Abstract
Purpose
Augmented reality (AR) is an innovative approach that could assist percutaneous procedures; by directly seeing “through” a phantom, targeting a lesion might be more intuitive than using ultrasound (US). The objective of this study was to compare the performance of experienced interventional radiologists and operators untrained in soft tissue lesion puncture using AR guidance and standard US guidance.
Material and Methods
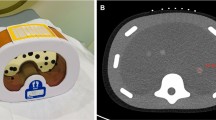
Three trained interventional radiologists with 5–10 years of experience and three untrained operators performed punctures of five targets in an abdominal phantom, with US guidance and AR guidance. Correct targeting, accuracy (defined as the Euclidean distance between the tip and the center of the target), planning time, and puncture time were documented.
Results
Accuracy was higher for the trained group than the untrained group using US guidance (1 mm versus 4 mm, p = 0.001), but not when using AR guidance (4 mm vs. 4 mm, p = 0.76). All operators combined, no significant difference was found concerning accuracy between US and AR guidance (2 mm vs. 4 mm, p = 0.09), but planning time and puncture time were significantly shorter using AR (respectively, 15.1 s vs. 74 s, p < 0.001; 16.1 s vs. 59 s; p < 0.001).
Conclusion
Untrained and trained operators obtained comparable accuracy in percutaneous punctures when using AR guidance whereas US performance was better in the experienced group. All operators together, accuracy was similar between US and AR guidance, but shorter planning time, puncture time were found for AR guidance.
Graphical Abstract



Similar content being viewed by others
Abbreviations
- AR:
-
Augmented reality
- CT:
-
Computed tomography
- US:
-
Ultrasound
References
Alexander LF, McComb BL, Bowman AW, Bonnett SL, Ghazanfari SM, Caserta MP. Ultrasound simulation training for radiology residents—curriculum design and implementation. J Ultrasound Med. 2023;42:777–90. https://doi.org/10.1002/jum.16098.
Fatima H, Mahmood F, Mufarrih SH, Mitchell JD, Wong V, Amir R, et al. Preclinical proficiency-based model of ultrasound training. Anesth Analg. 2022;134:178–87. https://doi.org/10.1213/ANE.0000000000005510.
Rankin JH, Elkhunovich MA, Rangarajan V, Chilstrom M, Mailhot T. Learning curves for ultrasound assessment of lumbar puncture insertion sites: when is competency established? J Emerg Med. 2016;51:55–62. https://doi.org/10.1016/j.jemermed.2016.03.025.
Härle P, Bester J, Hillebrand M, Hartung W. Ultrasound-guided puncture: an inexpensive and effective learning model. Z Rheumatol. 2011;70:525–9. https://doi.org/10.1007/s00393-011-0839-x.
Liu Y, Glass NL, Glover CD, Power RW, Watcha MF. Comparison of the development of performance skills in ultrasound-guided regional anesthesia simulations with different phantom models. Simul Healthc. 2013;8:368–75. https://doi.org/10.1097/SIH.0b013e318299dae2.
Dabadie A, Soussan J, Mancini J, Vidal V, Bartoli JM, Gorincour G, et al. Development and initial evaluation of a training program for peripherally inserted central catheter (PICC) placement for radiology residents and technicians. Diagn Interv Imaging. 2016;97:877–82. https://doi.org/10.1016/j.diii.2015.11.014.
De Fiori E, Rampinelli C, Turco F, Bonello L, Bellomi M. Role of operator experience in ultrasound-guided fine-needle aspiration biopsy of the thyroid. Radiol Med. 2010;115:612–8. https://doi.org/10.1007/s11547-010-0528-x.
Zammit C, Calleja-Agius J, Azzopardi E. Augmented reality for teaching anatomy. Clin Anat. 2022;35:824–7. https://doi.org/10.1002/ca.23920.
Barral M, Razakamanantsoa L, Cornelis FH. How to further train medical students in Interventional radiology? Diagn Interv Imaging. 2021;102:9–10. https://doi.org/10.1016/j.diii.2020.11.014.
Shuhaiber JH. Augmented reality in surgery. Arch Surg. 2004;139:170–4. https://doi.org/10.1001/archsurg.139.2.170.
Verhey JT, Haglin JM, Verhey EM, Hartigan DE. Virtual, augmented, and mixed reality applications in orthopedic surgery. Int J Med Robot. 2020;16:e2067. https://doi.org/10.1002/rcs.2067.
Park BJ, Hunt SJ, Martin C, Nadolski GJ, Wood BJ, Gade TP. Augmented and Mixed reality: technologies for enhancing the future of IR. J Vasc Interv Radiol. 2020;31:1074–82. https://doi.org/10.1016/j.jvir.2019.09.020.
Sparwasser P, Haack M, Epple S, Frey L, Zeymer S, Dotzauer R, et al. Smartglass augmented reality-assisted targeted prostate biopsy using cognitive point-of-care fusion technology. Int J Med Robot. 2022;18:e2366. https://doi.org/10.1002/rcs.2366.
Pfefferle M, Shahub S, Shahedi M, Gahan J, Johnson B, Le P, et al. Renal biopsy under augmented reality guidance. Proc SPIE Int Soc Opt Eng. 2020;11315:113152W. https://doi.org/10.1117/12.2550593.
Costa N, Ferreira L, de Araújo ARVF, Oliveira B, Torres HR, Morais P, et al. Augmented reality-assisted ultrasound breast biopsy. Sensors (Basel). 2023;23:1838. https://doi.org/10.3390/s23041838.
Fritz J, Paweena U, Ungi T, Flammang AJ, McCarthy EF, Fichtinger G, et al. Augmented reality visualization using image overlay technology for MR-guided interventions: cadaveric bone biopsy at 1.5 T. Invest Radiol. 2013;48:464–70. https://doi.org/10.1097/RLI.0b013e31827b9f86.
Gadodia G, Yanof J, Hanlon A, Bustos S, Weunski C, West K, et al. Early clinical feasibility evaluation of an augmented reality platform for guidance and navigation during percutaneous tumor ablation. J Vasc Interv Radiol. 2022;33:333–8. https://doi.org/10.1016/j.jvir.2021.11.014.
Nicolau SA, Pennec X, Soler L, Buy X, Gangi A, Ayache N, et al. An augmented reality system for liver thermal ablation: design and evaluation on clinical cases. Med Image Anal. 2009;13:494–506. https://doi.org/10.1016/j.media.2009.02.003.
Solbiati M, Ierace T, Muglia R, Pedicini V, Iezzi R, Passera KM, et al. Thermal ablation of liver tumors guided by augmented reality: an initial clinical experience. Cancers (Basel). 2022;14:1312. https://doi.org/10.3390/cancers14051312.
Yang J, Zhu J, Sze DY, Cui L, Li X, Bai Y, et al. Feasibility of augmented reality-guided transjugular intrahepatic portosystemic shunt. J Vasc Interv Radiol. 2020;31:2098–103. https://doi.org/10.1016/j.jvir.2020.07.025.
Li M, Seifabadi R, Long D, De Ruiter Q, Varble N, Hecht R, et al. Smartphone- versus smartglasses-based augmented reality (AR) for percutaneous needle interventions: system accuracy and feasibility study. Int J Comput Assist Radiol Surg. 2020;15:1921–30. https://doi.org/10.1007/s11548-020-02235-7.
Long DJ, Li M, De Ruiter QMB, Hecht R, Li X, Varble N, et al. Comparison of smartphone augmented reality, smartglasses augmented reality, and 3D CBCT-guided fluoroscopy navigation for percutaneous needle insertion: a phantom study. Cardiovasc Intervent Radiol. 2021;44:774–81. https://doi.org/10.1007/s00270-020-02760-7.
Fedorov A, Beichel R, Kalpathy-Cramer J, Finet J, Fillion-Robin J-C, Pujol S, et al. 3D Slicer as an image computing platform for the quantitative imaging network. Magn Reson Imaging. 2012;30:1323–41. https://doi.org/10.1016/j.mri.2012.05.001.
Barat M, Jannot A-S, Dohan A, Soyer P. How to report and compare quantitative variables in a radiology article. Diagn Interv Imaging. 2022;103:571–3. https://doi.org/10.1016/j.diii.2022.09.007.
Schullian P, Laimer G, Johnston E, Putzer D, Eberle G, Widmann G, et al. Reliability of stereotactic radiofrequency ablation (SRFA) for malignant liver tumors: novice versus experienced operators. Biology (Basel). 2023;12:175. https://doi.org/10.3390/biology12020175.
Uppot RN, Laguna B, McCarthy CJ, De Novi G, Phelps A, Siegel E, et al. Implementing virtual and augmented reality tools for radiology education and training, communication, and clinical care. Radiology. 2019;291:570–80. https://doi.org/10.1148/radiol.2019182210.
Barsom EZ, Graafland M, Schijven MP. Systematic review on the effectiveness of augmented reality applications in medical training. Surg Endosc. 2016;30:4174–83. https://doi.org/10.1007/s00464-016-4800-6.
Kim Y, Kim H, Kim YO. Virtual reality and augmented reality in plastic surgery: a review. Arch Plast Surg. 2017;44:179–87. https://doi.org/10.5999/aps.2017.44.3.179.
Buchs NC, Volonte F, Pugin F, Toso C, Fusaglia M, Gavaghan K, et al. Augmented environments for the targeting of hepatic lesions during image-guided robotic liver surgery. J Surg Res. 2013;184:825–31. https://doi.org/10.1016/j.jss.2013.04.032.
Perkins SL, Lin MA, Srinivasan S, Wheeler AJ, Hargreaves BA, Daniel BL (2017) A mixed-reality system for breast surgical planning. In: 2017 IEEE International symposium on mixed and augmented reality (ISMAR-Adjunct), pp. 269–74. https://doi.org/10.1109/ISMAR-Adjunct.2017.92
Mohammed MAA, Khalaf MH, Kesselman A, Wang DS, Kothary N. A role for virtual reality in planning endovascular procedures. J Vasc Interv Radiol. 2018;29:971–4. https://doi.org/10.1016/j.jvir.2018.02.018.
Solbiati LA. Augmented reality: thrilling future for interventional oncology? Cardiovasc Intervent Radiol. 2021;44:782–3. https://doi.org/10.1007/s00270-021-02801-9.
Farshad-Amacker NA, Kubik-Huch RA, Kolling C, Leo C, Goldhahn J. Learning how to perform ultrasound-guided interventions with and without augmented reality visualization: a randomized study. Eur Radiol. 2022. https://doi.org/10.1007/s00330-022-09220-5.
Mahmood F, Mahmood E, Dorfman RG, Mitchell J, Mahmood F-U, Jones SB, et al. Augmented reality and ultrasound education: initial experience. J Cardiothorac Vasc Anesth. 2018;32:1363–7. https://doi.org/10.1053/j.jvca.2017.12.006.
Chalhoub J, Ayer SK, Ariaratnam ST. Augmented reality for enabling un and under trained individuals to complete specialty construction tasks. J Inf Technol Constr (ITcon). 2021. https://doi.org/10.36680/j.itcon.2021.008.
Hiranaka T, Fujishiro T, Hida Y, Shibata Y, Tsubosaka M, Nakanishi Y, et al. Augmented reality: the use of the PicoLinker smart glasses improves wire insertion under fluoroscopy. World J Orthop. 2017;8:891–4. https://doi.org/10.5312/wjo.v8.i12.891.
Ghaednia H, Fourman MS, Lans A, Detels K, Dijkstra H, Lloyd S, et al. Augmented and virtual reality in spine surgery, current applications and future potentials. Spine J. 2021;21:1617–25. https://doi.org/10.1016/j.spinee.2021.03.018.
Funding
L.S. was supported by Institut Servier research grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent for Publication
For this type of study consent for publication is not required.
Informed Consent
For this type of study informed consent is not required.
Human and Animal Participants
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Saccenti, L., Bessy, H., Ben Jedidia, B. et al. Performance Comparison of Augmented Reality Versus Ultrasound Guidance for Puncture: A Phantom Study. Cardiovasc Intervent Radiol (2024). https://doi.org/10.1007/s00270-024-03727-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00270-024-03727-8