Abstract
Background
Postoperative complications are not rare in the elderly population after hepatectomy. However, predicting postoperative risk in elderly patients undergoing hepatectomy is not easy. We aimed to develop a new preoperative evaluation method to predict postoperative complications in patients above 65 years of age using biological impedance analysis (BIA).
Methods
Clinical data of 59 consecutive patients (aged 65 years or older) who underwent hepatectomy at our institution between 2017 and 2020 were retrospectively analyzed. Risk factors for postoperative complications (Clavien-Dindo ≥ III) were evaluated using multivariate regression analysis. Additionally, a new preoperative risk score was developed for predicting postoperative complications.
Results
Fifteen patients (25.4%) had postoperative complications, with biliary fistula being the most common complication. Abnormal skeletal muscle mass index from BIA and type of surgical procedure were found to be independent risk factors in the multivariate analysis. These two variables and preoperative serum albumin levels were used for developing the risk score. The postoperative complication rate was 0.0% with a risk score of ≤ 1 and 57.1% with a risk score of ≥ 4. The area under the receiver operating characteristic curve of the risk score was 0.810 (p = 0.001), which was better than that of other known surgical risk indexes.
Conclusion
Decreased skeletal muscle and the type of surgical procedure for hepatectomy were independent risk factors for postoperative complications after elective hepatectomy in elderly patients. The new preoperative risk score is simple, easy to perform, and will help in the detection of high-risk elderly patients undergoing elective hepatectomy.
Similar content being viewed by others
Introduction
Generally, elderly patients have a high incidence of comorbidity (9.0–52.5%) and are usually considered a high-risk group for hepatectomy [1, 2]. According to a report of the Japanese Nationwide Survey on hepatocellular carcinoma (HCC) resection, elderly patients had significantly worse overall survival probabilities than younger patients (the 5-year overall survival probabilities: 68.8% vs. 59.5%; hazard ratio: 0.76). Furthermore, the cumulative incidence of HCC- or liver-related death was almost identical between elderly and younger patients, though the cumulative incidence of other causes of death was higher in the elderly (subdistribution hazard ratio: 0.32) [3]. For example, preoperative frailty in elderly patients undergoing hepatectomy is associated with age-related events such as cardiopulmonary complications, delirium, transfer to a rehabilitation facility, and dependency [4]. Thus, the indication of hepatectomy for elderly patients should be considered based on not only the tumor condition and liver function but also the risks specific to elderly patients.
However, predicting postoperative risk in elderly patients undergoing hepatectomy is not easy because of the lack of a reliable preoperative evaluation system. For example, estimation of physiological ability and surgical stress (E-PASS) [5] and physiological and operative severity score for the enumeration of mortality and morbidity (POSSUM) scores [6] have been reported previously for predicting postoperative complications in elderly patients with HCC. However, these systems are complicated and not specific for the elderly or hepatectomy. Simons et al. also reported an original risk score of in-hospital mortality for HCC resection [7]; however, this score cannot predict postoperative complications.
Therefore, we aimed to establish a new simple preoperative evaluation system for predicting postoperative complications in elderly patients undergoing elective hepatectomy. Biological impedance analysis (BIA), which is different from tests for the evaluation of tumor condition or liver function, was introduced in this study to evaluate patients’ preoperative body composition. BIA can be used to measure body water content, muscle mass, and fat mass using electrical impedance [8] and to diagnose decreased skeletal muscle, which is an element of sarcopenia and an important prognostic factor for hepatectomy for both HCC [9] and colorectal liver metastasis [10].
Material and methods
Subjects
The clinical data of 74 consecutive patients (≥ 65 years) who underwent hepatectomy at the Tokyo Medical University Hachioji Medical Center between May 2017 and April 2020 were analyzed retrospectively. These included patients with HCC, liver metastasis, and gallbladder carcinoma. Patients undergoing surgical procedures ranging from partial hepatectomy to trisectionectomy were included; however, four patients undergoing hepatopancreatoduodenectomy were excluded because such patients are at a much higher risk for postoperative complications than patients undergoing other procedures included here [11]. Moreover, 11 patients who could not undergo BIA, for reasons described below, were excluded. After excluding these cases, the remaining 59 cases were included in this study (Fig. 1).
All patients underwent blood tests preoperatively, including serum total bilirubin, albumin, prothrombin, and indocyanine green tests. In terms of disease diagnosis, especially for patients with HCC, the pathological liver-fibrosis stage was evaluated according to the METAVIR fibrosis score [12].
This study was approved by the institutional review board of Tokyo Medical University (T2020-0174). Informed consent was obtained from all patients.
BIA
In the present study, the InBody 770 (Biospace Co., Seoul, Korea) device was used for BIA. BIA was performed preoperatively in the physiology laboratory before or after admission. The InBody 770 device can be used to measure each patient’s characteristics in 90 s, with the patient holding the machine while standing upright. BIA can be used to measure body weight, water content (intra- and extra-cellular), amount of protein, skeletal muscle mass, muscle mass of extremities, fat mass, body cell mass, and minerals [8]. During the study, skeletal muscle mass (kg), skeletal muscle mass index (SMI), body fat (kg), and body cell mass (kg) were measured. The SMI cut-off value was based on the Asian Working Group for Sarcopenia (AWGS) criteria [13]. SMI values lower than 7.0 kg/m2 for male patients and 5.7 kg/m2 for female patients were considered abnormal. Generally, the BIA could not be performed in patients with metal objects inside the body, such as a cardiac pacemaker, or those who could not stand unassisted. These patients were excluded from this study.
Evaluation of the liver function
At our institution, the preoperative evaluation of liver function is achieved by performing blood tests, including a liver function test, indocyanine green retention rate at 15 min, and 99mTc-galactosyl human serum albumin (GSA) scintigraphy. The usefulness of 99mTc-GSA scintigraphy was reported previously [14].
Postoperative complications
The postoperative complications were graded using the Clavien-Dindo classification [15], which is a representative grading system for postoperative complications used worldwide. This study aimed to predict complications with a Clavien-Dindo Grade III or higher because such patients need invasive treatment.
Development of new preoperative risk score
The risk factors for postoperative complications (Clavien-Dindo ≥ III) were evaluated by univariate and multivariate analyses. The risk score for predicting postoperative complications was developed based on significant factors and serum albumin from the multivariate analysis. Scores were assigned for each variable according to the beta-coefficient value from the logistic regression analysis.
Surgical risk indexes
The new risk score was compared with other known surgical risk indexes. These included the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) surgical risk [16], American Society of Anesthesiologists (ASA) classification, E-PASS [17], POSSUM [18], and Portsmouth-POSSUM (P-POSSUM) [19].
Statistical analyses and development of risk score
All statistical analyses were performed using IBM SPSS Statistics, version 26.0 (IBM Corp., Armonk, N.Y., the USA). Continuous variables are expressed as the median and range (minimum–maximum). The Mann–Whitney U-test was used to evaluate the significance of the difference between groups. Categorical variables were compared using the Chi-square test or Fisher’s exact test, as required. Multivariate analysis was performed using logistic regression analysis with a forward selection of the likelihood ratio. The performance of the risk score was evaluated using receiver operating characteristic (ROC) analysis, and the area under the ROC curve (AUROC) was calculated. All statistical tests were two-tailed, and significance was set at a pvalue of < 0.05.
Results
Patient characteristics
The patient characteristics are shown in Table 1. In total, there were 34 male and 25 female patients with a median age of 75 years. Hypertension was the most common comorbidity observed in patients. HCC and liver metastasis were diagnosed in 44.1% and 32.2% of the patients, respectively. The median SMI using the InBody 770 device was 7.1 kg/m2 in male and 5.8 kg/m2 in female patients; both were only slightly higher than the AWGS cut-off values. The number of patients who underwent the different surgical procedures was as follows: partial hepatectomy, 29 (49.2%); segmentectomy, 6 (10.2%); sectionectomy, 7 (11.9%); hemihepatectomy or bisectionectomy, 14 (23.7%); and trisectionectomy, 3 (5.1%). Combined biliary resection was performed in three cases (two for perihilar cholangiocarcinoma and one for gallbladder carcinoma).
In terms of the postoperative complications, 12 patients (20.3%) had Clavien-Dindo ≥ III, whereas no patient died (Clavien-Dindo V) during this study. Among the observed postoperative complications, biliary fistula was the most common (13.6%). There were few cases of other complications, such as intra-abdominal abscess, pulmonary complications, and ileus. None of these patients had posthepatectomy liver failure of Clavien-Dindo ≥ III.
Univariate and multivariate analyses of postoperative complications
The results of the univariate and multivariate analyses of postoperative complications are shown in Table 2. In the univariate analysis, there was a significant difference in the serum albumin level (lower than 3.5 g/dL) and the type of surgical procedure between the two groups (Clavien-Dindo ≥ III and Clavien-Dindo ≤ II). Multivariate analysis revealed that abnormal SMI and the type of surgical procedure were independent risk factors for postoperative complications (p < 0.05).
Risk score for predicting postoperative complications
Based on the results of the multivariate analysis, abnormal albumin levels, abnormal SMI, and the type of surgical procedure were used for developing the risk score for predicting the postoperative complications. The scores were assigned based on the coefficient value for each item in the logistic regression model (Table 3). The risk score of patients ranged from 0 to 5. The estimated probability of postoperative complications between each risk score is shown in Fig. 2. The postoperative complication rate was 0.0% for patients with a risk score of ≤ 1 and 57.1% for those with a risk score of ≥ 4.
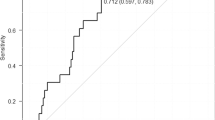
Comparison of the risk score performance
The results of the ROC analysis of the new risk score and other known surgical risk indexes for predicting postoperative complications are shown in Fig. 3. The corresponding AUROCs are shown in Table 4. Among these scores or indexes, the new risk score showed the best result, with an AUROC of 0.810 (p = 0.001).
Discussion
The present study revealed that preoperative decreased skeletal muscle and the type of surgical procedure used for hepatectomy appeared to have a statistically significant impact on the Clavien-Dindo ≥ III postoperative complications among patients aged 65 years or older undergoing hepatectomy. In this report, the preoperative risk assessment of the elderly undergoing hepatectomy is discussed from a new perspective using BIA.
Recently, sarcopenia has increasingly been recognized as an important factor in predicting postoperative complications and long-term prognosis among patients undergoing gastrointestinal surgery [20]. Decreased skeletal muscle is an important element of sarcopenia. The guidelines from the American College of Surgeons have also highlighted the importance of assessing sarcopenia before surgical oncology in the elderly [21]. Valero et al. showed that a low preoperative psoas muscle mass is an independent risk factor for postoperative complications in patients with Clavien-Dindo ≥ III undergoing hepatectomy and liver transplantation for HCC [22]. Higashi et al. similarly reported that sarcopenia is a risk factor for postoperative complications in patients undergoing major hepatectomy. They also mentioned that sarcopenia is a risk factor for liver-related morbidity and mortality in patients aged > 70 years [23]. According to another report, low skeletal muscle mass and quality are also related to mortality after resection of intrahepatic cholangiocarcinomas [24]. Thus, sarcopenia or decreased skeletal muscle is a risk factor for hepatectomy, though it has not been used as an item of preoperative risk index before.
In the present study, we used the BIA for diagnosis of decreased skeletal muscle mass. BIA can be used to evaluate the body composition precisely by calculating the electrical impedance of a patient’s body. The usefulness of the BIA has already been confirmed widely in liver cirrhosis [25] and living donor liver transplantation patients [26]. However, in almost all of the previously cited reports, the psoas or skeletal muscle mass was calculated either using L3-level computed tomography (CT) or magnetic resonance imaging (MRI). The area of skeletal muscle at the L3 level was directly correlated with whole-body skeletal muscle [27]. This method had the advantage that most of our hepatectomy patients underwent CT or MRI preoperatively, meaning that there was no need for performing other tests. These methods approximate the BIA, though they can be used as a substitute for BIA, especially when an institution lacks BIA equipment. However, the BIA has the disadvantage that the optimal cut-off values for SMI in the elderly population have not been determined. Because of the lack of optimal cut-off values of SMI in both the elderly population and in hepatectomy patients, the AWGS criteria were used in this study. Further studies will be needed to determine the optimal cut-off value, especially in elderly patients.
Furthermore, there are some reports on the relationship between body composition (other than muscle mass) and postoperative complications in hepatectomy. Low preoperative body cell mass is a risk factor for infections associated with mortality in cases of living donor liver transplantation [26]. In line with this study, we evaluated the body cell mass, though no significant difference was observed in our study cohort. Hamaguchi et al. reported that preoperative muscle steatosis in patients undergoing hepatectomy for HCC is an independent risk factor for postoperative complications in patients with Clavien-Dindo ≥ III and infectious complications [28]. In another study, it was reported that a low preoperative SMI value, high intramuscular adipose tissue content, and high visceral-to-subcutaneous adipose tissue-area ratio were risk factors for mortality and recurrence in patients undergoing hepatectomy for HCC [29]. In this study, only total body fat was evaluated, with no significant difference observed in this parameter.
Serum albumin was previously shown to be an independent risk factor for postoperative complications in elderly patients undergoing hepatectomy [5]. Therefore, the preoperative serum albumin levels, in addition to the SMI value and the type of surgical procedure, were also included in the development of the new preoperative risk score for predicting postoperative complications. Based on these three items, we developed a new, simple preoperative risk score for elderly patients who underwent elective hepatectomy. There are already some other established risk assessment systems. For example, the ACS NSQIP surgical risk [16], E-PASS [17], POSSUM [18], and P-POSSUM [19] also showed relatively good results with significant differences in ROC analysis for predicting postoperative complications. However, our risk score showed better results and may be simpler and easier to use than these other risk assessment systems. Additionally, our risk score may have better performance than other systems because it focuses on hepatectomy in elderly patients and uses BIA, which has not been used in other systems.
Despite these significant findings, the present study has several limitations. This study was performed in a single center with a relatively small number of patients. Therefore, our risk score should be validated in other subjects in a multicenter study. Further, patients in whom BIA could not be performed, such as those with metal objects inside the body, or those who could not stand unassisted, were excluded from the study. Therefore, our risk score may not be applicable directly for these patients. Evaluation of psoas muscle mass at the L3 level is a possible substitute for BIA, although further studies are needed for confirmation. Also, elderly patients who were deemed too frail for the surgery did not undergo hepatectomy. Therefore, further prospective studies will be needed to exclude this preselection bias.
Conclusion
In conclusion, the present study revealed that decreased skeletal muscle and the type of surgical procedure for hepatectomy are independent risk factors for postoperative complications after elective hepatectomy in elderly patients. Furthermore, the new preoperative risk assessment system developed using serum albumin levels, SMI, and surgical procedure will help in the identification of high-risk elderly patients undergoing elective hepatectomy.
References
Zhou Y, Zhang X, Zhang Z et al (2013) Hepatectomy in elderly patients: does age matter? World J Surg 37:2899–2910. https://doi.org/10.1007/s00268-013-2184-5
Hung AK, Guy J (2015) Hepatocellular carcinoma in the elderly: meta-analysis and systematic literature review. World J Gastroenterol 21:12197–12210
Kaibori M, Yoshii K, Yokota I et al (2019) Impact of advanced age on survival in patients undergoing resection of hepatocellular carcinoma: report of a Japanese nationwide survey. Ann Surg 269:692–699
Tanaka S, Ueno M, Iida H et al (2018) Preoperative assessment of frailty predicts age-related events after hepatic resection: a prospective multicenter study. J Hepatobiliary Pancreat Sci 25:377–387
Ide T, Miyoshi A, Kitahara K et al (2013) Prediction of postoperative complications in elderly patients with hepatocellular carcinoma. J Surg Res 185:614–619
Oishi K, Itamoto T, Kohashi T et al (2014) Safety of hepatectomy for elderly patients with hepatocellular carcinoma. World J Gastroenterol 20:15028–15036
Simons JP, Ng SC, Hill JS et al (2010) In-hospital mortality from liver resection for hepatocellular carcinoma: a simple risk score. Cancer 116:1733–1738
Cha K, Chertow GM, Gonzalez J et al (1985) (1995) Multifrequency bioelectrical impedance estimates the distribution of body water. J Appl Physiol 79:1316–1319
Harimoto N, Shirabe K, Yamashita YI et al (2013) Sarcopenia as a predictor of prognosis in patients following hepatectomy for hepatocellular carcinoma. Br J Surg 100:1523–1530
van Vledder MG, Levolger S, Ayez N et al (2012) Body composition and outcome in patients undergoing resection of colorectal liver metastases. Br J Surg 99:550–557
Aoki T, Sakamoto Y, Kohno Y et al (2018) Hepatopancreaticoduodenectomy for biliary cancer: strategies for near-zero operative mortality and acceptable long-term outcome. Ann Surg 267:332–337
The French METAVIR Cooperative Study Group (1994) Intraobserver and interobserver variations in liver biopsy interpretation in patients with chronic hepatitis C. Hepatology 20:15–20
Chen LK, Liu LK, Woo J et al (2014) Sarcopenia in Asia: consensus report of the Asian working group for Sarcopenia. J Am Med Dir Assoc 15:95–101
Chiba N, Shimazu M, Takano K et al (2017) Predicting hepatic failure with a new diagnostic technique by preoperative liver scintigraphy and computed tomography: a pilot study in 123 patients undergoing liver resection. Patient Saf Surg 11:29
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Bilimoria KY, Liu Y, Paruch JL et al (2013) Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg 217:833-842.e3
Haga Y, Ikei S, Ogawa M (1999) Estimation of Physiologic Ability and Surgical Stress (E-PASS) as a new prediction scoring system for postoperative morbidity and mortality following elective gastrointestinal surgery. Surg Today 29:219–225
Copeland GP, Jones D, Walters M (1991) POSSUM: a scoring system for surgical audit. Br J Surg 78:355–360
Whiteley MS, Prytherch DR, Higgins B et al (1996) An evaluation of the POSSUM surgical scoring system. Br J Surg 83:812–815
Wagner D, DeMarco MM, Amini N et al (2016) Role of frailty and sarcopenia in predicting outcomes among patients undergoing gastrointestinal surgery. World J Gastrointest Surg 8:27–40
Chow WB, Rosenthal RA, Merkow RP et al (2012) Optimal preoperative assessment of the geriatric surgical patient: a best practices guideline from the American college of surgeons national surgical quality improvement program and the American geriatrics society. J Am Coll Surg 215:453–466
Valero V, Amini N, Spolverato G et al (2015) Sarcopenia adversely impacts postoperative complications following resection or transplantation in patients with primary liver tumors. J Gastrointest Surg 19:272–281
Higashi T, Hayashi H, Taki K et al (2016) Sarcopenia, but not visceral fat amount, is a risk factor of postoperative complications after major hepatectomy. Int J Clin Oncol 21:310–319
Okumura S, Kaido T, Hamaguchi Y et al (2017) Impact of skeletal muscle mass, muscle quality, and visceral adiposity on outcomes following resection of intrahepatic cholangiocarcinoma. Ann Surg Oncol 24:1037–1045
Nishikawa H, Enomoto H, Iwata Y et al (2017) Clinical utility of bioimpedance analysis in liver cirrhosis. J Hepatobiliary Pancreat Sci 24:409–416
Kaido T, Mori A, Ogura Y et al (2012) Pre- and perioperative factors affecting infection after living donor liver transplantation. Nutrition 28:1104–1108
Mourtzakis M, Prado CM, Lieffers JR et al (2008) A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab 33:997–1006
Hamaguchi Y, Kaido T, Okumura S et al (2016) Muscle steatosis is an independent predictor of postoperative complications in patients with hepatocellular carcinoma. World J Surg 40:1959–1968. https://doi.org/10.1007/s00268-016-3504-3
Hamaguchi Y, Kaido T, Okumura S et al (2019) Preoperative visceral adiposity and muscularity predict poor outcomes after hepatectomy for hepatocellular carcinoma. Liver Cancer 8:92–109
Funding
This study was funded by Grant-in-Aid for Scientific Research (16K10440) and Daiwa Securities Co., Ltd (46th Research Grant).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have conflicts of interest to declare.
Informed consent
Informed consent was obtained from all participants included in the study.
Ethical approval
This study was approved by the institutional review board of Tokyo Medical University (T2020-0174).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tomita, K., Koganezawa, I., Nakagawa, M. et al. A New Preoperative Risk Score for Predicting Postoperative Complications in Elderly Patients Undergoing Hepatectomy. World J Surg 45, 1868–1876 (2021). https://doi.org/10.1007/s00268-021-05985-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-05985-w