Abstract
Background
Oral drug formulations have several advantages compared to intravenous formulation. Apart from patient convenience and favorable pharmacoeconomics, they offer the possibility of frequent drug administration at home. In this study, we present a new oral irinotecan formulation designed as an enteric coated immediate release tablet which in pre-clinical studies has shown good exposure with low variability.
Methods
A phase I, dose escalating study to assess safety, tolerability, pharmacokinetics and efficacy of an oral irinotecan formulation and to establish the maximum tolerated dose (MTD). Each treatment cycle was once-daily irinotecan for 14 days followed by 1 week rest.
Results
25 patients were included across four cohorts; 3 patients were included in cohort 1 (20 mg/m2), 7 patients were included in cohort 2 (30 mg/m2), 3 patients were included in cohort 3 (25 mg/m2) and 12 patients were included in cohort 4 (21 mg/m2). Median age was 67 years, 52% were performance status (PS) 0 while 48% were PS 1. Median number of prior therapies was 3 (range 1–6). MTD was established at 21 mg/m2. No responses were observed. Nine patients (36%) had stable disease (SD), lasting median 19 weeks (range 7–45 weeks). Among these five patients had previously received irinotecan. No grade 3/4 hematologic toxicities were reported. Totally six patients experienced grade 1/2 anemia, three patients had grade 1/2 leucopenia and 1 patient had grade 1 thrombocytopenia. Most common non-hematological grade 1 and 2 adverse events were nausea, fatigue, diarrhea, vomiting and cholinergic syndrome. Grade 3 toxicities included diarrhea, fatigue, nausea and vomiting, no grade 4 events were reported. PK data showed consistent daily exposures during treatment at days 1 and 14 and no drug accumulation. SN-38 interpatient variability was in the same range as after infusion.
Conclusions
Oral irinotecan was generally well tolerated; side effects were manageable and similar in type to those observed with intravenous irinotecan. Hematological toxicities were few and only grade 1/2. In this heavily pre-treated patient population, oral irinotecan demonstrated activity even among patients previously treated with irinotecan.
Similar content being viewed by others
Introduction
Irinotecan has been used in the treatment of various solid tumors for the past 2 decades and constitutes a corner stone in the treatment of metastatic colorectal, pancreatic and gastric cancers [1,2,3,4,5,6,7].
Originally introduced as an intravenous therapy, the search for an oral formulation has been ongoing almost since the drug was introduced [8]. Oral drug formulations are generally preferred by patients due to comfort and convenience, they often carry health economic benefits and, in the case of irinotecan, some studies indicate that oral irinotecan might be more effectively converted to the active metabolite SN-38 compared to intravenous administration [9, 10]. Further, oral administration allows for the concept of frequent dosing i.e., giving the chemotherapy at frequent time intervals in lower doses.
Irinotecan is a pro-drug which is enzymatically converted to the biologically active metabolite SN-38 [11]. Whereas irinotecan is water soluble, SN-38 is practically insoluble in water. Following metabolization in the liver SN-38 is converted to the water-soluble but inactive metabolite SN-38G. SN-38 is 100–1000 times more potent than irinotecan but the fraction of irinotecan actually converted to active SN-38 is small and exhibits a very large inter-patient variability. Due to severe side effects this problem is not readily solved by increasing the dose of irinotecan [12, 13]. During the past 20 years, several studies including various oral formulations of irinotecan have been conducted [8, 9, 14,15,16,17,18,19]. Oral bioavailability for both irinotecan and SN-38 has differed substantially among patients in the various studies [14,15,16,17,18]. The most common dose limiting toxicities have been diarrhea as well as nausea and vomiting. Despite fair efficacy results, none of the previously tested oral irinotecan formulations have gone into phase II trials mainly because of problems concerning poor solubility and a substantial interpatient variability in the oral bioavailability. In clinical trials, various oral formulations have been tested including solutions of i.v. irinotecan mixed with grape juice, powder filled capsules and semisolid matrix capsules, respectively. These formulations were all based on the water-soluble irinotecan hydrochloride, trihydrate salt [8,9,10, 18, 20]. More recently, preclinical studies have focused on improving solubility and increasing the bioavailability. In one study, SN-38 was encapsulated in lipid nano capsules and showed high permeability, however, only 8% of SN-38 was released after 3 days [21]. Another study investigated the conjugation of SN-38 to poly-amido amine dendrimers which resulted in increased trans-epithelial transport. Drug release was 10%, 20% and 56%, respectively, in simulated gastric, intestinal and liver environments [22]. Finally, pH-sensitive polymeric micelles of SN38 have been developed to improve permeability [23].
In the current study another approach has been used. The oral formulation in the present study is based on irinotecan in the free base form being solubilized in a hydrophobic lipid system. The system is formulated into an enteric coated tablet to avoid release in the stomach, as the stomach pH may influence the bio-absorption of irinotecan. The tablet releases the irinotecan immediately in the duodenum thereby avoiding protracted release. This is to ensure that the dosed irinotecan is eliminated before the next dose to avoid drug accumulation and to ensure high bio-absorption with low variability. In a pre-clinical repeat dose toxicity study, the irinotecan tablet was administered once daily for 14 days within a 3-week cycle and compared to irinotecan i.v. administration on day 1. The small daily doses of the irinotecan tablet resulted in less gastro-intestinal side effects compared to i.v. administration. Further, the white blood cell counts were less affected.
The aim of the present study was to evaluate a new oral tablet formulation of irinotecan in a clinical phase I study. The main purpose of the present study was to evaluate the safety and tolerability of the new oral formulation and to identify the maximal tolerated dose (MTD) in patients upon repeated oral dosing. Further, the pharmacokinetics including the interpatient variability were evaluated.
The study was designed as a standard dose escalating study with a subsequent extension trial in which the oral formulation was tested in combination with oral capecitabine. Only the first part of the study is described here.
Patients and methods
Study design
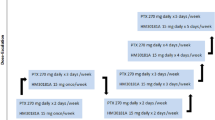
The study was a phase I, dose escalating, single center study to investigate the safety, tolerability and MTD. The investigational drug was designed and supplied by Oncoral Pharma ApS Denmark as an enteric coated immediate release tablet. The study drug was administered as tablets of either 7.5 mg or 10 mg. The total dose administered in mg was calculated as the body surface area (BSA) × dose in mg/m2. The number of tablets dispensed of each strength was selected to fit the total dose best possible.
One treatment cycle was 21 days and consisted of once-daily oral irinotecan for 14 days followed by 1 week rest, mimicking the most common used regimes with capecitabine.
The study was designed as a standard “3 + 3” design with an estimated 15–24 patients needed to establish the MTD. After reaching the MTD, an additional 12 patients were included to obtain sufficient data on safety and pharmacokinetics at the MTD level.
The starting dose was 20 mg/m2 daily followed by fixed increments of 10 mg/m2 with the opportunity to increase by only 5 mg/m2 in case of safety concerns. Progression to the next dose level was allowed if no dose limiting toxicities (DLT) were found in three patients. In case of a DLT occurrence, an additional three patients were to be included in the dose level and progression was only allowed if ≤ 1 patient experienced a DLT. If DLTs were found in ≥ 2 patients the study design was to be modified following safety data review. A safety board was established, and meetings were held prior to every dose escalation and on demand.
During the DLT period, i.e., the first two cycles, clinical safety assessment was performed at screening, on days 2, 5, 9, 14, 15, 22 in cycle one and once weekly in cycle two. Laboratory safety assessment was performed at screening, on days 5, 15 and 19 in cycle one and on days 8, 15 and 19 in cycle two.
DLT was defined as neutropenia or thrombocytopenia grade 4 or bleeding due to thrombocytopenia, any grade 3–4 adverse events thought to be treatment related, grade ≥ 3 diarrhea, vomiting or nausea despite optimal treatment, moderate to severe symptoms of early cholinergic syndrome or other adverse reactions leading to treatment delay for more than 2 weeks.
Pharmacokinetics of irinotecan, SN-38 and SN-38G were investigated on days 1 and 14 of the first cycle, 10 min pre-dosing and at 1 h, 1.5 h, 2 h, 2.5 h, 3 h, 3.5 h, 4 h, 5 h, 6 h, 8 h, 12 h and 24 h post dosing.
There were no restrictions on food intake during treatment except for days 1 and 14 of pharmacokinetic sampling where the patients were fasted from 10 p.m. in the evening and until 1 h post dosing.
Any impact of food was investigated at the dose level 21 mg/m2 (MTD) for six subjects taking the dose in fasted state on day 1 and in fed state on day 14, respectively.
Tumor response was evaluated according to RECIST 1.1 [24] with CT scans at day 36 (after 2 cycles of treatment) and hereafter every 6 weeks.
UGT1A1
SN-38 is primarily metabolized to the inactive SN-38 glucuronide by uridine diphosphate-glucuronyl transferase 1A1 (UGT1A1). UGT1A1 is an enzyme responsible for catalyzing the glucuronidation of various compounds, including steroid hormones, bilirubin, as well as xenobiotics, such as irinotecan. A polymorphic variation in the promoter of UGT1A1 leads to decreased expression of UGT1A1, resulting in reduced glucuronidation of SN-38, the active metabolite of irinotecan. Some studies have indicated that the risk of irinotecan toxicity is increased among persons with genetic variants associated with reduced UGT enzyme activity. Thus, patients with a (TA)7 repeat (UGT1A1*28) are at increased risk of developing grade 4 neutropenia or severe diarrhea [25]. The FDA-approved drug label for irinotecan states that when irinotecan is administered as a single agent, a reduction in the starting dose by at least one level of irinotecan hydrochloride injection should be considered for patients known to be homozygous for the UGT1A1*28 allele [26, 27]. As a consequence, we decided to study the polymorphisms of UGT1A1 in all patients entering the study.
A UGT1A1 Genotyping Kit (UGT-RT50, EntroGen) was used. This is a polymerase chain reaction (PCR)-based assay with allele-specific probes, which identify the most common irinotecan polymorphic variant. Briefly, genomic DNA was extracted from whole blood (n = 25) and used for the multiplexed amplification of the promoter region of the UGT1A1 gene with oligonucleotide primers that flanks the UGT1A1*1/*28 SNP. The variants were detected using fluorescent dyes [FAM labeled probes detect UGT1A1*1 (wild type), VIC labeled probes detect UGT1A1*28 (mutant)]. Samples were classified as: homozygote (UGT1A1*1 or UGT1A1*28) and heterozygote (UGT1A1*1 and UGT1A1*28). Amplification was performed on an Applied Biosystems 7500 instrument.
Study population
Patients with metastatic or unresectable solid tumors for whom no standard treatment options existed were eligible for inclusion. Patients were required to be in performance status 0–1 according to ECOG [28], have a life expectancy of ≥ 3 month and adequate organ and bone marrow function. Furthermore, patients with chronic enteropathy, bowel obstruction or sub-obstruction, prior history of malabsorption or symptomatic brain metastases were excluded.
Study objectives
The primary objectives were to determine the safety, tolerability and MTD of oral irinotecan. Secondary objectives included pharmacokinetics and tumor response.
Statistical analysis
No formal statistical analyses were performed on safety or efficacy data. Descriptive statistics were used for patient demographics, safety and efficacy data.
Pharmacokinetic analysis
Concentrations of irinotecan, SN-38 and SN-38G in stabilized human plasma samples were measured using LC-MS/MS with protein precipitation extraction. The corrected lower limit of quantification (LLOQ) for irinotecan and SN-38 in human plasma was 0.110 ng/mL and 0.550 ng/mL for SN-38G. Values below were reported as below limit of quantification (BLQ). The extent of conversion of irinotecan to SN-38 was calculated as the metabolic ratio being AUCSN-38/AUCIri. The extent of glucuronidation of SN-38 to SN-38G was calculated as the glucuronidation ratio being AUCSN-38G/AUCSN-38.
Pharmacokinetic non-compartmental analysis was performed using WinNonlin v6.3 on irinotecan and its metabolites SN-38 and SN-38G. A value of 0 was used for all human plasma concentrations recorded as BLQ prior to tmax and concentrations recorded as BLQ after tmax were set to missing. Estimation of t½ was subject to a minimum of 3 data points on the fitted line of regression, a measured portion of the line of regression equivalent to at least 1.5 times the half-life and a coefficient of determination (R2) of at least 0.80.
Ethics
The study was performed in accordance with the Declaration of Helsinki, ICH-Good Clinical Practice and approved by the Regional Ethics Committee (H-15000878) of Denmark. All included patients provided written, informed consent. The study was initiated by the principal investigator at Herlev and Gentofte Hospital, Department of Oncology and partly sponsored by grants from the Innovation Foundation and the Danish Cancer Society and registered at EudraCT (2014-005584-32) and at ClinicalTrials.Gov (NCT03295084).
Results
Patient characteristics
From July 2015 to September 2017, 25 patients were included across 4 treatment cohorts; 3 patients were included in cohort 1 (20 mg/m2), 7 patients were included in cohort 2 (30 mg/m2), 3 patients were included in cohort 3 (25 mg/m2) and 12 patients were included in cohort 4 (21 mg/m2). According to the protocol, one patient in cohort 2 was replaced as this patient was withdrawn due to cancer-related complaints after only 4 days of dosing with irinotecan.
Included patients were median 67 years old (range 51–82), 52% were performance status (PS) 0 while 48% were PS 1. Among the included patients, six had a diagnosis of cholangiocarcinoma, five had a diagnosis of colon cancer, four had pancreas and prostate cancer, respectively, and one each had cervical cancer, NSCLC, ovarian cancer, rectal cancer, SCLC and mesothelioma. Median number of prior therapies was 3 ranging from 1 to 6.
Patients’ characteristics are summarized in Table 1.
Dose escalation and dose limiting toxicities
In cohort 1, no DLTs were observed. At progression to next dose level (30 mg/m2), one patient experienced diarrhea grade 3 and thus three more patients were included. As one more patient experienced grade 3 diarrhea, the MTD was exceeded and the dose level was lowered to 25 mg/m2. Three patients were included; one grade 3 diarrhea accompanied with dehydration grade 3 was reported as well as elevated alkaline phosphatase grade 3.
Following a safety board meeting, the dose was lowered to 21 mg/m2 and this dose was accepted as MTD.
The median treatment duration in cohort 1–4 was 70 days (range 35–97), 9 days (range 4–35), 11 days (range 5–119) and 35.5 days (range 2–228), respectively. Total doses of irinotecan were 1640 mg, 450 mg, 440 mg and 1100 mg, respectively, in cohorts 1, 2, 3 and 4. The shorter treatment periods in cohorts 2 and 3 are reflected in the lower total doses. Among the 15 patients treated in either cohort 1 or 4 at the MTD, the median dose of irinotecan was 1120 mg (range 71–8190 mg).
Pharmacokinetics
The pharmacokinetic parameters of Irinotecan, SN-38 and SN-38G were determined in totally 25 patients on day 1 and day 14 of the first cycle. As the three patients in cohort 1 (20 mg/m2) were dosed 20.9 mg/m2 and within the range of dosing for cohort 4 (21 mg/m2) the patients of cohorts 1 and 4 were merged into a common cohort 4, i.e., dose level 21 mg/m2 for the pharmacokinetic evaluation.
The pharmacokinetic data for irinotecan, SN-38 and SN-38G on both days are provided in Table 2 and plasma profiles of irinotecan, SN-38 and SN-38G on day 1 are provided in Fig. 1.
At the MTD level (21 mg/m2 dose level), mean Cmax levels of 19.2 ng/mL and 15.2 ng/mL and mean AUC0–24 levels of 135 h ng/mL and 133 h ng/mL, respectively, were found on day 1 and day 14 for irinotecan. Median time to observe maximum concentration (tmax) for irinotecan was 3 h on both days. For SN-38 mean Cmax levels of 2.67 ng/mL and 2.19 ng/mL and mean AUC0–24 levels of 22.5 and 21.6 ng/mL were found with a median tmax of 4 h on both day 1 and day 14. The metabolic ratios of SN-38/irinotecan at MTD were consistent after 14 days of repeat dosing with AUC0–24 ratios of 0.175 (17.5%) and 0.163 (16.3%), and Cmax ratios of 0.142 and 0.145 on day 1 and day 14, respectively. The metabolic AUC0–24 ratios of SN-38G/SN-38 were 6.38 and 6.78 and Cmax ratios were 5.45 and 5.91 on day 1 and day 14, respectively.
The geometric means day 14 over day 1 exposure ratio of irinotecan for Cmax and AUC0–24 were 0.85 and 1.08, respectively, and 0.87 and 1.00 for SN-38. The geometric mean trough concentration C24 prior to dosing at day 14 was 1.95 ng/mL for irinotecan and 0.631 ng/mL for SN-38. Both the geometric mean day 14 over day 1 exposure ratio and the C24 level indicate no drug accumulation of relevance for irinotecan and SN-38.
The inter-patient coefficient of variation (CV%) in SN-38 exposure (based on AUC0–t) was 63.3% on day 1 and 42.6% day 14 for SN-38.
The geometric mean AUC0–t obtained was 159 h ng/mL and 124 h ng/mL in fasted and fed state, respectively. The fed/fasted ratio of the geometric mean AUC0–24 for the six patients taking the irinotecan tablet in fasted state at MTD on day 1 and in fed state on day 14 was 0.776 for irinotecan and 0.791 for SN-38 with a range from 0.145 to 2.17 for irinotecan and 0.218 to 1.58 for SN-38 as some patients experienced somewhat higher AUC0–24 on day 1 in fasted state and others on day 14 after a meal.
Increasing the doses to 25 mg/m2 and to 30 mg/m2 resulted in increases in both geometric mean Cmax and AUC0–t of irinotecan. For SN-38 the exposure increased with increasing dose in a manner that was greater than dose proportional between the 21 and 25 mg/m2 dose levels, and proportional between the 25 and 30 mg/m2 doses. In general, there was not enough data at day 14 for the dose levels 25 mg/m2 and 30 mg/m2 to draw any firm pharmacokinetic conclusions.
UGT1A1
In total, 25 blood samples from patients included were analyzed. We did perform all analyses in duplicate to ensure consistent results. The detected variants found were classified as homozygote UGT1A1*1; 13 (52%), homozygote UGT1A1*28; 2 (8%) and heterozygote 10 (40%). Of two patients homozygote for UGT1A1*28, one patient experienced a grade 3 diarrhea and withdrew the study due to toxicity. The following CT scan showed stable disease (SD). The other patient terminated the study early due to cancer-related complaints and only received oral irinotecan for 4 days. Among the remaining patients with grade 3 diarrhea one was heterozygote for UGT1A1*28 and three were homozygote for UGT1A1*1. Additionally, patients with SD were found among both UGT1A1*1 homozygote and UGT1A1*28 heterozygote.
Safety
Only grade 1 and 2 hematologic toxicities were reported. Totally six patients across all cohorts experienced grade 1/2 anemia, three patients had grade 1/2 leucopenia and only one patient had grade 1 thrombocytopenia (Table 3).
Most common non-hematological grade 1 and 2 adverse events were nausea, fatigue, diarrhea, vomiting and cholinergic syndrome (Table 4). Across cohorts 1–3 DLTs were observed in four patients and included diarrhea (three patients) and increased alkaline phosphatase (one patient). In cohort 4, totally four patients experienced grade 3 AEs probably or possible related, these included diarrhea, nausea, vomiting, spleen infarction, cataract, increased blood bilirubin, fatigue and deterioration of general condition (Table 4). Totally 13 patients (52%) discontinued the study due to unacceptable side effects. In cohort 4, five patients (42%) discontinued due to toxicities.
Efficacy
No complete or partial responses were observed. Nine patients (36%) had SD at first response evaluation, lasting median 19 weeks (range 7–45 weeks). Among patients with SD three had a diagnosis of colon cancer, three had cholangiocarcinoma and one each had SCLC, mesothelioma and ovarian cancer. Among patients with SD, five had previously received intravenous irinotecan.
Totally eight patients were non-evaluable as they discontinued the study due to toxicities and no CT scan was performed at the end of treatment.
Discussion
Oral drug formulations possess several advantages compared to intravenous formulations. Apart from patient convenience and favorable pharmacoeconomics, they offer the possibility of out-hospital drug administration at frequent intervals at lower doses. As no oral irinotecan formulations have been approved, clinical data on frequent dosing with irinotecan are sparse. However, data from the few published studies seem to indicate that frequent dosing is well tolerated and possibly more efficacious than more protracted administration schedules [29,30,31].
Several attempts have been made to develop a safe and efficient oral administration of irinotecan using a dosing regimen of either 5 or 14 days of treatment within 3 weeks treatment cycles [8,9,10, 18, 20].
These studies indicate that it is most likely the cumulative dose within a treatment cycle that defines DLT and thereby the MTD. Treatment once daily for 5 days within a 3-week cycle resulted in MTDs in the range 50–80 mg/m2 of irinotecan, hydrochloride, and trihydrate, whereas treatment once daily for 14 days resulted in MTDs in the range of 30–40 mg/m2 of irinotecan, hydrochloride, and trihydrate. In the present study, a MTD of 21 mg/m2 irinotecan (free base) corresponding to 24 mg/m2 of irinotecan, hydrochloride, trihydrate was administered daily providing a cumulative dose of approximately 340 mg/m2 within each 3-week treatment cycle. This cumulative dose corresponds well with the commonly used dose 340 mg/m2 provided as i.v. administration every 3 weeks [27].
The pharmacokinetic data of the present study showed that irinotecan was rapidly and well absorbed and converted to its active metabolite SN-38 upon oral administration. Oral irinotecan was more effectively converted to SN-38 compared to intravenous administration as conversion was approximately six- to sevenfold higher following oral administration. The metabolic ratio of SN38/irinotecan was in the range of 16.3–16.6% compared to 2.3% following i.v. administration. The gastro-intestinal tract contains high levels of the carboxylesterase enzyme most likely responsible for the additional conversion to SN-38. Plasma peaks of irinotecan and SN-38 occurred after approximately 3 h. The absorbed irinotecan was eliminated within 24 h with no evidence of accumulation upon repeated dosing. Thus, the current treatment regimen appeared to be safe in relation to drug accumulation and provided consistent daily exposures during treatment from day 1 to day 14 within each cycle.
The cumulative exposure of SN-38 within a 3-week cycle was in the same range as that obtained following a single i.v. administration of 340 mg/m2 (approximately 315 ng/mL versus 474 ng/mL) [27].
The inter-patient coefficient of variation in SN-38 exposure (AUC0–24) after i.v. dosing has been reported to be approximately 47–51% and is most likely linked to the complex pharmacokinetics of the drug. The CV% for the active metabolite SN-38 after oral administration of the irinotecan tablet was 43–63% which is comparable to that of i.v. treatment [26].
The impact of food on oral irinotecan was investigated in six patients. In accordance with previously published data, no significant effect on absorption of irinotecan was found following food intake [19].
Grades 3 and 4 late diarrhea appear in 16–22% of patients after i.v. administration of irinotecan [32]. SN-38G is considered responsible for the delayed diarrhea through biliary excretion and increased SN-38 exposure in the gut. Totally five patients experienced grade 3 diarrhea after oral dosing in the present study, respectively, three patients after exposure to 30 mg/m2, one patient after exposure to 25 mg/m2 and one patient at MTD after oral dosing in the present study. However, no correlation was found between grade 3 diarrhea and the levels of SN-38G or the SN-38G/SN-38 ratios found in the patients.
UGT1A1 plays a role in the glucuronidation of SN-38 and it has been speculated whether a screening for UGT1A1*28 polymorphism could identify patients with lower SN-38 glucuronidation rates and a greater susceptibility to irinotecan induced diarrhea [33]. Although a limited number of patients were included in this study no correlation between UGT1A1 variants and toxicity or response was identified. This agrees with findings from another study of oral irinotecan where no correlation was found between irinotecan associated toxicity and the UGT1A1*28 genotype [19].
Non-hematological side effects such as late diarrhea, nausea and vomiting are common following i.v. administration. Grades 3 and 4 diarrhea were reported in 30.6% of patients, grades 3 and 4 nausea in 16.8% of patients and grades 3 and 4 vomiting in 12.5% of patients after i.v. administration [19]. The non-hematological side effects following administration of the irinotecan tablet were comparable to those observed following i.v. formulations but less severe [4, 6, 7]. In our study, most non-hematological side effects were of grade 1 or 2. Only one subject (8.3%) experienced grade 3 diarrhea, vomiting or nausea, respectively at the MTD level.
Myelosuppression is a common toxicity following i.v. administration of irinotecan and possesses a serious threat to patients on chemotherapy. Thus, while hematologic side effects grades 3 and 4 are reported following i.v. administration of irinotecan in 10–31.4% of patients participating in clinical trials [27, 34,35,36,37], no grade 3 or 4 hematologic toxicities were reported in the present study, indicating that the oral administration may have a favorable hematologic profile compared to intravenous administration. This is most likely due to the administration of small daily oral doses in contrast to a large dose administered intravenously weekly or every third week [4, 6, 7].
No objective responses were seen in this heavily pretreated cohort, however, nine (36%) patients did obtain a clinical benefit with SD lasting median 19 weeks. Among these, five patients (56%) had previously been treated with intravenous irinotecan.
In conclusion, we found the oral formulation to be safe and efficacious with less hematologic side effects. Our tablet formulation is currently investigated in combination with capecitabine.
References
Van Cutsem E, Cervantes A, Nordlinger B, Arnold D, Group EGW (2014) Metastatic colorectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 25(Suppl 3):iii1–i9. https://doi.org/10.1093/annonc/mdu260
de Man FM, Goey AKL, van Schaik RHN, Mathijssen RHJ, Bins S (2018) Individualization of irinotecan treatment: a review of pharmacokinetics, pharmacodynamics, and pharmacogenetics. Clin Pharmacokinet. https://doi.org/10.1007/s40262-018-0644-7
Wagener DJ, Verdonk HE, Dirix LY, Catimel G, Siegenthaler P, Buitenhuis M, Mathieu-Boue A, Verweij J (1995) Phase II trial of CPT-11 in patients with advanced pancreatic cancer, an EORTC early clinical trials group study. Ann Oncol 6(2):129–132
Ueno H, Okusaka T, Funakoshi A, Ishii H, Yamao K, Ishikawa O, Ohkawa S, Saitoh S (2007) A phase II study of weekly irinotecan as first-line therapy for patients with metastatic pancreatic cancer. Cancer Chemother Pharmacol 59(4):447–454. https://doi.org/10.1007/s00280-006-0283-9
Conroy T, Desseigne F, Ychou M, Bouche O, Guimbaud R, Becouarn Y, Adenis A, Raoul JL, Gourgou-Bourgade S, de la Fouchardiere C, Bennouna J, Bachet JB, Khemissa-Akouz F, Pere-Verge D, Delbaldo C, Assenat E, Chauffert B, Michel P, Montoto-Grillot C, Ducreux M, Groupe Tumeurs Digestives of Unicancer and the PRODIGE Intergroup (2011) FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med 364(19):1817–1825. https://doi.org/10.1056/NEJMoa1011923
Thuss-Patience PC, Kretzschmar A, Bichev D, Deist T, Hinke A, Breithaupt K, Dogan Y, Gebauer B, Schumacher G, Reichardt P (2011) Survival advantage for irinotecan versus best supportive care as second-line chemotherapy in gastric cancer—a randomised phase III study of the Arbeitsgemeinschaft Internistische Onkologie (AIO). Eur J Cancer 47(15):2306–2314. https://doi.org/10.1016/j.ejca.2011.06.002
Roy AC, Park SR, Cunningham D, Kang YK, Chao Y, Chen LT, Rees C, Lim HY, Tabernero J, Ramos FJ, Kujundzic M, Cardic MB, Yeh CG, de Gramont A (2013) A randomized phase II study of PEP02 (MM-398), irinotecan or docetaxel as a second-line therapy in patients with locally advanced or metastatic gastric or gastro-oesophageal junction adenocarcinoma. Ann Oncol 24(6):1567–1573. https://doi.org/10.1093/annonc/mdt002
Drengler RL, Kuhn JG, Schaaf LJ, Rodriguez GI, Villalona-Calero MA, Hammond LA, Stephenson JA Jr, Hodges S, Kraynak MA, Staton BA, Elfring GL, Locker PK, Miller LL, Von Hoff DD, Rothenberg ML (1999) Phase I and pharmacokinetic trial of oral irinotecan administered daily for 5 days every 3 weeks in patients with solid tumors. J Clin Oncol 17(2):685–696
Pitot HC, Adjei AA, Reid JM, Sloan JA, Atherton PJ, Rubin J, Alberts SR, Duncan BA, Denis L, Schaaf LJ, Yin D, Sharma A, McGovren P, Miller LL, Erlichman C (2006) A phase I and pharmacokinetic study of a powder-filled capsule formulation of oral irinotecan (CPT-11) given daily for 5 days every 3 weeks in patients with advanced solid tumors. Cancer Chemother Pharmacol 58(2):165–172. https://doi.org/10.1007/s00280-005-0138-9
Rothenberg ML, Kuhn JG, Schaaf LJ, Drengler RL, Eckhardt SG, Villalona-Calero MA, Hammond L, Miller LL, Petit RG, Rowinsky EK, Von Hoff DD (1998) Alternative dosing schedules for irinotecan. Oncology (Williston Park) 12(8 Suppl 6):68–71
Moukharskaya J, Verschraegen C (2012) Topoisomerase 1 inhibitors and cancer therapy. Hematol Oncol Clin N Am 26(3):507–525. https://doi.org/10.1016/j.hoc.2012.03.002 vii.
Bala V, Rao S, Boyd BJ, Prestidge CA (2013) Prodrug and nanomedicine approaches for the delivery of the camptothecin analogue SN38. J Control Release 172(1):48–61. https://doi.org/10.1016/j.jconrel.2013.07.022
Bala V, Rao S, Li P, Wang S, Prestidge CA (2016) Lipophilic prodrugs of SN38: synthesis and in vitro characterization toward oral chemotherapy. Mol Pharm 13(1):287–294. https://doi.org/10.1021/acs.molpharmaceut.5b00785
Berlin J, Benson AB, Rubin EH et al (2003) Phase I safety, pharmacokinetic and bioavailability study of a semi-solid matrix formulations of oral irinotecan in patients with advanced solid tumors. Proc Am Soc Clin Oncol 22:130 (Abstract 521)
Dumez H, Awada A, Piccart M, Assadourian S, Semiond D, Guetens G, de Boeck G, Maes RA, de Bruijn EA, van Oosterom A (2006) A phase I dose-finding clinical pharmacokinetic study of an oral formulation of irinotecan (CPT-11) administered for 5 days every 3 weeks in patients with advanced solid tumours. Ann Oncol 17(7):1158–1165. https://doi.org/10.1093/annonc/mdl071
Goff LW, Benson AB III, LoRusso PM, Tan AR, Berlin JD, Denis LJ, Benner RJ, Yin D, Rothenberg ML (2012) Phase I study of oral irinotecan as a single-agent and given sequentially with capecitabine. Investig New Drugs 30(1):290–298. https://doi.org/10.1007/s10637-010-9528-x
Kuppens IE, Dansin E, Boot H, Feger C, Assadourian S, Bonneterre ME, Beijnen JH, Schellens JH, Bonneterre J (2006) Dose-finding phase I clinical and pharmacokinetic study of orally administered irinotecan in patients with advanced solid tumors. Clin Cancer Res 12(12):3774–3781. https://doi.org/10.1158/1078-0432.CCR-05-2368
Schoemaker NE, Kuppens IE, Huinink WW, Lefebvre P, Beijnen JH, Assadourian S, Sanderink GJ, Schellens JH (2005) Phase I study of an oral formulation of irinotecan administered daily for 14 days every 3 weeks in patients with advanced solid tumours. Cancer Chemother Pharmacol 55(3):263–270. https://doi.org/10.1007/s00280-004-0874-2
Soepenberg O, Dumez H, Verweij J, de Jong FA, de Jonge MJ, Thomas J, Eskens FA, van Schaik RH, Selleslach J, Ter Steeg J, Lefebvre P, Assadourian S, Sanderink GJ, Sparreboom A, van Oosterom AT (2005) Phase I pharmacokinetic, food effect, and pharmacogenetic study of oral irinotecan given as semisolid matrix capsules in patients with solid tumors. Clin Cancer Res 11(4):1504–1511. https://doi.org/10.1158/1078-0432.CCR-04-1758
Lien K, Georgsdottir S, Sivanathan L, Chan K, Emmenegger U (2013) Low-dose metronomic chemotherapy: a systematic literature analysis. Eur J Cancer 49(16):3387–3395. https://doi.org/10.1016/j.ejca.2013.06.038
Roger E, Lagarce F, Benoit JP (2011) Development and characterization of a novel lipid nanocapsule formulation of Sn38 for oral administration. Eur J Pharm Biopharm 79(1):181–188. https://doi.org/10.1016/j.ejpb.2011.01.021
Goldberg DS, Vijayalakshmi N, Swaan PW, Ghandehari H (2011) G3.5 PAMAM dendrimers enhance transepithelial transport of SN38 while minimizing gastrointestinal toxicity. J Control Release 150(3):318–325. https://doi.org/10.1016/j.jconrel.2010.11.022
Le Garrec D, Benquet C, Lessard D, Parisien M, Palusova D, Kujawa P, Baille W, Nasser-Eddine M, Smith D (2009) Antitumor activities of a novel oral formulation of SN38. Mol Cancer Ther 8(Suppl12):C218. https://doi.org/10.1158/1535-7163. TARG-09-C218
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45(2):228–247. https://doi.org/10.1016/j.ejca.2008.10.026
Schulz C, Boeck S, Heinemann V, Stemmler HJ (2009) UGT1A1 genotyping: a predictor of irinotecan-associated side effects and drug efficacy? Anticancer Drugs 20(10):867–879. https://doi.org/10.1097/CAD.0b013e328330c7d2
FDA (2009) FDA highlight of prescribing information for Camptosar injection, intravenous infusion. https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/020571s031s032s033s036s037lbl.pdf. Accessed 8 Nov 2018
Inc PC (2018) Product Monograph for irinotecan hydrochloride trihydrate for injection 20 mg/mL. https://www.pfizerca/sites/g/files/g10045006/f/201803/20181313_Irinotecan_PM_E_212772.pdf
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5(6):649–655
Moiseyenko V, Chubenko V, Protsenko S (2010) Phase II study of metronomic chemotherapy with irinotecan in patients with refractory metastatic colorectal cancer. J Clin Oncol. https://doi.org/10.1200/jco.2010.28.15_suppl.e14109
Perez EA, Hillman DW, Mailliard JA, Ingle JN, Ryan JM, Fitch TR, Rowland KM, Kardinal CG, Krook JE, Kugler JW, Dakhil SR (2004) Randomized phase II study of two irinotecan schedules for patients with metastatic breast cancer refractory to an anthracycline, a taxane, or both. J Clin Oncol 22(14):2849–2855. https://doi.org/10.1200/JCO.2004.10.047
Allegrini G, Falcone A, Fioravanti A, Barletta MT, Orlandi P, Loupakis F, Cerri E, Masi G, Di Paolo A, Kerbel RS, Danesi R, Del Tacca M, Bocci G (2008) A pharmacokinetic and pharmacodynamic study on metronomic irinotecan in metastatic colorectal cancer patients. Br J Cancer 98(8):1312–1319. https://doi.org/10.1038/sj.bjc.6604311
Stein A, Voigt W, Jordan K (2010) Chemotherapy-induced diarrhea: pathophysiology, frequency and guideline-based management. Ther Adv Med Oncol 2(1):51–63. https://doi.org/10.1177/1758834009355164
Iyer L, Das S, Janisch L, Wen M, Ramirez J, Karrison T, Fleming GF, Vokes EE, Schilsky RL, Ratain MJ (2002) UGT1A1*28 polymorphism as a determinant of irinotecan disposition and toxicity. Pharmacogenomics J 2(1):43–47
Rothenberg ML, Eckardt JR, Kuhn JG, Burris HA III, Nelson J, Hilsenbeck SG, Rodriguez GI, Thurman AM, Smith LS, Eckhardt SG, Weiss GR, Elfring GL, Rinaldi DA, Schaaf LJ, Von Hoff DD (1996) Phase II trial of irinotecan in patients with progressive or rapidly recurrent colorectal cancer. J Clin Oncol 14(4):1128–1135. https://doi.org/10.1200/JCO.1996.14.4.1128
Verschraegen CF, Levy T, Kudelka AP, Llerena E, Ende K, Freedman RS, Edwards CL, Hord M, Steger M, Kaplan AL, Kieback D, Fishman A, Kavanagh JJ (1997) Phase II study of irinotecan in prior chemotherapy-treated squamous cell carcinoma of the cervix. J Clin Oncol 15(2):625–631. https://doi.org/10.1200/JCO.1997.15.2.625
Sanchez R, Esteban E, Palacio I, Fernandez Y, Muniz I, Vieitez JM, Fra J, Blay P, Villanueva N, Una E, Mareque B, Estrada E, Buesa JM, Lacave AJ (2003) Activity of weekly irinotecan (CPT-11) in patients with advanced non-small cell lung cancer pretreated with platinum and taxanes. Investig New Drugs 21(4):459–463
Pitot HC, Wender DB, O’Connell MJ, Schroeder G, Goldberg RM, Rubin J, Mailliard JA, Knost JA, Ghosh C, Kirschling RJ, Levitt R, Windschitl HE (1997) Phase II trial of irinotecan in patients with metastatic colorectal carcinoma. J Clin Oncol 15(8):2910–2919. https://doi.org/10.1200/JCO.1997.15.8.2910
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The study was initiated by the primary investigator at the Department of Oncology, Herlev and Gentofte Hospital. All study medication was manufactured and provided by Oncoral Pharma ApS. The study was partly funded by grants from Innovationsfonden (Innovation Fund Denmark) and the Danish Cancer Society. Oncoral Pharma is partly owned by Peter G Nielsen and Ann Fullerton. All other authors declare no conflict of interests.
Ethical standards
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kümler, I., Sørensen, P.G., Palshof, J. et al. Oral administration of irinotecan in patients with solid tumors: an open-label, phase I, dose escalating study evaluating safety, tolerability and pharmacokinetics. Cancer Chemother Pharmacol 83, 169–178 (2019). https://doi.org/10.1007/s00280-018-3720-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-018-3720-7