prediction of response to neoadjuvant chemotherapy in breast cancer patients: comparison of single-voxel (1)H-magnetic resonance spectroscopy and (18)F-fluorodeoxyglucose positron emission tomography. Eur Radiol 26:2279–2290
Chang JM, Moon WK, Cho N, Kim SJ (2011) Breast mass evaluation: factors influencing the quality of US elastography. Radiology 259:59–64
Barr RG (2012) Sonographic breast elastography: a primer. J Ultrasound Med 31:773–783
Chang JM, Won JK, Lee KB, Park IA, Yi A, Moon WK (2013) Comparison of shear-wave and strain ultrasound elastography in the differentiation of benign and malignant breast lesions. AJR Am J Roentgenol 201:W347–356
Youk JH, Son EJ, Gweon HM, Kim H, Park YJ, Kim JA (2014) Comparison of strain and shear wave elastography for the differentiation of benign from malignant breast lesions, combined with B-mode ultrasonography: qualitative and quantitative assessments. Ultrasound Med Biol 40:2336–2344
Gahlaut R, Bennett A, Fatayer H et al (2016) Effect of neoadjuvant chemotherapy on breast cancer phenotype, ER/PR and HER2 expression - Implications for the practising oncologist. Eur J Cancer 60:40–48
Fei F, Messina C, Slaets L et al (2015) Tumour size is the only predictive factor of distant recurrence after pathological complete response to neoadjuvant chemotherapy in patients with large operable or locally advanced breast cancers: a sub-study of EORTC 10994/BIG 1-00 phase III trial. Eur J Cancer 51:301–309
Jung NY, Park CS, Kim SH et al (2016) Sonoelastographic strain ratio: how does the position of reference fat influence it? Jpn J Radiol 34:440–447
Itoh A, Ueno E, Tohno E et al (2006) Breast disease: clinical application of US elastography for diagnosis. Radiology 239:341–350
Symmans WF, Peintinger F, Hatzis C et al (2007) Measurement of residual breast cancer burden to predict survival after neoadjuvant chemotherapy. J Clin Oncol 25:4414–4422
Vriens BE, de Vries B, Lobbes MB et al (2016) Ultrasound is at least as good as magnetic resonance imaging in predicting tumour size post-neoadjuvant chemotherapy in breast cancer. Eur J Cancer 52:67–76
Lee SH, Chang JM, Han W et al (2015) Shear-wave elastography for the detection of residual breast cancer after neoadjuvant chemotherapy. Ann Surg Oncol 22:376–384
Jing H, Cheng W, Li ZY et al (2016) Early evaluation of relative changes in tumor stiffness by shear wave elastography predicts the response to neoadjuvant chemotherapy in patients with breast cancer. J Ultrasound Med 35:1619–1627
Cosgrove DO, Berg WA, Dore CJ et al (2012) Shear wave elastography for breast masses is highly reproducible. Eur Radiol 22:1023–1032
Barr RG, Zhang Z (2012) Effects of precompression on elasticity imaging of the breast: development of a clinically useful semiquantitative method of precompression assessment. J Ultrasound Med 31:895–902
Song G, Jing L, Yan M, Cong S, Xuejiao W (2015) Influence of various breast factors on the quality of strain elastograms. J Ultrasound Med 34:395–400
Bamber J, Cosgrove D, Dietrich CF et al (2013) EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 1: Basic principles and technology. Ultraschall Med 34:169–184
Aalders KC, van Bommel AC, van Dalen T et al (2016) Contemporary risks of local and regional recurrence and contralateral breast cancer in patients treated for primary breast cancer. Eur J Cancer 63:118–126
Hayashi M, Yamamoto Y, Sueta A et al (2015) Associations between elastography findings and clinicopathological factors in breast cancer. Medicine (Baltimore) 94, e2290
Evans A, Rauchhaus P, Whelehan P et al (2014) Does shear wave ultrasound independently predict axillary lymph node metastasis in women with invasive breast cancer? Breast Cancer Res Treat 143:153–157
Ma Y, Li G, Li J, Ren WD (2015) The diagnostic value of superb microvascular imaging (SMI) in detecting blood flow signals of breast lesions: a preliminary study comparing smi to color doppler flow imaging. Medicine (Baltimore) 94, e1502
Acknowledgements
The scientific guarantor of this publication is Weidong Ren. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. This study has received funding by Fundamental Research Funds of Shengjing Hospital, China Medical University (MD63) and Science and Technology Project Funds from Education Department of Liaoning Province(LK201621). Qijun Wu, Chao Ji and Liqiang Zheng kindly provided statistical advice for this manuscript. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Methodology: prospective, diagnostic or prognostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ma, Y., Zhang, S., Li, J. et al. Comparison of strain and shear-wave ultrasounic elastography in predicting the pathological response to neoadjuvant chemotherapy in breast cancers. Eur Radiol 27, 2282–2291 (2017). https://doi.org/10.1007/s00330-016-4619-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4619-5