Abstract
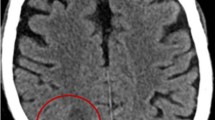
Central nervous system infections, which are rarely seen in systemic lupus erythematosus (SLE), have considerably high mortality but they are difficult to distinguish from neuropsychiatric manifestation of lupus. This article reports the case of a patient with SLE with brain abscess which developed during immunosuppressive therapy for lupus nephritis. The patient completely recovered without neurological sequelae by open surgical drainage and 12-week antibiotic therapy. It is recommended that CNS infections must be excluded in patients with SLE, particularly who are receiving immunosuppressive therapy.


Similar content being viewed by others
References
Ospina FE, Echeverri A, Zambrano D, Suso JP, Martínez-Blanco J, Cañas CA, Tobón GJ (2017) Distinguishing infections vs flares in patients with systemic lupus erythematosus. Rheumatology;56 (suppl_1):i46–i54. https://doi.org/10.1093/rheumatology/kew340
Danza A, Ruiz-Irastorza G (2013) Infection risk in systemic lupus erythematosus patients: susceptibility factors and preventive strategies. Lupus 22:1286–1294. https://doi.org/10.1177/0961203313493032
Horta-Baas G, Guerrero-Soto O, Barile-Fabris L (2013) Central nervous system infection by listeria monocytogenes in patients with systemic lupus erythematosus: analysis of 26 cases, including the report of a new case. Reumatol Clin 9(6):340–347. https://doi.org/10.1016/j.reuma.2013.04.011
Yang CD, Wang XD, Ye S, Gu YY, Bao CD, Wang Y, Chen SL (2007) Clinical features, prognostic and risk factors of central nervous system infections in patients with systemic lupus erythematosus. Clin Rheumatol 26:895–901. https://doi.org/10.1007/s10067-006-0424-x
Vargas PJ, King G, Navarra SV (2009) Central nervous system infections in filipino patients with systemic lupus erythematosus. Int J Rheum Dis 12(3):234–238. https://doi.org/10.1111/j.1756-185X.2009.01416.x
David JHetem, Suzan HM, Rooijakkers, Miquel BEkkelenkamp (2017) Staphylococci and Micrococci. In: Jonathan Cohen WG, Powderly, Opal SM (eds) Infectious diseases, 4th edn, Volume 2, pp 1509–1522
Jeong JH, Moon SM, Park PW, Ahn JY, Kim KH, Seo JY, Lee HT, Jae KW, Seo YH (2017) multiple brain abscesses caused by Nocardia asiatica in a patient with systemic lupus erythematosus: the first case report and literature review. Ann Lab Med 37(5):459–461. https://doi.org/10.3343/alm.2017.37.5.459
Sakarunchai I, Saeheng S, Oearsakul T, Sanghan N (2016) Listeria monocytogenes brain abscess on MR imaging mimicking the track of a migrating worm like a sparganum: a case report. Interdiscipl Neurosurg 5:9–11. https://doi.org/10.1016/j.inat.2016.03.008
Perini G, Pravettoni R, Farina E, Grande G, Contri P, Mariani C (2015) Listeria brain abscesses during administration of mycophenolate mofetil for systemic lupus erythematosus: a case report. Neurol Sci 36(6):1019–1020. https://doi.org/10.1007/s10072-014-1969-0
Ueda Y, Yamamoto K, Watanabe K, Yamashita H, Ohmagari N, Mimori A (2014) Obstructive pneumonia and brain abscess due to Nocardia elegans in a patient with systemic lupus erythematosus. Kansenshogaku Zasshi 88(3):282–287. (Japanase)
Prasad BNS, Misra R, Agarwal V, Lawrence A, Aggarwal A (2014) Nocardia infection in SLE: a case series of three patients. Indian J Rheumatol 9(2):53–56. https://doi.org/10.1016/j.injr.2014.02.004
Fei Y, Shi X, Gan F, Li X, Zhang W, Li M, Hou Y, Zhang X, Zhao Y, Zeng X, Zhang F (2014) Death causes and pathogens analysis of systemic lupus erythematosus during the past 26 years. Clin Rheumatol 33:57–63. https://doi.org/10.1007/s10067-013-2383-3
Xu Y, Xu D, Zhang T, Leng X-M, Zhang F-C, Zeng X-F (2012) The prevalence and clinical characteristics of systemic lupus erythematosus with infectious brain lesions in China. Scand J Rheumatol 41:466–471. https://doi.org/10.3109/03009742.2012.680607
Baizabal-Carvallo JF, Delgadillo-Márquez G, Estañol B, García-Ramos G (2009) Clinical characteristics and outcomes of the meningitides in systemic lupus erythematosus. Eur Neurol 61:143–148. https://doi.org/10.1159/000186504
.Cone LA, Somero MS, Qureshi FJ, Kerkar S, Byrd RG, Hirschberg JM, Gauto AR (2008) Unusual infections due to Listeria monocytogenes in the Southern California desert. Int J Infect Dis 12:578–581. https://doi.org/10.1016/j.ijid.2007.12.003
Hernández-Belmonte A, Mateos-Rodríguez F, Andrés-Mompean E, PalomarPérez J (2008) Bacteremia, absceso cerebral y meningitis por Listeria monocytogenes. Enferm Infecc Microbiol Clin 26:318–319. https://doi.org/10.1157/13120425
Amr SS, Al-Tawfiq JA (2007) Aspiration cytology of brain abscess from a fatal case of cerebral phaeohyphomycosis due to Ramichloridium mackenziei. Diagn Cytopathol 35(11):695–699. https://doi.org/10.1002/dc.20724
Justiniano M, Glorioso S, Dold S, Espinoza LR (2007) Nocardia brain abscesses in a male patient with SLE: successful outcome despite delay in diagnosis. Clin Rheumatol 26(6):1020–1022. https://doi.org/10.1007/s10067-006-0262-x
Kilincer C, Hamamcioglu MK, Simsek O, Hicdonmez T, Aydoslu B, Tansel O, Tiryaki M, Soy M, Tatman-Otkun M, Cobanoglu S (2006) Nocardial brain abscess: review of clinical management. J Clin Neurosci 13(4):481–485. https://doi.org/10.1016/j.jocn.2005.04.031
Geramishoar M, Zomorodian K, Zaini F, Saadat F, Tarazooie B, Norouzi M, Rezaie S (2004) First case of cerebral phaeohyphomycosis caused by Nattrassia mangiferae in Iran. Jpn J Infect Dis 57(6):285–286
Yoneyama T, Yamakami I, Mine S, Saeki N, Yamaura A, Ozaki H, Nakazaki M (2004) [Nocardial brain abscess: surgery and postoperative antibiotic therapy]. No Shinkei Geka 32(5):457–462. (Japanese)
Inamasu J, Nakamura Y, Saito R (2003) Ring-enhanced mass in the brain of a woman with systemic lupus erythematosus and elevated serum CA19-9 level: brain abscess or metastatic tumor?—case report. Neurol Med Chir (Tokyo) 43(1):43–46
Raut A, Muzumdar D, Narlawar R, Nagar A, Ahmed N, Hira P (2003) Cerebral abscess caused by Cladosporium bantianum infection-case report. Neurol Med Chir (Tokyo) 43(8):413–415. https://doi.org/10.2176/nmc.43.413
AlHabib KF, Bryce EA (2003) Xylohypha bantiana multiple brain abscesses in a patient with systemic lupus erythematosus. Can J Infect Dis 14(2):119–120
Eckburg PB, Montoya JG, Vosti KL (2001) Brain abscess due to Listeria monocytogenes: five cases and a review of the literature. Medicine (Baltimore) 80:223–235
Takano A, Adachi H, Mizuno M, Kawamura K, Sobue G (1999) Direct gram staining of blood culture sample enabled the early diagnosis of brain abscess due to Listeria monocytogenes. Clin Neurol 39(11):1164–1167
Huang JL, Chou ML, Hung IJ, Hsieh KH (1996) Multiple cryptococcal brain abscesses in systemic lupus erythematosus. Br J Rheumatol 35(12):1334–1335
Escobar A, Del Brutto OH (1990) Multiple brain abscesses from isolated cerebral mucormycosis. J Neurol Neurosurg Psychiatry 53(5):431–433
Nishimoto Y, Ohno T, Kawabata Y (1980) An autopsy case of SLE with multiple brain abscess. J Wakayama Med Soc 31(4):383–393
Forno LS, Billingham ME (1972) Allescheria boydii infection of the brain. J Pathol 106(3):195–198
Tay SH, Mak A (2017) Diagnosing and attributing neuropsychiatric events to systemic lupus erythematosus: time to untie the Gordian knot? Rheumatology 56(suppl_1):i14-i23. https://doi.org/10.1093/rheumatology/kew338
Patel K, Clifford DB (2014) Bacterial brain abscess. Neurohospitalist 4(4):196–204. https://doi.org/10.1177/1941874414540684
Chowdhury FH, Haque MR, Sarkar MH, Chowdhury SM, Hossain Z, Ranjan S (2015) Brain abscess: surgical experiences of 162 cases. Neuroimmunol Neuroinflammation 2(3):153–161. https://doi.org/10.4103/2347-8659.160851
Fang H, Lan L, Qu Y, Zhang Q, Lv J (2018) Differences between central nervous system infection and neuropsychiatric systemic lupus erythematosus in patients with systemic lupus erythematosus. J Int Med Res 46(1):485–491. https://doi.org/10.1177/0300060517722695
Alvis Miranda H, Castellar-Leones SM, Elzain MA, Moscote-Salazar LR (2013) Brain abscess: Current management. J Neurosci Rural Pract 4(Suppl 1):S67–S81. https://doi.org/10.4103/0976-3147.116472
Acknowledgements
I would like to thank Enago for assistance in English language editing.
Author information
Authors and Affiliations
Contributions
FE designed, reviewed the literature, and wrote the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no competing interests.
Informed consent
An informed consent was obtained from the patient for publication.
Rights and permissions
About this article
Cite this article
Erbasan, F. Brain abscess caused by Micrococcus luteus in a patient with systemic lupus erythematosus: case-based review. Rheumatol Int 38, 2323–2328 (2018). https://doi.org/10.1007/s00296-018-4182-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-018-4182-2