Abstract
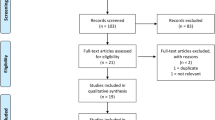
The most troublesome complications of inguinal hernia repair are recurrent herniation and chronic pain. A multitude of technological products dedicated to abdominal wall surgery, such as self-gripping mesh (SGM) and glue fixation (GF), were introduced in alternative to suture fixation (SF) in the attempt to lower the postoperative complication rates. We conducted an electronic systematic search using MEDLINE databases that compared postoperative pain and short- and long-term surgical complications after SGM or GF and SF in open inguinal hernia repair. Twenty-eight randomized controlled trials totaling 5495 patients met the inclusion criteria and were included in this network meta-analysis. SGM and GF did not show better outcomes in either short- or long-term complications compared to SF. Patients in the SGM group showed significantly more pain at day 1 compared to those in the GF group (VAS score pain mean difference: − 5.2 Crl − 11.0; − 1.2). The relative risk (RR) of developing a surgical site infection (RR 0.83; Crl 0.50–1.32), hematoma (RR 1.9; Crl 0.35–11.2), and seroma (RR 1.81; Crl 0.54–6.53) was similar in SGM and GF groups. Both the SGM and GF had a significantly shorter operative time mean difference (1.70; Crl − 1.80; 5.3) compared to SF. Chronic pain and hernia recurrence did not statistically differ at 1 year (RR 0.63; Crl 0.36–1.12; RR 1.5; Crl 0.52–4.71, respectively) between SGM and GF. Methods of inguinal hernia repair are evolving, but there remains no superiority in terms of mesh fixation. Ultimately, patient’s preference and surgeon’s expertise should still lead the choice about the fixation method.







Similar content being viewed by others
References
Lichtenstein IL, Shulman AG (1986) Ambulatory outpatient hernia surgery. Including a new concept, introducing tension-free repair. Int Surg 71:1–4
Magnusson J, Gustafsson UO, Nygren J, et al (2018) Rates of and methods used at reoperation for recurrence after primary inguinal hernia repair with Prolene Hernia System and Lichtenstein. Hernia 22:439–444. https://doi.org/10.1007/s10029-017-1705-9
Charalambous MP, Charalambous CP (2018) Incidence of chronic groin pain following open mesh inguinal hernia repair, and effect of elective division of the ilioinguinal nerve: meta-analysis of randomized controlled trials. Hernia 22:401–409. https://doi.org/10.1007/s10029-018-1753-9
Pandanaboyana S, Mittapalli D, Rao A et al (2014) Meta-analysis of self-gripping mesh (Progrip) versus sutured mesh in open inguinal hernia repair. Surgeon 12:87–93
Fang Z, Zhou J, Ren F et al (2014) Self-gripping mesh versus sutured mesh in open inguinal hernia repair: system review and meta-analysis. Am J Surg 207:773–781
Sun P, Cheng X, Deng S et al (2017) Mesh fixation with glue versus suture for chronic pain and recurrence in Lichtenstein inguinal hernioplasty. Cochrane Database Syst Rev 2:Cd010814
Lichtenstein IL, Shulman AG, Amid PK et al (1989) The tension-free hernioplasty. Am J Surg 157:188–193
Ronka K, Vironen J, Kossi J et al (2015) Randomized multicenter trial comparing glue fixation, self-gripping mesh, and suture fixation of mesh in Lichtenstein Hernia Repair (FinnMesh Study). Ann Surg 262:714–719 (discussion 719–720)
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Higgins JP, Altman DG, Gotzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Mills EJ, Thorlund K, Ioannidis JP (2013) Demystifying trial networks and network meta-analysis. BMJ 346:f2914
Dias S, Sutton AJ, Ades AE et al (2013) Evidence synthesis for decision making 2: a generalized linear modeling framework for pairwise and network meta-analysis of randomized controlled trials. Med Decis Mak 33:607–617
Higgins JP, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Dias S, Welton NJ, Caldwell DM et al (2010) Checking consistency in mixed treatment comparison meta-analysis. Stat Med 29:932–944
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Plummer M (2003) JAGS: a program for analysis of Bayesian graphical models using Gibbs sampling. In: Proceedings of the 3rd international workshop on distributed statistical computing, Vienna, Austria. 20–22 March 2003
R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria: [Accessed on 5 April 2018]. Available online: http://www.R-project.org/
Anadol AZ, Tezel E (2009) Prospective randomized comparison of conventional Lichtenstein versus self adhesive mesh repair for inguinal hernia. Surg Endosc 23:S315
Bruna Esteban M, Cantos Pallares M, Artigues Sanchez De Rojas E (2010) Use of adhesive mesh in hernioplasty compared to the conventional technique. Results of a randomised prospective study. Cir Esp 88:253–258
Chatzimavroudis G, Papaziogas B, Koutelidakis I et al (2014) Lichtenstein technique for inguinal hernia repair using polypropylene mesh fixed with sutures vs. self-fixating polypropylene mesh: a prospective randomized comparative study. Hernia 18:193–198
Fan JKM, Yip J, Foo DCC et al (2017) Randomized trial comparing self gripping semi re-absorbable mesh (PROGRIP) with polypropylene mesh in open inguinal hernioplasty: the 6 years result. Hernia 21:9–16
Jorgensen LN, Sommer T, Assaadzadeh S et al (2013) Randomized clinical trial of self-gripping mesh versus sutured mesh for Lichtenstein hernia repair. Br J Surg 100:474–481
Kapischke M, Schulze H, Caliebe A (2010) Self-fixating mesh for the Lichtenstein procedure—a prestudy. Langenbecks Arch Surg 395:317–322
Lionetti R, Neola B, Dilillo S et al (2012) Sutureless hernioplasty with light-weight mesh and fibrin glue versus Lichtenstein procedure: a comparison of outcomes focusing on chronic postoperative pain. Hernia 16:127–131
Molegraaf MJ, Grotenhuis B, Torensma B et al (2017) The HIPPO trial, a randomized double-blind trial comparing self-gripping Parietex Progrip mesh and sutured Parietex mesh in Lichtenstein Hernioplasty: a long-term follow-up study. Ann Surg 266:939–945
Nikkolo C, Vaasna T, Murruste M et al (2015) Single-center, single-blinded, randomized study of self-gripping versus sutured mesh in open inguinal hernia repair. J Surg Res 194:77–82
Pierides G, Scheinin T, Remes V et al (2012) Randomized comparison of self-fixating and sutured mesh in open inguinal hernia repair. Br J Surg 99:630–636
Porrero JL, Castillo MJ, Perez-Zapata A et al (2015) Randomised clinical trial: conventional Lichtenstein vs. hernioplasty with self-adhesive mesh in bilateral inguinal hernia surgery. Hernia 19:765–770
Sanders DL, Nienhuijs S, Ziprin P et al (2014) Randomized clinical trial comparing self-gripping mesh with suture fixation of lightweight polypropylene mesh in open inguinal hernia repair. Br J Surg 101:1373–1382 (discussion 1382)
Verhagen T, Zwaans WA, Loos MJ et al (2016) Randomized clinical trial comparing self-gripping mesh with a standard polypropylene mesh for open inguinal hernia repair. Br J Surg 103:812–818
Bracale U, Rovani M, Picardo A et al (2014) Beneficial effects of fibrin glue (Quixil) versus Lichtenstein conventional technique in inguinal hernia repair: a randomized clinical trial. Hernia 18:185–192
Campanelli G, Pascual MH, Hoeferlin A et al (2012) Randomized, controlled, blinded trial of Tisseel/Tissucol for mesh fixation in patients undergoing Lichtenstein technique for primary inguinal hernia repair: results of the TIMELI trial. Ann Surg 255:650–657
Dabrowiecki S, Pierscinski S, Szczesny W (2012) The Glubran 2 glue for mesh fixation in Lichtenstein’s hernia repair: a double-blind randomized study. Wideochir Inne Tech Maloinwazyjne 7:96–104
Hidalgo M, Castillo MJ, Eymar JL et al (2005) Lichtenstein inguinal hernioplasty: sutures versus glue. Hernia 9:242–244
Hoyuela C, Juvany M, Carvajal F et al (2017) Randomized clinical trial of mesh fixation with glue or sutures for Lichtenstein hernia repair. Br J Surg 104:688–694
Jain SK, Vindal A (2009) Gelatin-resorcin-formalin (GRF) tissue glue as a novel technique for fixing prosthetic mesh in open hernia repair. Hernia 13:299–304
Karigoudar A, Gupta AK, Mukharjee S et al (2016) A Prospective randomized study comparing fibrin glue versus Prolene suture for mesh fixation in Lichtenstein inguinal hernia repair. Indian J Surg 78:288–292
Kim-Fuchs C, Angst E, Vorburger S et al (2012) Prospective randomized trial comparing sutured with sutureless mesh fixation for Lichtenstein hernia repair: long-term results. Hernia 16:21–27
Moreno-Egea A (2014) Is it possible to eliminate sutures in open (Lichtenstein technique) and laparoscopic (totally extraperitoneal endoscopic) inguinal hernia repair? A randomized controlled trial with tissue adhesive (n-hexyl-alpha-cyanoacrylate). Surg Innov 21:590–599
Nowobilski W, Dobosz M, Wojciechowicz T et al (2004) Lichtenstein inguinal hernioplasty using butyl-2-cyanoacrylate versus sutures. Preliminary experience of a prospective randomized trial. Eur Surg Res 36:367–370
Paajanen H, Kossi J, Silvasti S et al (2011) Randomized clinical trial of tissue glue versus absorbable sutures for mesh fixation in local anaesthetic Lichtenstein hernia repair. Br J Surg 98:1245–1251
Shen YM, Sun WB, Chen J et al (2012) NBCA medical adhesive (n-butyl-2-cyanoacrylate) versus suture for patch fixation in Lichtenstein inguinal herniorrhaphy: a randomized controlled trial. Surgery 151:550–555
Testini M, Lissidini G, Poli E et al (2010) A single-surgeon randomized trial comparing sutures, N-butyl-2-cyanoacrylate and human fibrin glue for mesh fixation during primary inguinal hernia repair. Can J Surg 53:155–160
Wong JU, Leung TH, Huang CC et al (2011) Comparing chronic pain between fibrin sealant and suture fixation for bilayer polypropylene mesh inguinal hernioplasty: a randomized clinical trial. Am J Surg 202:34–38
The HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22:1–165. https://doi.org/10.1007/s10029-017-1668-x
Lin H, Zhuang Z, Ma T et al (2018) A meta-analysis of randomized control trials assessing mesh fixation with glue versus suture in Lichtenstein inguinal hernia repair. Medicine (Baltimore) 97:e0227
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rausa, E., Asti, E., Kelly, M.E. et al. Open Inguinal Hernia Repair: A Network Meta-analysis Comparing Self-Gripping Mesh, Suture Fixation, and Glue Fixation. World J Surg 43, 447–456 (2019). https://doi.org/10.1007/s00268-018-4807-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4807-3