Abstract
Background
The concept of intraductal papillary neoplasm of the bile duct (IPNB) has been proposed to be the biliary equivalent of intraductal papillary mucinous neoplasm (IPMN) of the pancreas. While the classification of IPMNs is based on their location of duct involvement, such classification has not been fully evaluated for IPNBs. The aim of this study is to investigate the value of IPNB classification based on its location.
Methods
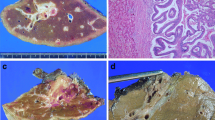
A total of 306 consecutive patients who underwent surgical resection with a diagnosis of bile duct tumor were enrolled. Among these patients, 21 were diagnosed as having IPNB. The IPNBs were classified into two groups as follows: extrahepatic IPNB, which located in the distal or perihilar bile duct, and intrahepatic IPNB, which located more peripherally than the hilar bile duct. The clinicopathological features of the two groups were then compared.
Results
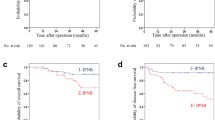
Extrahepatic IPNB tended to show more invasive characteristics than intrahepatic IPNB (presence of invasive component: 40.0 vs. 9.1%, p = 0.084). Moreover, patients with extrahepatic IPNB showed significantly poorer relapse-free survival (RFS) than those with intrahepatic IPNB [5-year RFS rate (%): 81.8 vs. 16.2, p = 0.014].
Conclusion
Patients with intrahepatic IPNB show more favorable pathological characteristics and postoperative survival outcomes than those with extrahepatic IPNB.

Similar content being viewed by others
Abbreviations
- Alb:
-
Albumin
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- CA19-9:
-
Carbohydrate antigen 19-9
- CEA:
-
Carcinoembryonic antigen
- CRP:
-
C-reactive protein
- γ-GTP:
-
Gamma-glutamyltransferase
- IPMN-P:
-
Intraductal papillary mucinous neoplasm of the pancreas
- IPNB:
-
Intraductal papillary neoplasm of the bile duct
- PLT:
-
Platelet
- TP:
-
Total protein
- WHO:
-
World Health Organization
References
Bosman FT (2010) World Health Organization., international agency for research on cancer. WHO classification of tumours of the digestive system. Lyon, International agency for research on cancer
Chen TC, Nakanuma Y, Zen Y et al (2001) Intraductal papillary neoplasia of the liver associated with hepatolithiasis. Hepatology 34:651–658
Ohtsuka M, Shimizu H, Kato A et al (2014) Intraductal papillary neoplasms of the bile duct. Int J Hepatol 2014:10
Nakanuma Y, Sato Y, Ojima H et al (2014) Clinicopathological characterization of so-called “cholangiocarcinoma with intraductal papillary growth” with respect to “intraductal papillary neoplasm of bile duct (IPNB)”. Int J Clin Exp Pathol 7:3112–3122
Nakanuma Y, Kakuda Y, Uesaka K et al (2016) Characterization of intraductal papillary neoplasm of bile duct with respect to histopathologic similarities to pancreatic intraductal papillary mucinous neoplasm. Hum Pathol 51:103–113
Fujikura K, Fukumoto T, Ajiki T et al (2016) Comparative clinicopathological study of biliary intraductal papillary neoplasms and papillary cholangiocarcinomas. Histopathology 69(6):950–961
Adsay V, Mino-Kenudson M, Furukawa T et al (2016) Pathologic evaluation and reporting of intraductal papillary mucinous neoplasms of the pancreas and other tumoral intraepithelial neoplasms of pancreatobiliary tract: recommendations of verona consensus meeting. Ann Surg 263:162–177
Ji Y, Fan J, Zhou J et al (2008) Intraductal papillary neoplasms of bile duct. A distinct entity like its counterpart in pancreas. Histol Histopathol 23:41–50
Rocha FG, Lee H, Katabi N et al (2012) Intraductal papillary neoplasm of the bile duct: a biliary equivalent to intraductal papillary mucinous neoplasm of the pancreas? Hepatology 56:1352–1360
Koh Y-X, Chok A-Y, Zheng H-L et al (2014) Systematic review and meta-analysis comparing the surgical outcomes of invasive intraductal papillary mucinous neoplasms and conventional pancreatic ductal adenocarcinoma. Ann Surg Oncol 21:2782–2800
Salvia R, Castillo CF, Bassi C et al (2004) Main-duct intraductal papillary mucinous neoplasms of the pancreas: clinical predictors of malignancy and long-term survival following resection. Ann Surg 239:678–687
Miyazaki M, Ohtsuka M, Miyakawa S et al (2015) Classification of biliary tract cancers established by the Japanese Society of Hepato-Biliary-Pancreatic Surgery: 3rd English edition. J Hepatobiliary Pancreat Sci 22:181–196
Union for International Cancer Control (UICC) TNM Classification of Malignant Tumors, Wiley Blackwell, New Jersey
Kim KM, Lee JK, Shin JU et al (2012) Clinicopathologic features of intraductal papillary neoplasm of the bile duct according to histologic subtype. Am J Gastroenterol 107:118–125
Wan X-S, Xu Y-Y, Qian J-Y et al (2013) Intraductal papillary neoplasm of the bile duct. World J Gastroenterol 19:8595–8604
Deutsch G, Jung J, Zheng M et al (2001) A bipotential precursor population for pancreas and liver within the embryonic endoderm. Development 128:871–881
Bennett S, Marginean EC, Paquin-Gobeil M et al (2015) Clinical and pathological features of intraductal papillary neoplasm of the biliary tract and gallbladder. HPB 17(9):811–818
Nakanuma Y (2010) A novel approach to biliary tract pathology based on similarities to pancreatic counterparts: is the biliary tract an incomplete pancreas? Pathol Int 60:419–429
Minagawa N, Sato N, Mori Y et al (2013) A comparison between intraductal papillary neoplasms of the biliary tract (BT-IPMNs) and intraductal papillary mucinous neoplasms of the pancreas (P-IPMNs) reveals distinct clinical manifestations and outcomes. Eur J Surg Oncol 39:554–558
Zen Y, Fujii T, Itatsu K et al (2006) Biliary papillary tumors share pathological features with intraductal papillary mucinous neoplasm of the pancreas. Hepatology 44:1333–1343
Suh KS, Roh HR, Koh YT et al (2000) Clinicopathologic features of the intraductal growth type of peripheral cholangiocarcinoma. Hepatology 31:12–17
Fong Y, Blumgart LH (2000) Surgery of the liver and biliary tract. WB Saunders, Philadelphia
Salvia R, Fernandez-del Castillo C, Bassi C et al (2004) Main-duct intraductal papillary mucinous neoplasms of the pancreas: clinical predictors of malignancy and long-term survival following resection. Ann Surg 239:678–685 discussion 685–677
Kubota K, Nakanuma Y, Kondo F et al (2014) Clinicopathological features and prognosis of mucin-producing bile duct tumor and mucinous cystic tumor of the liver: a multi-institutional study by the Japan biliary association. J Hepatobiliary Pancreat Sci 21:176–185
Gordon-Weeks AN, Jones K, Harriss E et al (2016) Systematic review and meta-analysis of current experience in treating IPNB: clinical and pathological correlates. Ann Surg 263:656–663
Vibert E, Dokmak S (2010) Belghiti J Surgical strategy of biliary papillomatosis in Western countries. J Hepatobiliary Pancreat Sci 17:241–245
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest to declare.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Matsumoto, T., Kubota, K., Hachiya, H. et al. Impact of Tumor Location on Postoperative Outcome of Intraductal Papillary Neoplasm of the Bile Duct. World J Surg 43, 1313–1322 (2019). https://doi.org/10.1007/s00268-019-04913-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-04913-3