Abstract
Purpose
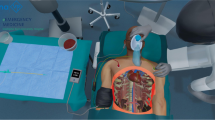
This study evaluates a fully immersive simulated angiosuite for training and assessment of technical endovascular and human factor skills during a crisis scenario.
Materials and Methods
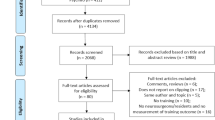
Virtual reality (VIST-C, Mentice) simulators were integrated into a simulated angiosuite (ORCAMP, Orzone). Teams, lead by experienced (N = 5) or trainee (N = 5) endovascular specialists, performed simulated endovascular ruptured aortic aneurysm repair (rEVAR). Timed performance metrics were recorded as surrogate measures of performance. Participants (N = 22) completed postprocedure questionnaires evaluating face validity, as well as technical and human factor aspects, of the simulation on a Likert scale from 1 (not at all) to 5 (very much).
Results
Experienced team leaders were significantly faster than trainees in obtaining proximal control with an intra-aortic occlusion balloon (352 vs. 501 s, p = 0.047) and all completed the procedure within the allotted time, whilst no trainee was able to do so. Total fluoroscopy times were significantly lower in the experienced group (782 vs. 1,086 s, p = 0.016). Realism of the simulated angiosuite was scored highly by experienced team leaders (median 4/5, IQR 4–5). Participants found the simulation useful for acquiring technical (4/5, IQR 4–5) and communication skills (4/5, IQR 4–5) and particularly valuable for enhancing teamwork (5/5, IQR 4–5) and patient safety (5/5, IQR 4–5).
Conclusion
This study shows feasibility of creation of a crisis scenario in a fully immersive angiosuite simulation and team performance of a simulated rEVAR. Performance metrics differentiated between experienced specialists and trainees, and the realism of the simulation exercise and environment were rated highly by experienced endovascular specialists. This simulation has potential as a powerful training and assessment tool with opportunities to improve team performance in rEVAR through both technical and human factor skills training.




Similar content being viewed by others
References
Mayer D, Aeschbacher S, Pfammatter T et al (2012) Complete replacement of open repair for ruptured abdominal aortic aneurysms by endovascular aneurysm repair: a two-center 14-year experience. Ann Surg 256(5):688–695
Choke E, Vijaynagar B, Thompson J et al (2012) Changing epidemiology of abdominal aortic aneurysms in England and Wales: older and more benign? Circulation 125(13):1617–1625
Mayer D, Pfammatter T, Rancic Z et al (2009) 10 years of emergency endovascular aneurysm repair for ruptured abdominal aortoiliac aneurysms: lessons learned. Ann Surg 249(3):510–515
Reichart M, Geelkerken RH, Huisman AB et al (2003) Ruptured abdominal aortic aneurysm: endovascular repair is feasible in 40 % of patients. Eur J Vasc Endovasc Surg 26(5):479–486
Peppelenbosch N, Yilmaz N, van Marrewijk C et al (2003) Emergency treatment of acute symptomatic or ruptured abdominal aortic aneurysm. Outcome of a prospective intent-to-treat by EVAR protocol. Eur J Vasc Endovasc Surg 26(3):303–310
Franks S, Lloyd G, Fishwick G et al (2006) Endovascular treatment of ruptured and symptomatic abdominal aortic aneurysms. Eur J Vasc Endovasc Surg 31(4):345–350
Seymour NE, Gallagher AG, Roman SA et al (2002) Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 236(4):458–463
Walsh CM, Sherlock ME, Ling SC (2012) Virtual reality simulation training for health professions trainees in gastrointestinal endoscopy. Cochrane Database Syst Rev 6:CD008237
Dawson DL, Meyer J, Lee ES et al (2007) Training with simulation improves residents’ endovascular procedure skills. J Vasc Surg 45(1):149–154
Van Herzeele I, Aggarwal R, Neequaye S et al (2008) Experienced endovascular interventionalists objectively improve their skills by attending carotid artery stent training courses. Eur J Vasc Endovasc Surg 35(5):541–550
Chaer RA, Derubertis BG, Lin SC et al (2006) Simulation improves resident performance in catheter-based intervention: results of a randomized, controlled study. Ann Surg 244(3):343–352
Hseino H, Nugent E, Lee MJ et al (2012) Skills transfer after proficiency-based simulation training in superficial femoral artery angioplasty. Simul Healthc 7(5):274–281
Undre S, Koutantji M, Sevdalis N et al (2007) Multidisciplinary crisis simulations: the way forward for training surgical teams. World J Surg 31(9):1843–1853
Lonn L, Edmond JJ, Marco J et al (2012) Virtual reality simulation training in a high-fidelity procedure suite: operator appraisal. J Vasc Interv Radiol 23(10):1361–1366
Vincent C, Moorthy K, Sarker S et al (2004) Systems approaches to surgical quality and safety: from concept to measurement. Ann Surg 239(4):475–482
Morbi AH, Hamady MS, Riga CV et al (2012) Reducing error and improving efficiency during vascular interventional radiology: implementation of a preprocedural team rehearsal. Radiology 264(2):473–483
Albayati MA, Gohel MS, Patel SR et al (2011) Identification of patient safety improvement targets in successful vascular and endovascular procedures: analysis of 251 hours of complex arterial surgery. Eur J Vasc Endovasc Surg 41(6):795–802
McCulloch P, Mishra A, Handa A et al (2009) The effects of aviation-style non-technical skills training on technical performance and outcome in the operating theatre. Qual Saf Health Care 18(2):109–115
Morey JC, Simon R, Jay GD et al (2002) Error reduction and performance improvement in the emergency department through formal teamwork training: evaluation results of the MedTeams project. Health Serv Res 37(6):1553–1581
Malec JF, Torsher LC, Dunn WF et al (2007) The mayo high performance teamwork scale: reliability and validity for evaluating key crew resource management skills. Simul Healthc 2(1):4–10
Mishra A, Catchpole K, McCulloch P (2009) The Oxford NOTECHS system: reliability and validity of a tool for measuring teamwork behaviour in the operating theatre. Qual Saf Health Care 18(2):104–108
Acknowledgments
We acknowledge with thanks the participants and faculty on the Imperial College Vascular Interventional Radiology Virtual Reality Simulation Course 2012, Mentice (Gothenburg, Sweden) for providing VR simulators and technical support and Orzone (Gothenburg, Sweden) for providing technical support. This research was funded by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Imperial College Healthcare National Health Service (NHS) Trust and Imperial College London. The views expressed are those of the authors and not necessarily those of the NHS, NIHR or the Department of Health.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rudarakanchana, N., Van Herzeele, I., Bicknell, C.D. et al. Endovascular Repair of Ruptured Abdominal Aortic Aneurysm: Technical and Team Training in an Immersive Virtual Reality Environment. Cardiovasc Intervent Radiol 37, 920–927 (2014). https://doi.org/10.1007/s00270-013-0765-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-013-0765-1