Abstract
Background
Pharyngolaryngeal symptoms are a main concern after neck surgery. The Protector™ LMA is a new supraglottic airway device. The main purpose of this study was to evaluate whether application of the LMA Protector™ causes fewer pharyngolaryngeal symptoms than application of the endotracheal tube after minimally invasive total thyroidectomy and parathyroidectomy.
Methods
This prospective, randomized controlled trial involved one university and one private practice clinic, during the period from January 2017 until November 2017. The patients were randomly allocated to two groups: ETT and LMA. Main outcomes were Numerical Rating Scale scores of postoperative dysphagia, pharyngodynia, and incisional pain. Secondary outcomes were the frequency of rescue analgesia (paracetamol) consumption and emergence cough. Data were recorded in the post-anesthesia care unit and at 1, 6, 12, and 24 h after surgery.
Results
Data from 78 patients were included in the final analysis. Pharyngodynia scores were significantly lower in the LMA group, compared with the ETT group, at 1 h, 6 h and 12 h after surgery. Dysphagia and surgical incision pain scores were also significantly lower in the LMA group, compared with the ETT group, at 6 h and 12 h after surgery. The frequency of postoperative paracetamol consumption was significantly increased in the ETT group, compared with the LMA group. Finally, the LMA group had fewer episodes of emergence cough, compared with the ETT group.
Conclusion
The LMA Protector™ causes fewer pharyngolaryngeal symptoms than the ETT within 6 and 12 h after minimally invasive total thyroidectomy and parathyroidectomy.
Trial registration
ClinicalTrials.gov Identifier NCT03098667.
Similar content being viewed by others
Introduction
Postoperative pharyngolaryngeal symptoms, particularly postoperative pharyngodynia (sore throat), are a common concern after general anesthesia [1,2,3,4]. These symptoms may constitute discomfort, but can potentially cause hoarseness, dysphagia, laryngitis, bronchitis, and respiratory distress [4]. Manipulations during laryngoscopy and intubation, as well as the presence of the endotracheal tube (ETT) itself, can irritate the larynx, pharynx, and trachea; such events contribute to the pathophysiology of postoperative pharyngolaryngeal symptoms [3], which cause physical stress, patient dissatisfaction, and delayed recovery [5].
Thyroidectomy is a type of surgery with a high rate of pharyngodynia [5], likely due to surgical manipulations of the head, neck, trachea, and thyroid gland, as well as tissues close to the larynx and pharynx [3]. Surgical site pain after thyroidectomy is typically not expected to be significant, particularly when the minimally invasive technique is applied; this comprises a small incision and no surgical site drainage [6,7,8,9]. Therefore, pharyngolaryngeal symptoms are likely to comprise the main source of post-thyroidectomy discomfort.
Laryngeal mask airway (LMA) is currently used as an alternative for airway management during thyroidectomy [10,11,12]. The Protector™ (Teleflex Medical Europe Ltd., Westmeath, Ireland) LMA is a second-generation supraglottic airway device (SAD) with a built-in cuff pressure indicator, which ensures filling of the air chamber of the mask with the appropriate volume of air. We hypothesized that the Protector™ LMA would cause fewer pharyngolaryngeal symptoms, compared with the ETT, after minimally invasive thyroid and parathyroid surgery.
Materials and methods
This prospective, single-blind, randomized, controlled trial included patients who were 18–80 years of age, had American Society of Anesthesiologists status 1–3, and were scheduled for thyroid and parathyroid surgery at the AHEPA University Hospital of Thessaloniki and the Interbalkan Medical Center of Thessaloniki during a six-month period between February 2017 and November 2017. After acquiring approval from the scientific board of AHEPA University Hospital of Thessaloniki (No 185; March 15, 2017), the patients who signed the written consent formed after thorough explanation of the purposes of the study were randomly allocated to 2 groups by computer software (https://www.randomizer.org/): LMA and ETT. Patients were excluded if they had clinical conditions that caused any type of airway obstruction or compromise; tracheal displacement >2 cm from midline; history of gastroesophageal reflux disease; a potentially difficult airway; a history of impossible intubation; substitution of the LMA with an ETT due to inadequate ventilation; duration of surgery >3 h; body mass index (BMI) >35; or reoperation within 24 h.
After preoxygenation with 100% O2 for 2 min via face mask, general anesthesia was induced with 3 μg/kg fentanyl and 2 mg/kg propofol for patients in both groups, followed by 0.6 mg/kg rocuronium only for patients in the ETT group. Endotracheal intubation was performed for patients in the ETT group; the sizes of the laryngoscope blade and ETT were chosen by the attending anesthetist. The cuff of the ETT was gradually filled until there was no air leak from the trachea. For patients in the LMA group, the LMA Protector™ was used for airway management. The size of the mask was chosen in accordance with the manufacturer’s instructions. A lubricant gel was applied at the posterior surface of the mask, and the air chamber was filled in accordance with the indication of the pilot cuff. If inadequate ventilation occurred before or during the surgery, the LMA was removed and replaced with an ETT. The ventilator was set in volume-controlled mode for all patients, and settings were modified by the attending anesthetist.
Anesthesia was maintained with sevoflurane and remifentanil infusion. Remifentanil was administered by a target-controlled infusion (TCI) pump with a target plasma concentration of 3.5 ng/ml during surgery and 3 ng/ml during extubation. Alterations during surgery were done by the attending anesthesiologist according to the hemodynamic status of each patient. All the patients were administered 4 mg dexamethasone, 4 mg ondansetron, 1000 mg paracetamol, and 8 mg lornoxicam. All the patients were operated by the same surgical team. After surgery was completed, sevoflurane and remifentanil infusion was discontinued; after emergence from general anesthesia, the ETT or LMA was removed. Postoperatively, 8 mg lornoxicam was administered every 12 h; patients were instructed to request supplementary analgesia (1000 mg paracetamol) as needed. The patients were given liquids at 2 h upon arrival to the ward and solid food within 6 h and were discharged within 24 h from the end of surgery.
The main outcomes of this study were intensity of postoperative pharyngodynia, dysphagia (pain after swallowing 1 sip of water), and surgical site pain. These parameters were evaluated by patients within 20 min from the end of surgery, as well as at 1, 6, 12, and 24 h after surgery, by using the 11-point (0 = no pain, 10 = maximum possible pain) numerical rating scale. Documentation was done by the shift nurse of the ward who was unaware of the purpose and methodology of the study. Secondary outcomes were rate of emergence cough (recorded by the attending anesthesiologist) and rate of postoperative paracetamol consumption.
The following parameters were also recorded: age, sex, weight, height, duration of surgery, and type of surgery (thyroid or parathyroid surgery). For statistical analysis, the Mann–Whitney test was used to compare scores between the groups (notably, the data did not exhibit a normal distribution); the Chi-squared and Fisher’s exact test were used to compare rates. All tests were performed using SPSS 23.0 software (IBM Corp., Armonk, NY, USA). Sample size was calculated with G*Power 3.1 software (Heinrich-Heine-Universität, Düsseldorf, Germany). The mean and standard deviation of pharyngodynia score at 1 h after surgery in a 20-patient pilot study (n = 10 patients per group) were used for power calculations; for p = 0.05 and power = 0.8, a minimum of 35 patients in each group were required.
Results
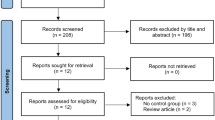
A total of 91 patients were enrolled in the study, and data from 78 were finally analyzed. The flowchart of the study is shown in Fig. 1. No differences were found between the groups in age, sex, BMI, or duration of surgery (Table 1). Primary outcomes of the study are shown in Table 2 and Figs. 2, 3, 4. Pharyngodynia scores were significantly lower in the LMA group, compared with the ETT group, at 1 h (2.7 vs. 3.8), 6 h (2 vs. 3.7), and 12 h (1.6 vs. 3.2) after surgery. Dysphagia and surgical incision pain scores were also significantly lower in the LMA group, compared with the ETT group, at 6 h (2.8 vs. 4.2; 1.9 vs. 3) and 12 h (2.4 vs. 3.7; 1.5 vs. 2.7) after surgery. Secondary outcomes are shown in Table 1. The frequencies of additional analgesia consumption (46.3 vs. 15.8%, p = 0.013) and emergence cough (31.7 vs. 7.9%, p = 0.008) were significantly greater in the ETT group than in the LMA group (Fig. 5). No differences were found in any other parameters of the study.
Discussion
The results of this study show that the use of the LMA Protector™ for airway management in patients undergoing minimally invasive thyroid and parathyroid surgery has advantages over use of the ETT, regarding postoperative pharyngolaryngeal symptoms. The subjective feeling of pharyngeal discomfort (pharyngodynia) was reportedly less intense for patients ventilated via LMA within the first 12 h after surgery. The sense of pain after swallowing (dysphagia) was also reduced in these patients within the same time period, as was the frequency of supplemental analgesia for any type of pain or discomfort. These findings are important for minimally invasive neck surgery, because pharyngolaryngeal symptoms are expected to be the main source of postoperative discomfort; in this type of surgery, surgical incision pain is expected to be minimal [6, 9, 13]. Notably, in our study, incisional pain was also reduced for patients in the LMA group. Finally, the frequency of emergence cough, following general anesthesia, was significantly lower in the LMA group. Possible detrimental effects of emergence cough (e.g., laryngospasm; cardiovascular compromise; and increased intraocular, intracranial, and intrathoracic pressures) [14] might increase the possibility of venous bleeding [15]; however, our study was likely underpowered to determine the superiority of LMA regarding emergence cough. The results of our study are consistent with the results of similar studies, which also favored LMA usage over ETT usage for thyroid surgery [16, 17].
Pharyngodynia is a common problem after general anesthesia [4]. The incidence of pharyngeal discomfort appears to be significantly higher after thyroidectomy, compared with other types of surgery [18,19,20]. Irritation of the local mucosa by the ETT, as well as laryngeal edema and vocal cord trauma, is the probable cause of pharyngodynia; these may work in combination with movement of the ETT during surgical manipulations of the thyroid gland and adjacent tissues [18]. The use of smaller ETTs with high-volume, low-pressure cuffs, as well as careful control of intracuff pressure and avoidance of lubricants containing local anesthetics, is the measure proposed to reduce pharyngodynia [4]. The use of gabapentin [2] and dexamethasone [3] has also proven to be beneficial.
LMA usage is generally associated with reduced incidences of hoarseness and airway complications during and after general anesthesia [21], compared with ETT usage; however, a recent meta-analysis failed to find any differences in the occurrence of pharyngodynia [22]. LMA usage is not very popular in neck surgery, due to the possibility of displacement after neck extension and surgical manipulations of the trachea, as well as the inconvenience caused by limited access to the airway if adjustments of LMA position are needed during surgery [16]. ETT usage remains the typical practice for major neck surgeries [10]. However, LMA, in combination with a fiberoptic bronchoscope, has been successfully used for intraoperative monitoring of recurrent laryngeal [23,24,25,26,27,28,29,30] and superior laryngeal [31] nerve function.
The LMA Protector™ is a new single-use SAD. It is latex-free and does not require a special introducer for insertion; moreover, a built-in bite-block prevents damage from accidental biting. Similar to other LMAs, it enables intubation of the patient through the lumen of the mask, either blindly or with the aid of a fiberoptic bronchoscope [32]. An advantage of the LMA Protector™ over other second-generation SADs is that it provides a very high pharyngeal seal, which is unaffected by extension of the patient’s neck [33]. In our study, we encountered only 1 instance of inadequate ventilation during surgery. Because of hypercapnia (PCO2 > 50 mmHg), the LMA was removed and an ETT was placed; the patient was excluded from the study. All other patients in the LMA group were ventilated uneventfully, and no neuromuscular blocking agents were needed. Another advantage of the LMA Protector™ is that it has two separate drain channels; one channel can be used to suction gastric contents from the laryngeal area, if regurgitation occurs, while the other channel can be used to insert a tube inside the stomach [32]. Finally, the LMA Protector™ devices used in our study had built-in cuff pressure indicators; this feature ensures that the minimum pressure required to achieve an adequate seal will be applied to the supraglottic area. Recent studies have shown that the use of manometry with LMA devices reduces postoperative pharyngolaryngeal symptoms [34,35,36,37]. This may be why the LMA Protector™ was superior to the ETT in our study, and the incidence of emergence cough was significantly lower for LMA patients.
Our study had some limitations. First, it was not double-blinded. The main outcomes were self-reported by patients, none of whom were aware of the device used for airway management; however, anesthetists in the operating theater were not (and could not be) blinded to the device, so bias could not be excluded. Second, the intracuff pressure of the air chamber was solely measured for the LMA group (using the built-in indicator), and not for the ETT group as it is not a common everyday practice and the appropriate device is not available in the anesthetic departments of the participating hospitals. We believed that we minimized the possibility of overinflating the cuff by gradually filling (initially 5 ml of air and then increments of 1 ml) the cuff until no air leak was achieved. Moreover, the size of the ETT was not recorded; however, the typical practice of the department is to use size 7.5 for women and 8.5 for men. Third, the study did not include measurement of the total dose of remifentanil administered to each patient. The remifentanil infusion was standardized with the TCI pump and the goal was to achieve the same plasma concentration for all the patients during surgery and extubation; however, the total amount of remifentanil administered during surgery might affect postoperative discomfort, as well as the incidence of emergence cough. Fourth, the size of the thyroid gland was not recorded. Removal of a large thyroid might require a more vigorous operation, which may be followed by more severe postoperative symptoms; however, such thyroidectomies are not typically performed using a minimally invasive technique.
Conclusion
The LMA Protector™ causes lower levels of pharyngolaryngeal discomfort, compared with the ETT, after minimally invasive total thyroidectomy or parathyroidectomy. It also appears to reduce the incidence of emergence cough; however, studies designed to specifically investigate this effect are needed to reach reliable conclusions. Anesthetists should consider the LMA Protector™ as an alternative to the ETT in thyroid and parathyroid surgeries.
References
Higgins PP, Chung F, Mezei G (2002) Postoperative sore throat after ambulatory surgery. Br J Anaesth 88:582–584
Lee JH, Lee HK, Chun NH et al (2013) The prophylactic effects of gabapentin on postoperative sore throat after thyroid surgery. Korean J Anesthesiol 64:138–142
Yang C, Jung SM, Bae YK, Park S-J (2017) The effect of ketorolac and dexamethasone on the incidence of sore throat in women after thyroidectomy: a prospective double-blinded randomized trial. Korean J Anesthesiol 70:64–71
McHardy FE, Chung F (1999) Postoperative sore throat: cause, prevention and treatment. Anaesthesia 54:444–453
Jung TH, Rho J-H, Hwang JH et al (2011) The effect of the humidifier on sore throat and cough after thyroidectomy. Korean J Anesthesiol 61:470
Papavramidis TS, Michalopoulos N, Pliakos J et al (2010) Minimally invasive video-assisted total thyroidectomy: an easy to learn technique for skillful surgeons. Head Neck 32:1370–1376
Miccoli P, Bellantone R, Mourad M et al (2002) Minimally invasive video-assisted thyroidectomy: multiinstitutional experience. World J Surg 26:972–975. https://doi.org/10.1007/s00268-002-6627-7
Govednik CM, Snyder SK, Quinn CE et al (2014) Minimally invasive, nonendoscopic thyroidectomy: a cosmetic alternative to robotic-assisted thyroidectomy. Surgery 156:1030–1037
Soo Park C, Youn Chung W, Seok Chang H (2001) Minimally invasive open thyroidectomy. Surg Today 31:665–669
Jefferson N, Riffat F, McGuinness J, Johnstone C (2011) The laryngeal mask airway and otorhinolaryngology head and neck surgery. Laryngoscope 121:1620–1626
Martin-Castro C, Montero A (2008) Flexible laryngeal mask as an alternative to reinforced tracheal tube for upper chest, head and neck oncoplastic surgery. Eur J Anaesthesiol 25:261–266
Gong Y, Wang J, Xu X et al (2018) Performance of air seal of flexible reinforced laryngeal mask airway in thyroid surgery compared with endotracheal tube. Anesth Analg. https://doi.org/10.1213/ANE.0000000000003763
Sabuncuoglu MZ, Sabuncuoglu A, Sozen I et al (2014) Minimally invasive surgery using mini anterior incision for thyroid diseases: a prospective cohort study. Int J Clin Exp Med 7:3404–3409
Hans P, Marechal H, Bonhomme V (2008) Effect of propofol and sevoflurane on coughing in smokers and non-smokers awakening from general anaesthesia at the end of a cervical spine surgery. Br J Anaesth 101:731–737
Kim ES, Bishop MJ (1998) Cough during emergence from isoflurane anesthesia. Anesth Analg 87:1170–1174
Ryu J-H, Yom C-K, Park D-J et al (2014) Prospective randomized controlled trial on the use of flexible reinforced laryngeal mask airway (LMA) during total thyroidectomy: effects on postoperative laryngopharyngeal symptoms. World J Surg 38:378–384. https://doi.org/10.1007/s00268-013-2269-1
Chun B-J, Bae J-S, Lee S-H et al (2015) A prospective randomized controlled trial of the laryngeal mask airway versus the endotracheal intubation in the thyroid surgery: evaluation of postoperative voice, and laryngopharyngeal symptom. World J Surg 39:1713–1720. https://doi.org/10.1007/s00268-015-2995-7
Hisham AN, Roshilla H, Amri N, Aina EN (2001) Post-thyroidectomy sore throat following endotracheal intubation. ANZ J Surg 71:669–671
Sanou J, Ilboudo D, Rouamba A, Traore O (1996) Sore throat after tracheal intubation. Cah Anesthesiol 44:203–206
Christensen AM, Willemoes-Larsen H, Lundby L, Jakobsen KB (1994) Postoperative throat complaints after tracheal intubation. Br J Anaesth 73:786–787
Yu SH, Beirne OR (2010) Laryngeal mask airways have a lower risk of airway complications compared with endotracheal intubation: a systematic review. J Oral Maxillofac Surg 68:2359–2376
Xu R, Lian Y, Li WX (2016) Airway complications during and after general anesthesia: a comparison, systematic review and meta-analysis of using flexible laryngeal mask airways and endotracheal tubes. PLoS ONE 11:e0158137
Shah EF, Allen JG, Greatorex RA (2001) Use of the laryngeal mask airway in thyroid and parathyroid surgery as an aid to the identification and preservation of the recurrent laryngeal nerves. Ann R Coll Surg Engl 83:315–318
Dingle AF (2002) Use of the laryngeal mask airway in thyroid and parathyroid surgery as an aid in identification and preservation of the recurrent laryngeal nerves. Ann R Coll Surg Engl 84:147 (author reply 148)
Charters P, Cave-Bigley D (1992) Application of the laryngeal mask airway to thyroid surgery and the preservation of the recurrent laryngeal nerve. Ann. R. Coll. Surg. Engl. 74:225–226
Pott L, Swick JT, Stack BCJ (2007) Assessment of recurrent laryngeal nerve during thyroid surgery with laryngeal mask airway. Arch Otolaryngol Head Neck Surg 133:266–269
Akhtar TM (1991) Laryngeal mask airway and visualisation of vocal cords during thyroid surgery. Can J Anaesth 38:140
Rosswick P (2002) Use of the laryngeal mask airway in thyroid and parathyroid surgery as an aid in identification and preservation of the recurrent laryngeal nerves. Ann R Coll Surg Engl 84:148 (author reply 148)
Premachandra DJ (1992) Application of the laryngeal mask airway to thyroid surgery and the preservation of the recurrent laryngeal nerve. Ann R Coll Surg Engl 74:226
Eltzschig HK, Posner M, Moore FD (2002) The use of readily available equipment in a simple method for intraoperative monitoring of recurrent laryngeal nerve function during thyroid surgery: initial experience with more than 300 cases. Arch Surg 137:452–456 (discussion 456–457)
Brimacombe J, Knott J, Keller C (2003) Laryngeal mask airway for preservation of the external branch of the superior laryngeal nerve during thyroid surgery. Can J Anaesth 50:858
Sng BL, Ithnin FB, Mathur D et al (2017) A preliminary assessment of the LMA protector™ in non-paralysed patients. BMC Anesthesiol 17:26
Eckardt F, Engel J, Tw Mann S et al (2018) LMA® ProtectorTM Airway. First experience with a new second generation laryngeal mask. Minerva Anestesiol 85:45–52
Seet E, Yousaf F, Gupta S et al (2010) Use of manometry for laryngeal mask airway reduces postoperative pharyngolaryngeal adverse events. Anesthesiology 112:652–657
Brimacombe J, Holyoake L, Keller C et al (2000) Pharyngolaryngeal, neck, and jaw discomfort after anesthesia with the face mask and laryngeal mask airway at high and low cuff volumes in males and females. Anesthesiology 93:26–31
Chantzara G, Stroumpoulis K, Alexandrou N et al (2014) Influence of LMA cuff pressure on the incidence of pharyngolaryngeal adverse effects and evaluation of the use of manometry during different ventilation modes: a randomized clinical trial. Minerva Anestesiol 80:547–555
Wong DT, Tam AD, Mehta V et al (2013) New supraglottic airway with built-in pressure indicator decreases postoperative pharyngolaryngeal symptoms: a randomized controlled trial. Can J Anesth Can d’anesthésie 60:1197–1203
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors delcare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kotsovolis, G., Pliakos, I., Panidis, S. et al. Comparison Between the Protector™ Laryngeal Mask Airway and the Endotracheal Tube for Minimally Invasive Thyroid and Parathyroid Surgery. World J Surg 43, 2822–2828 (2019). https://doi.org/10.1007/s00268-019-05122-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05122-8