Abstract
Objectives
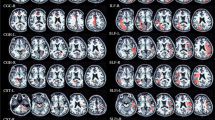
Application of multifrequency magnetic resonance elastography (MMRE) of the brain parenchyma in patients with neuromyelitis optica spectrum disorder (NMOSD) compared to age matched healthy controls (HC).
Methods
15 NMOSD patients and 17 age- and gender-matched HC were examined using MMRE. Two three-dimensional viscoelastic parameter maps, the magnitude |G*| and phase angle φ of the complex shear modulus were reconstructed by simultaneous inversion of full wave-field data in 1.9-mm isotropic resolution at 7 harmonic drive frequencies from 30 to 60 Hz.
Results
In NMOSD patients, a significant reduction of |G*| was observed within the white matter fraction (p = 0.017), predominantly within the thalamic regions (p = 0.003), compared to HC. These parameters exceeded the reduction in brain volume measured in patients versus HC (p = 0.02 whole-brain volume reduction). Volumetric differences in white matter fraction and the thalami were not detectable between patients and HC. However, phase angle φ was decreased in patients within the white matter (p = 0.03) and both thalamic regions (p = 0.044).
Conclusions
MMRE reveals global tissue degeneration with accelerated softening of the brain parenchyma in patients with NMOSD. The predominant reduction of stiffness is found within the thalamic region and related white matter tracts, presumably reflecting Wallerian degeneration.
Key Points
• Magnetic resonance elastography reveals diffuse cerebral tissue changes in patients with NMOSD.
• Premature tissue softening in NMOSD patients indicates tissue degeneration.
• Hypothesis of a widespread cerebral neurodegeneration in form of diffuse tissue alteration.




Similar content being viewed by others
Abbreviations
- AQP4:
-
Aquaporin 4 channel
- MDEV inversion:
-
Multifrequency dual elasco-visco inversion
- MMRE:
-
Multifrequency magnetic resonance elastography
- NMO:
-
Neuromyelitis optica
- NMOSD:
-
Neuromyelitis optica spectrum disorder
References
Jarius S, Wildemann B, Paul F (2014) Neuromyelitis optica: clinical features, immunopathogenesis and treatment. Clin Exp Immunol 176:149–164
Jarius S, Paul F, Franciotta D, Waters P, Zipp F, Hohlfeld R et al (2008) Mechanisms of disease: aquaporin-4 antibodies in neuromyelitis optica. Nat Clin Pract Neurol 4:202–214
Zekeridou A, Lennon VA (2015) Aquaporin-4 autoimmunity. Neurol Neuroimmunol Neuroinflamm 2, e110
Metz I, Beißbarth T, Ellenberger D, Pache F, Stork L, Ringelstein M et al (2016) Serum peptide reactivities may distinguish neuromyelitis optica subgroups and multiple sclerosis. Neurol Neuroimmunol Neuroinflamm 3, e204
Wingerchuk DM, Lennon VA, Pittock SJ, Lucchinetti CF, Weinshenker BG (2006) Revised diagnostic criteria for neuromyelitis optica. Neurology 66:1485–1489
Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T et al (2015) International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 85:177–189
Kister I, Paul F (2015) Pushing the boundaries of neuromyelitis optica: does antibody make the disease? Neurology 85:118–119
Matthews L, Marasco R, Jenkinson M, Küker W, Luppe S, Leite MI et al (2013) Distinction of seropositive NMO spectrum disorder and MS brain lesion distribution. Neurology 80:1330–1337
Jarius S, Ruprecht K, Wildemann B, Kuempfel T, Ringelstein M, Geis C et al (2012) Contrasting disease patterns in seropositive and seronegative neuromyelitis optica: a multicentre study of 175 patients. J Neuroinflammation 9:14
Kim HJ, Paul F, Lana-Peixoto MA, Tenembaum S, Asgari N, Palace J et al (2015) MRI characteristics of neuromyelitis optica spectrum disorder: an international update. Neurology 84:1165–1173
Kremer S, Renard F, Achard S, Lana-Peixoto MA, Palace J, Asgari N et al (2015) Use of advanced magnetic resonance imaging techniques in neuromyelitis optica spectrum disorder. JAMA Neurol 72:815–822
Zhang N, Li YJ, Fu Y, Shao JH, Luo LL, Yang L et al (2015) Cognitive impairment in Chinese neuromyelitis optica. Mult Scler 21:1839–1846
Muthupillai R, Ehman RL (1996) Magnetic resonance elastography. Nat Med 2:601–603
Kruse SA, Rose GH, Glaser KJ, Manduca A, Felmlee JP, Jack CR et al (2008) Magnetic resonance elastography of the brain. NeuroImage 39:231–237
Green MA, Bilston LE, Sinkus R (2008) In vivo brain viscoelastic properties measured by magnetic resonance elastography. NMR Biomed 21:755–764
Sack I, Beierbach B, Hamhaber U, Klatt D, Braun J (2008) Non-invasive measurement of brain viscoelasticity using magnetic resonance elastography. NMR Biomed 21:265–271
Sack I, Streitberger K-J, Krefting D, Paul F, Braun J (2011) The influence of physiological aging and atrophy on brain viscoelastic properties in humans. PLoS ONE 6, e23451
Sack I, Beierbach B, Wuerfel J, Klatt D, Hamhaber U, Papazoglou S et al (2009) The impact of aging and gender on brain viscoelasticity. NeuroImage 46:652–657
Freimann FB, Streitberger K-J, Klatt D, Lin K, McLaughlin J, Braun J et al (2012) Alteration of brain viscoelasticity after shunt treatment in normal pressure hydrocephalus. Neuroradiology 54:189–196
Streitberger K-J, Sack I, Krefting D, Pfüller C, Braun J, Paul F et al (2012) Brain viscoelasticity alteration in chronic-progressive multiple sclerosis. PLoS ONE 7, e29888
Streitberger K-J, Wiener E, Hoffmann J, Freimann FB, Klatt D, Braun J et al (2011) In vivo viscoelastic properties of the brain in normal pressure hydrocephalus. NMR Biomed 24:385–392
Reiss-Zimmermann M, Streitberger K-J, Sack I, Braun J, Arlt F, Fritzsch D, et al (2015) High Resolution imaging of viscoelastic properties of intracranial tumours by multi-frequency magnetic resonance elastography. Clin Neuroradiol 25:371–378
Wuerfel J, Paul F, Beierbach B, Hamhaber U, Klatt D, Papazoglou S et al (2010) MR-elastography reveals degradation of tissue integrity in multiple sclerosis. NeuroImage 49:2520–2525
Lipp A, Trbojevic R, Paul F, Fehlner A, Hirsch S, Scheel M et al (2013) Cerebral magnetic resonance elastography in supranuclear palsy and idiopathic Parkinson’s disease. Neuroimage Clin 3:381–387
Murphy MC, Huston J, Jack CR, Glaser KJ, Manduca A, Felmlee JP et al (2011) Decreased brain stiffness in Alzheimer’s disease determined by magnetic resonance elastography. J Magn Reson Imaging 34:494–498
Huston J, Murphy MC, Boeve BF, Fattahi N, Arani A, Glaser KJ et al (2016) Magnetic resonance elastography of frontotemporal dementia. J Magn Reson Imaging 43:474–478
Fehlner A, Behrens JR, Streitberger K-J, Papazoglou S, Braun J, Bellmann-Strobl J et al (2016) Higher-resolution MR elastography reveals early mechanical signatures of neuroinflammation in patients with clinically isolated syndrome. J Magn Reson Imaging 44:51–58
Riek K, Millward JM, Hamann I, Mueller S, Pfueller CF, Paul F et al (2012) Magnetic resonance elastography reveals altered brain viscoelasticity in experimental autoimmune encephalomyelitis. Neuroimage Clin 1:81–90
Freimann FB, Müller S, Streitberger K-J, Guo J, Rot S, Ghori A et al (2013) MR elastography in a murine stroke model reveals correlation of macroscopic viscoelastic properties of the brain with neuronal density. NMR Biomed 26:1534–1539
Millward JM, Guo J, Berndt D, Braun J, Sack I, Infante-Duarte C (2015) Tissue structure and inflammatory processes shape viscoelastic properties of the mouse brain. NMR Biomed 28:831–839
Hirsch S, Guo J, Reiter R, Papazoglou S, Kroencke T, Braun J et al (2014) MR elastography of the liver and the spleen using a piezoelectric driver, single-shot wave-field acquisition, and multifrequency dual parameter reconstruction. Magn Reson Med 71:267–277
Hirsch S, Klatt D, Freimann F, Scheel M, Braun J, Sack I (2012) In vivo measurement of volumetric strain in the human brain induced by arterial pulsation and harmonic waves. Magn Reson Med 70:671–683
Rump J, Klatt D, Braun J, Warmuth C, Sack I (2007) Fractional encoding of harmonic motions in MR elastography. Magn Reson Med 57:388–395
Sinnecker T, Dörr J, Pfueller CF, Harms L, Ruprecht K, Jarius S et al (2012) Distinct lesion morphology at 7-T MRI differentiates neuromyelitis optica from multiple sclerosis. Neurology 79:708–714
Paul F, Jarius S, Aktas O, Bluthner M, Bauer O, Appelhans H et al (2007) Antibody to aquaporin 4 in the diagnosis of neuromyelitis optica. PLoS Med 4, e133
Lennon VA, Kryzer TJ, Pittock SJ, Verkman AS, Hinson SR (2005) IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. J Exp Med 202:473–477
Jarius S, Wildemann B (2010) AQP4 antibodies in neuromyelitis optica: diagnostic and pathogenetic relevance. Nat Rev Neurol 6:383–392
Trebst C, Jarius S, Berthele A, Paul F, Schippling S, Wildemann B et al (2014) Update on the diagnosis and treatment of neuromyelitis optica: recommendations of the Neuromyelitis Optica Study Group (NEMOS). J Neurol 261:1–16
Sack I (2013) Magnetic resonance elastography 2.0: high resolution imaging of soft tissue elasticity, viscosity and pressure. Dtsch Med Wochenschr 138:2426–2430
Jiang X, Asbach P, Streitberger K-J, Thomas A, Hamm B, Braun J et al (2014) In vivo high-resolution magnetic resonance elastography of the uterine corpus and cervix. Eur Radiol 24:3025–3033
Guo J, Hirsch S, Streitberger KJ, Kamphues C, Asbach P, Braun J et al (2014) Patient-activated three-dimensional multifrequency magnetic resonance elastography for high-resolution mechanical imaging of the liver and spleen. Röfo 186:260–266
Guo J, Büning C, Schott E, Kröncke T, Braun J, Sack I et al (2015) In vivo abdominal magnetic resonance elastography for the assessment of portal hypertension before and after transjugular intrahepatic portosystemic shunt implantation. Investig Radiol 50:347–351
Sack I, Joehrens K, Wuerfel J, Braun J (2013) Structure sensitive elastography: on the viscoelastic powerlaw behaviour of an in vivo human tissue in health and disease. Soft Matter 9:5672–5680
Morrison JH, Hof PR (1997) Life and death of neurons in the aging brain. Science 278:412–419
Hrapko M, van Dommelen JA, Peters GW, Wismans JS (2008) The influence of test conditions on characterization of the mechanical properties of brain tissue. J Biomech Eng 130:031003
Matthews L, Kolind S, Brazier A, Leite MI, Brooks J, Traboulsee A et al (2015) Imaging surrogates of disease activity in neuromyelitis optica allow distinction from multiple sclerosis. PLoS ONE 10, e0137715
Pache F, Zimmermann H, Finke C, Lacheta A, Papazoglou S, Kuchling J, et al (2016) Brain parenchymal damage in neuromyelitis optica spectrum disorder - a multimodal MRI study. Eur Radiol. doi:10.1007/s00330-016-4282-x
Finke C, Heine J, Pache F, Lacheta A, Borisow N, Kuchling J et al (2016) Normal volumes and microstructural integrity of deep gray matter structures in AQP4+ NMOSD. Neurol Neuroimmunol Neuroinflamm 3, e229
Jonietz E (2012) Mechanics: the forces of cancer. Nature 491:S56–S57
Acknowledgement
AF acknowledges a scholarship of the Hanns Seidel Foundation. This work was supported by the German Research Foundation (DFG Exc 257 to FP, DFG 901/17 to IS) and by Bundesministerium für Bildung und Forschung (Competence Network Multiple Sclerosis to FP, FP, KR). The authors thank Susan Pikol and Cynthia Kraut for excellent technical assistance.
The scientific guarantor of this publication is Jens Würfel. The authors of this manuscript declare relationships with the following companies: Alexion, Chugai, Biogen, MedImmune, Teva, MerckSerono, Bayer, Novartis, Roche, SanofiGenzyme, Shire. No complex statistical methods were necessary for this paper. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Some study subjects or cohorts have been previously reported in Pache F, Zimmermann H, Finke C, et al. (2016) Brain parenchymal damage in neuromyelitis optica spectrum disorder - A multimodal MRI study. Eur Radiol online first: 24 March 2016. DOI 10.1007/s00330-016-4282-x
Methodology: prospective, case-control study, observational, performed at one institution
Author information
Authors and Affiliations
Corresponding author
Additional information
Kaspar-Josche Streitberger and Andreas Fehlner contributed equally to this work.
Rights and permissions
About this article
Cite this article
Streitberger, KJ., Fehlner, A., Pache, F. et al. Multifrequency magnetic resonance elastography of the brain reveals tissue degeneration in neuromyelitis optica spectrum disorder. Eur Radiol 27, 2206–2215 (2017). https://doi.org/10.1007/s00330-016-4561-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4561-6