Abstract
Aim
Percutaneous transluminal angioplasty (PTA) is widely used as the primary treatment for dialysis vascular access dysfunction. Nonetheless, many patients develop early occlusion after angioplasty. Thus, we investigated the role of thrombophilia in access occlusion within 30 days of angioplasty.
Materials and Methods
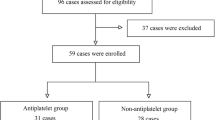
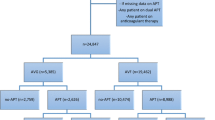
This case–control study included patients who underwent PTA for dialysis vascular access dysfunction. Patients who experienced occlusion within 30 days of angioplasty were included in the case group and those without occlusion for at least 30 days after angioplasty were included in the control group. All patients were tested for protein C, protein S, antithrombin III, lupus anticoagulant, and anticardiolipin antibodies.
Results
From February to October 2015, 462 patients underwent PTA for dialysis vascular access dysfunction. Forty-one patients (8.9%) had early occlusion within 30 days of angioplasty. The case group had more graft accesses (73 vs. 31%, P < 0.001) and thrombotic occlusions (67 vs. 15%, P < 0.001). A higher incidence of protein C (10 vs. 2%), protein S (15 vs. 5%), and antithrombin III (10 vs. 2%) deficiency and elevated anticardiolipin antibody (22 vs. 10%) levels were observed in the case group. Overall, 26 patients (63%) in the case group had at least one thrombophilic factor, compared with 15 patients (37%) in the control group (unadjusted odds ratio [OR], 3.004; 95% confidence interval [CI], 1.223–7.380; P = 0.027). After adjustment for confounding factors, the association between thrombophilic factors and early occlusion remained (adjusted OR, 3.806; 95% CI, 1.018–14.220; P = 0.047).
Conclusion
Thrombophilia is associated with early occlusion after angioplasty for hemodialysis vascular access.


Similar content being viewed by others
References
National Kidney Foundation. Dialysis outcomes quality initiative: NKF-DOQI clinical practice guidelines for vascular access. Am J Kidney Dis. 1997;30(4 Suppl 3):S150–91.
Neuen BL, Gunnarsson R, Baer RA, Tosenovsky P, Green SJ, Golledge J, et al. Factors associated with patency following angioplasty of hemodialysis fistulae. J Vasc Interv Radiol. 2014;25(9):1419–26.
Lilly RZ, Carlton D, Barker J, Saddekni S, Hamrick K, Oser R, et al. Predictors of arteriovenous graft patency after radiologic intervention in hemodialysis patients. Am J Kidney Dis. 2001;37(5):945–53.
Schwab SJ, Oliver MJ, Suhocki P, McCann R. Hemodialysis arteriovenous access: detection of stenosis and response to treatment by vascular access blood flow. Kidney Int. 2001;59(1):358–62.
Sarkar O, Assadian A, Frank H, Moessmer G, Heemann U, Eckstein HH. Hereditary and acquired thrombophilic disorders complicating vascular access in haemodialysis: O. Sarkar et al. NDT Plus. 2010;3(4):393–6.
Knoll GA, Wells PS, Young D, Perkins SL, Pilkey RM, Clinch JJ, et al. Thrombophilia and the risk for hemodialysis vascular access thrombosis. J Am Soc Nephrol. 2005;16(4):1108–14.
Manns BJ, Burgess ED, Parsons HG, Schaefer JP, Hyndman ME, Scott-Douglas NW. Hyperhomocysteinemia, anticardiolipin antibody status, and risk for vascular access thrombosis in hemodialysis patients. Kidney Int. 1999;55(1):315–20.
Nampoory MR, Das KC, Johny KV, Al-Hilali N, Abraham M, Easow S, et al. Hypercoagulability, a serious problem in patients with ESRD on maintenance hemodialysis, and its correction after kidney transplantation. Am J Kidney Dis. 2003;42(4):797–805.
O’Shea SI, Lawson JH, Reddan D, Murphy M, Ortel TL. Hypercoagulable states and antithrombotic strategies in recurrent vascular access site thrombosis. J Vasc Surg. 2003;38(3):541–8.
Wu CC, Wen SC, Chen MK, Yang CW, Pu SY, Tsai KC, et al. Radial artery approach for endovascular salvage of occluded autogenous radial-cephalic fistulae. Nephrol Dial Transplant. 2009;24(8):2497–502.
Wu CC, Lin MC, Pu SY, Tsai KC, Wen SC. Comparison of cutting balloon versus high-pressure balloon angioplasty for resistant venous stenoses of native hemodialysis fistulas. J Vasc Interv Radiol. 2008;19(6):877–83.
Wu CC, Hsieh MY, Hung SC, Kuo KL, Tsai TH, Lai CL, et al. Serum indoxyl sulfate associates with postangioplasty thrombosis of dialysis grafts. J Am Soc Nephrol. 2016;27(4):1254–64.
Hsieh MY, Chen TY, Lin L, Chuang SY, Lin SJ, Tarng DC, et al. Deficiency of circulating progenitor cells associated with vascular thrombosis of hemodialysis patients. Nephrol Dial Transplant. 2017;32(3):556–64.
Welt FG, Rogers C. Inflammation and restenosis in the stent era. Arterioscler Thromb Vasc Biol. 2002;22(11):1769–76.
Otsuka F, Finn AV, Yazdani SK, Nakano M, Kolodgie FD, Virmani R. The importance of the endothelium in atherothrombosis and coronary stenting. Nat Rev Cardiol. 2012;9(8):439–53.
Padfield GJ, Newby DE, Mills NL. Understanding the role of endothelial progenitor cells in percutaneous coronary intervention. J Am Coll Cardiol. 2010;55(15):1553–65.
Zavalloni D, Presbitero P, Lodigiani C, Mango R, Cogliati T, Quaglia I, et al. Prevalence of inherited thrombophilia in patients with documented stent thrombosis. Circ J. 2012;76(8):1874–9.
Kim RJ, Becker RC. Association between factor V Leiden, prothrombin G20210A, and methylenetetrahydrofolate reductase C677T mutations and events of the arterial circulatory system: a meta-analysis of published studies. Am Heart J. 2003;146(6):948–57.
Adler S, Szczech L, Qureshi A, Bollu R, Thomas-John R. IgM anticardiolipin antibodies are associated with stenosis of vascular access in hemodialysis patients but do not predict thrombosis. Clin Nephrol. 2001;56(6):428–34.
Chuang FR, Chang HW, Lin CL, Wang IK, Chang HY, Wang PH, et al. Anticardiolipin antibody and Taiwanese chronic haemodialysis patients with recurrent vascular access thrombosis. Int J Clin Pract. 2005;59(7):785–90.
Cockwell P, Tse WY, Savage CO. Activation of endothelial cells in thrombosis and vasculitis. Scand J Rheumatol. 1997;26(3):145–50.
Prakash R, Miller CC 3rd, Suki WN. Anticardiolipin antibody in patients on maintenance hemodialysis and its association with recurrent arteriovenous graft thrombosis. Am J Kidney Dis. 1995;26(2):347–52.
Crowther MA, Clase CM, Margetts PJ, Julian J, Lambert K, Sneath D, et al. Low-intensity warfarin is ineffective for the prevention of PTFE graft failure in patients on hemodialysis: a randomized controlled trial. J Am Soc Nephrol. 2002;13(9):2331–7.
Kaufman JS, O’Connor TZ, Zhang JH, Cronin RE, Fiore LD, Ganz MB, et al. Randomized controlled trial of clopidogrel plus aspirin to prevent hemodialysis access graft thrombosis. J Am Soc Nephrol. 2003;14(9):2313–21.
Lee PC, Lee PH, Shaw CK, Lei HY, Chen JC, Takemoto S. Effectiveness of an organ-sharing program in providing zero HLA-A, B, DR mismatched kidneys for transplantation in Taiwan. J Formos Med Assoc. 2000;99(6):447–52.
Shen MC, Lin JS, Tsay W. High prevalence of antithrombin III, protein C and protein S deficiency, but no factor V Leiden mutation in venous thrombophilic Chinese patients in Taiwan. Thromb Res. 1997;87(4):377–85.
Liu HW, Kwong YL, Bourke C, Lam CK, Lie AK, Wei D, et al. High incidence of thrombophilia detected in Chinese patients with venous thrombosis. Thromb Haemost. 1994;71(4):416–9.
Rabes JP, Trossaert M, Conard J, Samama M, Giraudet P, Boileau C. Single point mutation at Arg506 of factor V associated with APC resistance and venous thromboembolism: improved detection by PCR-mediated site-directed mutagenesis. Thromb Haemost. 1995;74(5):1379–80.
Acknowledgements
We thank the staff of Biotechnology R&D Center, National Taiwan University Hospital, Hsin-Chu Branch for their assistance in statistical analysis and interpretation of results.
Funding
This study was funded by National Taiwan University Hospital, Hsinchu Branch (Grant Numbers HCH104-10 and HCH105-7) and by the Ministry of Science and Technology (Grant Number 106-2314-B-002-173-MY3). The funders had no role in the study design, in the collection, analysis or interpretation of data, in writing this report, or in the decision to submit this report for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Chen, TY., Lin, L., Hsieh, MY. et al. Thrombophilia Associated with Early Post-angioplasty Thrombosis of Dialysis Vascular Access. Cardiovasc Intervent Radiol 41, 1683–1690 (2018). https://doi.org/10.1007/s00270-018-2046-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-018-2046-5