Abstract
Purpose
To compare radiation exposure of adrenal venous sampling (AVS) using dynamic trace digital angiography (DTDA) and spot fluoroscopy with that using conventional methods.
Materials and Methods
AVS was performed in 11 patients using DTDA and spot fluoroscopy (Group A) and 11 patients using conventional digital subtraction angiography (DSA) with collimation (Group B). Radiation exposure and image quality of adrenal venography using a five-point scale were compared between the groups.
Results
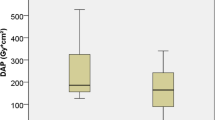
The acquisition dose–area product (DAP) using DTDA and fluoro-DAP using spot fluoroscopy in Group A were lower than those using conventional DSA (5.3 ± 3.7 vs. 29.1 ± 20.1 Gy cm2, p < 0.001) and collimation (33.3 ± 22.9 vs. 59.1 ± 35.7 Gy cm2, p = 0.088) in Group B. The total DAP in Group A was significantly lower than that in Group B (38.6 ± 25.9 vs. 88.2 ± 53.6 Gy cm2, p = 0.006). The peak skin dose for patients and operator radiation exposure in Group A were significantly lower than those in Group B (403 ± 340 vs. 771 ± 416 mGy, p = 0.030, and 17.1 ± 14.8 vs. 36.6 ± 21.7 μSv, p = 0.013). The image quality of DTDA (4.4 ± 0.6) was significantly higher than that of digital angiography (3.8 ± 0.9, p = 0.011) and equivalent to that of DSA (4.3 ± 0.8, p = 0.651).
Conclusions
Radiation exposure during AVS can be reduced by approximately half for both patients and operators by using DTDA and spot fluoroscopy without sacrificing image quality.



Similar content being viewed by others
References
Nishikawa T, Omura M, Satoh F, Task Force Committee on Primary Aldosteronism, The Japan Endocrine Society, et al. Guidelines for the diagnosis and treatment of primary aldosteronism—the Japan Endocrine Society 2009. Endocr J. 2011;58(9):711–21.
Funder JW, Carey RM, Fardella C, Endocrine Society, et al. Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2008;93(9):3266–81.
Rossi GP, Auchus RJ, Brown M, et al. An expert consensus statement on use of adrenal vein sampling for the subtyping of primary aldosteronism. Hypertension. 2014;63(1):151–60.
Nishikawa T, Matsuzawa Y, Saito J, Omura M. Is it possible to extirpate cardiovascular events in primary aldosteronism after surgical treatment. Jpn Clin Med. 2010;30(1):21–3.
Satani N, Ota H, Seiji K, et al. Intra-adrenal aldosterone secretion: segmental adrenal venous sampling for localization. Radiology. 2016;278(1):265–74.
Morita S, Yamazaki H, Sonoyama Y, Nishina Y, Ichihara A, Sakai S. Successful adrenal venous sampling by non-experts with reference to CT images. Cardiovasc Intervent Radiol. 2016;39(7):1001–6.
Busser WM, Arntz MJ, Jenniskens SF, et al. Image registration of cone-beam computer tomography and preprocedural computer tomography aids in localization of adrenal veins and decreasing radiation dose in adrenal vein sampling. Cardiovasc Intervent Radiol. 2015;38(4):993–7.
McAdams HP, Samei E, Dobbins J 3rd, Tourassi GD, Ravin CE. Recent advances in chest radiography. Radiology. 2006;241(3):663–83.
Borota L, Patz A, Uppsala SE, Zoetermeer NL. Spot Fluoro—A novel innovative approach to reduce the dose in interventional procedures—advantages and drawbacks. ECR 2014 C-1428.
Miller DL, Vañó E, Bartal G, Cardiovascular and Interventional Radiology Society of Europe, Society of Interventional Radiology, et al. Occupational radiation protection in interventional radiology: a joint guideline of the Cardiovascular and Interventional Radiology Society of Europe and the Society of Interventional Radiology. J Vasc Interv Radiol. 2010;21(5):607–15.
Stecker MS, Balter S, Towbin RB, SIR Safety and Health Committee, CIRSE Standards of Practice Committee, et al. Guidelines for patient radiation dose management. J Vasc Interv Radiol. 2009;20(7 Suppl):S263–73.
Acknowledgement
The authors wish to thank Takako Hidaka of Toshiba Medical Systems for technical advice, and Takafumi Shiohara and Akira Mitsuhasi of Central Department of Radiology, Tokyo Women’s Medical University Hospital for image acquisition.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Morita, S., Endo, K., Suzaki, S. et al. Reduction of Radiation Exposure Using Dynamic Trace Digital Angiography and Spot Fluoroscopy During Adrenal Venous Sampling. Cardiovasc Intervent Radiol 40, 697–703 (2017). https://doi.org/10.1007/s00270-017-1567-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-017-1567-7