Abstract
Objective
One of the presumed advantages of prophylactic central neck dissection (pCND) is offering staging basis for more aggressive radioactive iodine (RAI) therapy, which postulates the necessity of high dose for treatment efficacy. The present study aims to compare the effectiveness between low-dose and high-dose RAI in a select cohort of cN0 papillary thyroid cancer (PTC) patients with pathological N1a (pN1a) disease revealed by pCND in terms of ablation rate and response to therapy. The frequency of short-term adverse effects between the two groups was also compared.
Patients and Methods
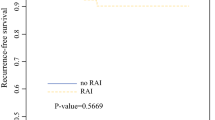
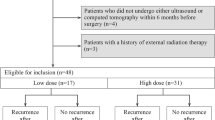
From January 2014 to April 2016, cN0 PTC patients with pN1a disease revealed by pCND in our hospital were retrospectively reviewed. Patients with other indications for high-dose RAI, such as the presence of extrathyroidal extension, vascular invasion or suspicions of distant metastasis, were excluded. For the included patients, high dose (3700 MBq) was administered between January 2014 and August 2015 and low dose (1110 MBq) between August 2015 and April 2016. Ablation assessment was performed 6 months after RAI therapy. Response evaluation after RAI therapy was performed after 46.3 ± 9.5 months for high-dose group and 29.1 ± 2.6 months for low-dose group. All patients were also evaluated for short-term adverse effects 24 and 72 hours after RAI administration.
Results
A total of 84 patients were enrolled. Among them, 42 were in the high-dose group and the other 42 in the low-dose group. There was no significant difference in ablation rate (P = 0.7707) and response to RAI therapy (P = 0.6454) between the two groups. Twenty-four hours after RAI administration, neck pain and swelling (33.3% VS. 11.9%; P = 0.0372) and gastrointestinal discomfort (45.2% vs. 21.4%; P = 0.0373) were significantly more frequent in the high-dose group.
Conclusion
High-dose RAI therapy, with higher frequency of short-term adverse effects, appears to be not superior to low-dose RAI therapy for cN0 PTC patients with pN1a disease revealed by pCND to achieve better response to therapy. Further randomized studies with larger series of patients and longer follow-up duration, especially with the low-dose group, are needed to validate our results.

Similar content being viewed by others
References
Carty SE, Cooper DS, Doherty GM et al (2009) Consensus statement on the terminology and classification of central neck dissection for thyroid cancer. Thyroid. 19(11):1153–1158. https://doi.org/10.1089/thy.2009.0159
Randolph GW, Duh QY, Heller KS et al (2012) The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid. 22(11):1144–1152. https://doi.org/10.1089/thy.2012.0043
Hughes DT, Rosen JE, Evans DB, Grubbs E, Wang TS, Solorzano CC (2018) Prophylactic Central Compartment Neck Dissection in Papillary Thyroid Cancer and Effect on Locoregional Recurrence. Ann Surg Oncol. 25(9):2526–2534. https://doi.org/10.1245/s10434-018-6528-0
Sitges-Serra A, Lorente L, Mateu G, Sancho JJ (2015) THERAPY OF ENDOCRINE DISEASE: Central neck dissection: a step forward in the treatment of papillary thyroid cancer. Eur J Endocrinol. 173(6):R199–R206. https://doi.org/10.1530/eje-15-0481
Bardet S, Ciappuccini R, Quak E et al (2015) Prognostic value of microscopic lymph node involvement in patients with papillary thyroid cancer. J Clin Endocrinol Metab. 100(1):132–140. https://doi.org/10.1210/jc.2014-1199
Hartl DM, Leboulleux S, Al Ghuzlan A et al (2012) Optimization of staging of the neck with prophylactic central and lateral neck dissection for papillary thyroid carcinoma. Ann Surg. 255(4):777–783. https://doi.org/10.1097/SLA.0b013e31824b7b68
Lin B, Qiang W, Wenqi Z, Tianyu Y, Lina Z, Bin J (2017) Clinical response to radioactive iodine therapy for prophylactic central neck dissection is not superior to total thyroidectomy alone in cN0 patients with papillary thyroid cancer. Nucl Med Commun. 38(12):1036–1040. https://doi.org/10.1097/mnm.0000000000000756
Haugen BR, Alexander EK, Bible KC et al (2016) 2015 American Thyroid Association Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association Guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 26(1):1–133. https://doi.org/10.1089/thy.2015.0020
Cooper DS, Doherty GM, Haugen BR et al (2009) Revised American Thyroid Association Management Guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 19(11):1167–1214. https://doi.org/10.1089/thy.2009.0110
Pashnehsaz M, Takavar A, Izadyar S et al (2016) Gastrointestinal Side Effects of the Radioiodine Therapy for the Patients with Differentiated Thyroid Carcinoma Two Days after Prescription. World J Nucl Med. 15(3):173–178. https://doi.org/10.4103/1450-1147.174703
Silva-Vieira M, Carrilho Vaz S, Esteves S et al (2017) Second Primary Cancer in Patients with Differentiated Thyroid Cancer: does radioiodine Play a Role? Thyroid. 27(8):1068–1076. https://doi.org/10.1089/thy.2016.0655
Valachis A, Nearchou A (2013) High versus low radioiodine activity in patients with differentiated thyroid cancer: a meta-analysis. Acta Oncol. 52(6):1055–1061. https://doi.org/10.3109/0284186x.2012.742959
Castagna MG, Cevenini G, Theodoropoulou A et al (2013) Post-surgical thyroid ablation with low or high radioiodine activities results in similar outcomes in intermediate risk differentiated thyroid cancer patients. Eur J Endocrinol. 169(1):23–29. https://doi.org/10.1530/eje-12-0954
Ma C, Feng F, Wang S et al (2017) Chinese Data of Efficacy of Low- and High-Dose Iodine-131 for the Ablation of Thyroid Remnant. Thyroid. 27(6):832–837. https://doi.org/10.1089/thy.2015.0658
Schlumberger M, Catargi B, Borget I et al (2012) Strategies of radioiodine ablation in patients with low-risk thyroid cancer. N Engl J Med. 366(18):1663–1673. https://doi.org/10.1056/NEJMoa1108586
Wang C, Zhao T, Li H, Gao W, Lin Y (2017) Low activity versus high activity: noninferior response to radioiodine therapy in differentiated patients with extrathyroid extension. Nucl Med Commun. 38(5):366–371. https://doi.org/10.1097/mnm.0000000000000666
Kim SK, Woo JW, Lee JH et al (2016) Prophylactic Central Neck Dissection Might Not Be Necessary in Papillary Thyroid Carcinoma: Analysis of 11,569 Cases from a Single Institution. J Am Coll Surg. 222(5):853–864. https://doi.org/10.1016/j.jamcollsurg.2016.02.001
Liu J, Xu Z, Li Z, Zhang Z, Tang P, Liu S (2015) Long-term outcomes of observation for clinically negative central compartment lymph nodes in papillary thyroid carcinoma. Eur Arch Otorhinolaryngol. 272(12):3801–3804. https://doi.org/10.1007/s00405-014-3453-0
Chereau N, Buffet C, Tresallet C, Tissier F, Leenhardt L, Menegaux F (2016) Recurrence of papillary thyroid carcinoma with lateral cervical node metastases: Predictive factors and operative management. Surgery. 159(3):755–762. https://doi.org/10.1016/j.surg.2015.08.033
Jeon MJ, Yoon JH, Han JM et al (2013) The prognostic value of the metastatic lymph node ratio and maximal metastatic tumor size in pathological N1a papillary thyroid carcinoma. Eur J Endocrinol. 168(2):219–225. https://doi.org/10.1530/eje-12-0744
Leboulleux S, Rubino C, Baudin E et al (2005) Prognostic factors for persistent or recurrent disease of papillary thyroid carcinoma with neck lymph node metastases and/or tumor extension beyond the thyroid capsule at initial diagnosis. J Clin Endocrinol Metab. 90(10):5723–5729. https://doi.org/10.1210/jc.2005-0285
Ryu IS, Song CI, Choi SH, Roh JL, Nam SY, Kim SY (2014) Lymph node ratio of the central compartment is a significant predictor for locoregional recurrence after prophylactic central neck dissection in patients with thyroid papillary carcinoma. Ann Surg Oncol. 21(1):277–283. https://doi.org/10.1245/s10434-013-3258-1
Zheng CM, Ji YB, Song CM, Ge MH, Tae K (2018) Number of Metastatic Lymph Nodes and Ratio of Metastatic Lymph Nodes to Total Number of Retrieved Lymph Nodes Are Risk Factors for Recurrence in Patients With Clinically Node Negative Papillary Thyroid Carcinoma. Clin Exp Otorhinolaryngol. 11(1):58–64. https://doi.org/10.21053/ceo.2017.00472
Acknowledgements
This work was supported by the Young Researcher Fund of Science and Technology Department of Jilin Province (Grant number: 20170520027JH) and the Norman Bethune Youth Program of Jilin University (Grant number: 2015219).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The author declares that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wei, L., Bai, L., Zhao, L. et al. High-Dose RAI Therapy Justified by Pathological N1a Disease Revealed by Prophylactic Central Neck Dissection for cN0 Papillary Thyroid Cancer Patients: Is it Superior to Low-Dose RAI Therapy?. World J Surg 43, 1256–1263 (2019). https://doi.org/10.1007/s00268-019-04924-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-04924-0