Abstract
Introduction
Enhanced recovery after surgery (ERAS) programs provide a format for multidisciplinary care and has been shown to predictably improve short term outcomes associated with surgical procedures. Esophagectomy has historically been associated with significant levels of morbidity and mortality and as a result routine application and audit of ERAS guidelines specifically designed for esophageal resection has significant potential to improve outcomes associated with this complex procedure.
Methods
A team of international experts in the surgical management of esophageal cancer was assembled and the existing literature was identified and reviewed prior to the production of the guidelines. Well established procedure specific components of ERAS were reviewed and updated with changes relevant to esophagectomy. Procedure specific, operative and technical sections were produced utilizing the best current level of evidence. All sections were rated regarding the level of evidence and overall recommendation according to the evaluation (GRADE) system.
Results
Thirty-nine sections were ultimately produced and assessed for quality of evidence and recommendations. Some sections were completely new to ERAS programs due to the fact that esophagectomy is the first guideline with a thoracic component to the procedure.
Conclusions
The current ERAS society guidelines should be reviewed and applied in all centers looking to improve outcomes and quality associated with esophageal resection.
Similar content being viewed by others
Introduction
The initial enhanced recovery after surgery (ERAS) protocol was developed by the ERAS study group in 2001. The initial protocol focused on the importance of a multidisciplinary team collaboration to apply concepts which would maximize the efficiency of surgical recovery. Specific goals included utilizing multimodal systems to minimize complications, initiate and maintain evidence-based care protocols while assessing progress and compliance through continuous audit.
Early reports by Kehlet demonstrated significant opportunities for improving the efficiency of recovery following colonic resection utilizing a multimodal approach [1]. The ERAS study group produced a consensus statement regarding the clinical care of patients undergoing colonic resection in 2005 [2].
The ERAS Society was founded in 2010 to consolidate and promote ERAS principles. The initial ERAS guidelines for colonic resection had 24 core elements [2, 3], and subsequent guidelines have been published on colorectal surgery [4], gastrectomy [5], bariatric surgery [6], liver surgery [7] and gynecologic oncology [8, 9].
Esophagectomy for both malignant and benign disease has been identified as a particularly complex surgical procedure due to documented high levels of perioperative morbidity and mortality. A comprehensive review of complications associated with the esophagectomies performed in high-volume esophageal units utilizing a standardized format for documenting complications and quality measures has confirmed an overall complication rate of 59% with 17.2% of patients sustaining complications of IIIb or greater utilizing the Clavien–Dindo severity grading system. This same assessment demonstrated 30- and 90-day mortality rates of 2.4% and 4.5%, respectively [10]. These results are from high-volume esophageal centers; however, when mortality has been assessed from national audits, 30-day mortality associated with esophagectomy routinely remains above 5% [11], while 90-day mortality remains as high as 13% [12].
These outcomes accentuate the need for providing an enhanced recovery after surgery standardized format for esophagectomy which can be routinely applied and audited to improve international outcomes.
Methods
This project was initiated by the ERAS Society. A working group was assembled to include high-volume thoracic and upper gastrointestinal surgeons and anesthesiologists as well as ERAS nurses who had an established commitment to esophageal surgery as well as a demonstrated commitment to the application of ERAS within their own institutions. Contributors were also selected with the goal of having international representation.
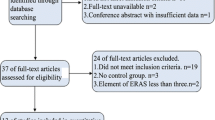
Surveys were initially circulated to the working group, and over 60 potential sections for inclusion into the ERAS guidelines were proposed. Following two Delphi surveys, 36 sections were identified for inclusion in the esophagectomy ERAS project. ERAS sections were divided into procedure-specific and non-procedure-specific components and subdivided into operative or technical issues and peri- and postoperative issues. Topics were assigned to individual members of the working group, taking into account areas of particular interest and expertise.
Each section underwent a comprehensive literature search spanning the time period between 1995 and 2017. This search placed emphasis on more recent publications, randomized controlled clinical trials and large high-quality cohort studies as well as systematic reviews and meta-analyses. Retrospective series were considered for inclusion if they had particular pertinence to a particular ERAS section and higher-quality evidence was not available.
Literature involving esophagectomy for both benign and malignant disease was included although some sections, for example lymphadenectomy, related only to esophagectomy for cancer. All sections were initially reviewed by two contributors, DEL and OL, and then sections were circulated for general review to the entire working group for final assessment.
Quality assessment and grading
The authors assessed the quality of evidence and the strength of the recommendations according to the well-established Grading of Recommendations, Assessment, Development and Evaluation (GRADE) system [13]. Quality of evidence was rated according to three separate levels: high, moderate and low. This assessment was based on the global assessment of the quality of the literature based on study limitations, consistency of results, directness of evidence, precision or the presence of reporting bias.
The grade of the recommendation was also assessed at three levels of quality: strong, moderate or weak. Strong recommendations are made when the desirable effects of an intervention clearly outweigh the undesirable effects, whereas moderate or weak recommendations result, either because of low quality of evidence or because evidence suggests that desirable and undesirable effects are closely balanced.
Commentary
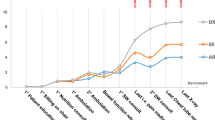
Preliminary results assessing the effect of ERAS on patients undergoing colorectal surgery have clearly demonstrated overall improvement in general clinical outcomes. Achieving these improved outcomes requires the successful initiation of a structured institutional ERAS program, but also requires ensuring that ERAS principles are maintained and adherence to programmatic goals are audited over time. Implementation of ERAS programs can be accomplished with high expectation of initial success in individual institutions. However, regular audit is critical as adherence to ERAS guidelines tends to decrease over time [14, 15].
Previous procedure-specific guidelines have undergone review to assess their effect on clinical outcomes. A report by Gustafson demonstrated that adherence to ERAS principles could produce a positive impact on complications, length of hospital stay and readmissions [16] associated with colorectal surgery. A reassessment of these results utilizing an audit by the ERAS Compliance Group confirmed this positive effect on outcomes in over 2300 patients treated in multiple centers [17].
ERAS programs have been directly linked to decreasing length of stay [18, 19] and reductions in the incidence and severity of postoperative complications [20]. Adherence to ERAS programs has also been demonstrated to decrease overall treatment-related costs [21].
Although adherence to ERAS programs has the potential to improve outcomes, there is clear recognition that the program must be multidisciplinary to be successful. Ideally, all participating stakeholders will be convinced and committed that ERAS goals are a critical component of patient-centered care within their areas of responsibility. A recent comprehensive review has highlighted the importance of ERAS principles with respect to anesthesiologists [22, 23], and standardizing the anesthetic approach to esophagectomy has already been demonstrated to be possible and to positively impact clinical outcomes with respect to esophageal resection [24].
Standardized and specific ERAS guidelines for esophagectomy have not been available until now. Systematic reviews of the effect of non-standardized enhanced recovery program with respect to esophageal resection typically acknowledge that the evidence demonstrating direct benefit is weak or lacking [25]. However, some more contemporary systematic reviews have highlighted that non-standardized approaches could be introduced safely and were likely associated with a reduction in length of stay [26]. Improvements in targeted discharge goals and length of stay have been documented in other single-center reports [27, 28]. Other reports have suggested improvements in anastomotic leak rate, pulmonary complications and length of stay, but have not demonstrated an improvement in overall mortality or readmissions [29]. However, all of these reports have utilized ERAS guidelines developed for, or adapted from, other major oncologic operations and not specifically designed to be applied for the unique challenges associated with esophageal resection. The current guidelines provide a specific structured framework of ERAS goals specifically aimed to improve outcomes associated with esophageal resection.
The current ERAS guidelines for esophagectomy cover all the critically important standard issues associated with enhanced recovery, but also address issues unique to esophageal resection. In some ways it is surprising that ERAS guidelines for esophagectomy have not been developed earlier as esophageal resection has historically been associated with higher levels of morbidity and mortality than virtually any other oncologic procedure.
The current guidelines are for utilization of all stakeholders and caregivers involved in the perioperative care of esophagectomy patients. The guidelines have also been developed not only to produce an infrastructure for perioperative care, but also to identify the specific issues within the ERAS guidelines which are appropriate and amenable for audit. This is an important issue, as it is the goal of the ERAS Society to not only provide infrastructure for initiation of ERAS guidelines, but also produce a workable system for long-term audit to monitor adherence to established guidelines and their impact on clinical outcomes over time (Table 1).
Procedure-specific components
Preoperative nutritional assessment and treatment
Esophageal cancer has the highest median weight loss, prior to diagnosis, of all cancers. The extent of weight loss directly relates to outcome with significant reduction in overall survival associated with more than 10% loss from premorbid weight. Malnutrition is also very prevalent in esophageal cancer and may affect up to 80% of patients and, as a result, is significantly associated with increased morbidity [30]. Nutritional assessment and support are therefore essential issues in the initial management of patients.
All patients with esophageal cancer should be assessed at diagnosis to determine whether they are malnourished. The following criteria established by the European Society for Clinical Nutrition and Metabolism (ESPEN) [31] should be evaluated at the initial consultation or at multidisciplinary tumor board once a diagnosis has been made.
-
Weight loss >10–15% in the previous 6 months
-
Body mass index <18.5 kg/m2
-
Serum albumin <30 g/l.
This assessment is ideally made by a qualified dietitian to determine the need for intervention.
Summary
Patients who undergo esophageal resections have a high prevalence of malnutrition, associated with an increased risk of complications.
Recommendation
Nutritional assessment should be undertaken in all patients with a view to detecting and optimizing nutritional status before surgery.
Evidence Level: Low
Recommendation Grade: Strong
Preoperative nutritional intervention
A number of risk scores for intervention have been described [32]. In principle, these are based on:
-
Identification of malnutrition
-
Assessment of the risk of malnutrition
-
Inadequate oral intake—dysphagia to all solids or minimal intake for 5 days
Those perceived to be at low risk should be given dietary advice. Moderate-risk patients should be given protein and energy supplements, and those at high risk should be considered for enteral support commonly with tube feeding (Table 2). These measures have been shown to improve patient outcomes [33].
Studies have reported the effect of counseling and advice to patients in different settings by dietitians [34, 35]. Although none have been in esophageal cancer, the findings of these reports can be applied. These approaches can result in an increase in energy and protein intake and some anthropometric parameters; however, there is little documentation regarding effect on quality of life. In addition, such approaches are labor-intensive in order to achieve the desired improvements.
Summary and Recommendation
Nutritional intervention should be based on the level of risk.
Recommendation
In high risk cases enteral support is indicated preferably using the GI tract with selective use of feeding tubes.
Evidence Level: Low
Recommendation Grade: Strong
Preoperative oral pharmaconutrition
Pharmaconutrition (PN) or immunonutrition involves the administration of immune-stimulating nutrients, primarily arginine, omega-3 unsaturated fatty acids and nucleotides. Immunonutrition is associated with increasing the immune response and reducing the inflammatory response, particularly the oxidative stress following major surgery that can contribute to organ damage [36]. Perioperative immunonutrition can potentially impact the incidence of postoperative morbidity including both infectious and non-infectious complications as well as length of hospital stay [37].
The role of postoperative immunonutrition remains controversial. Two systematic reviews have contradictory views on the impact of immunonutrition following esophagectomy [38, 39]. Sultan et al. concluded that early postoperative feeding with an immune-modulating diet conferred no outcome advantage when compared to a standard feed in esophagogastric cancer surgery [40]. In addition, two RCTs evaluated the impact of pre- and postoperative immunonutrition in patients undergoing surgery for esophageal cancer [41, 42]. One study concluded that eicosapentaenoic acid (EPA)-enriched enteral nutrition (EN) preserved lean body mass and attenuated the stress response in comparison with standard nutrition. Another study compared pre- and postoperative administration of antioxidant-enriched enteral nutrition with immune-enhancing enteral nutrition. The authors concluded no significant difference in body weight, BMI and inflammatory response between the two cohorts. Long-term outcomes were not evaluated in either study. Direct comparisons between the studies are not possible due to variations in the patient cohorts, differing nutrition regimes and control preparation that are not always isonitrogenous.
A recent randomized double-blind trial compared prolonged enteral nutrition with and without supplementation of omega-3 fatty acids in patients undergoing esophagectomy. This study analyzed the 1-, 3- and 6-month data for weight, body mass index (BMI), body composition, muscle strength, cytokines, complications and quality of life. In spite of excellent compliance with the enteral feeding regimen in both treatment groups, 30% of patients in this cohort of 191 had significant weight, muscle and fat loss postoperatively. Importantly, enteral nutrition with supplemental omega-3 fatty acids (eicosapentaenoic acid) did not have significant impact on anabolism, immune function and clinical outcomes post-esophagectomy [43].
Further trials are required and should be conducted in the current era of enhanced recovery with a standardized immunonutrition formula.
Summary and Recommendation
Evidence in support of pharmaconutrition for patients undergoing surgery for esophageal cancer is conflicting and its routine use cannot be supported at this time.
Evidence Level: Moderate
Recommendation Grade: Strong
Multidisciplinary tumor board
In a comprehensive review of the role of multidisciplinary teams (MDT), Taylor et al. [44] reported improved decision making by multiprofessional specialists. Treatment decisions originating in a MDT format lead to enhanced evidence-based treatment and increased quality of care, in addition to greater efficiency and better coordination of the patient journey.
Specifically, in esophageal cancer there is evidence of more accurate staging by an MDT allowing improved treatment selection [45] and improved surgical outcomes when surgical decisions are taken in the context of MDT discussion [46]. Similar results have been reported in a longitudinal study covering time before and after MDT implementation [47].
However, Blazeby and colleagues [48] have reported that 10–15% of MDT decisions in both curative and palliative gastroesophageal settings were not implemented, reflecting a lack of complete patient data. However, other reports have demonstrated that tumor board presentation can lead to a change in clinical treatment in 40% of patients, and implementation of MDT recommendations can be as high as 97% in some institutions [49].
The review by Taylor et al. [44] found that, despite the benefits to clinical coordination, there was little evidence of taking patient preferences into account; indeed, there was little consensus on how to involve patients. This was endorsed by a similar review from the USA [50]. It was this lack of patient engagement which Blazeby highlighted, particularly in the advanced disease setting.
Studies of MDT functioning have been limited to observational reports. MDTs have become part of standard practice, and randomized trials are now unlikely to occur. It is therefore difficult to demonstrate clearly whether MDTs have an effect on overall survival.
MDTs are advantageous to the overall management of patients with esophageal cancer facilitating input by the full spectrum of specialist opinion and ensuring a coordinated approach to care. The overall benefit to survival remains to be established, and there needs to be a better understanding of patient involvement in MDT decision making.
Summary and Recommendation
There is limited data to support an improvement in overall survival. MDTs should be fundamental to management planning for all patients with esophageal cancer. MDTs ensure appropriate multidisciplinary input into patient care and improve the quality of that care.
Evidence Level: Moderate
Recommendation Grade: Strong
Prehabilitation programs
A key determinant of ERAS program success is the rapid return to an acceptable level of functional activity after a major procedure. Since functional capacity has been shown to be a key issue associated with postsurgical complications [51] it seems logical that efforts to optimize and improve a patient’s physiological reserve before the intervention would improve outcomes. This process, termed “prehabilitation,” includes a multimodal approach incorporating nutritional intervention (e.g., protein supplementation), medical optimization (e.g., glycemic control, blood pressure control, smoking cessation, alcohol reduction) and psychological intervention (e.g., emotional stress reduction), in addition to a structured and goal-directed exercise program composed of both aerobic and strengthening activity [52]. Several small randomized trials investigating the value of prehabilitation programs after abdominal or oncologic surgery have demonstrated an increase in functional capacity [53,54,55]. However, despite improvements in physiological reserve, the impact on postsurgical outcomes has not yielded consistent results. The data regarding prehabilitation prior to esophagectomy will be augmented by two ongoing studies, one from Canada with promising preliminary results (Carli, F., personal communication, 2017) and another multi-institutional trial from France [56]. Therefore, at present, recommendations regarding prehabilitation prior to esophagectomy must be extrapolated from several small studies of either colonic resection or mixed patient population “upper abdominal” surgery [53, 54]. These publications do suggest that preoperative exercise (“prehab”) programs have a greater impact on return to baseline function than postoperative (“rehab”) programs [54] and that less than 4 weeks of prehabilitation is unlikely to influence outcomes.
Summary and Recommendation
Evidence from small studies supports the use of prehabilitation programs for major abdominal surgery, however there is limited data for esophagectomy. Patients undergoing esophagectomy may benefit from a multimodal prehabilitation program and ongoing assessments may provide additional information to direct future recommendations.
Evidence Level: Low (extrapolated, small studies)
Recommendation Grade: Moderate
Operative components
Timing of surgery following neoadjuvant therapy
Neoadjuvant therapy followed by surgery is now standard treatment for resectable stage II or III carcinoma of the esophagus, but the ideal timing between neoadjuvant therapy and surgery has not been defined [57]. Appropriate timing would balance the adverse effects of neoadjuvant therapy declining with the risk of the cancer progressing. In the major landmark trials of neoadjuvant chemotherapy the recommended interval before surgery varies from 2 to 6 weeks after completion of chemotherapy [58,59,60]. In this time, the adverse effects of neoadjuvant therapy can be expected to have decreased.
Neoadjuvant chemoradiotherapy is now the predominant neoadjuvant therapy worldwide, and in the recent neoadjuvant chemoradiotherapy CROSS trial, the recommended interval was 4–6 weeks after the last day of radiotherapy [61]. With neoadjuvant chemoradiotherapy, additional factors to consider are the possibility of ongoing tumor regression and a greater chance of pathological complete response (pCR) with a longer interval before surgery, but with an associated risk of post-radiotherapy fibrotic changes and therefore more challenging surgery. In a further analysis of the CROSS study [62], a longer time to surgery (up to 12 weeks) was found to increase the probability of a pCR and was associated with a slightly increased probability of postoperative complications, with no effect on disease-free or overall survival. The literature is conflicting, and a recent meta-analysis [63] reported that a longer interval to surgery (more than the standard 7–8 weeks) did not increase the pCR rate and was considered to lead to worse long-term outcomes.
Summary and Recommendation
The optimum time for surgery following neoadjuvant chemotherapy is 3–6 weeks following completion of chemotherapy. The optimum time for surgery following neoadjuvant chemoradiotherapy is 6–10 weeks following the last day of radiotherapy.
Evidence Level: Moderate
Recommendation Grade: Moderate
Access: minimally invasive or open
Since the early 1990s thoracoscopy and laparoscopy have seen increasing application in patients requiring esophagectomy either as a totally minimally invasive procedure or in a variety of different hybrid combinations with traditional open access. To date, there are a large number of case series and reviews, six meta-analyses and one RCT assessing the role of minimally invasive access in esophagectomy. Traditional invasive vs minimally invasive esophagectomy (TIME) trial is a RCT comparing early outcomes after minimally invasive esophagectomy (MIE) and open esophagectomy (OE) [64]. MIE was performed by a right thoracoscopy, upper abdominal laparoscopy and cervical incision, while OE comprised a right-sided thoracotomy and midline laparotomy with or without a cervical incision. Sixteen (29%) patients in the OE group developed postoperative pulmonary infection (primary outcome) in the first 2 weeks compared with five (9%) in the MIE group (RR 0.3, 95% CI 0.12–0.76; p = 0.005). Among secondary outcomes, MIE was associated with longer operative time, less blood loss, similar anastomotic leak rate and number of lymph nodes retrieved, lower rate of recurrent laryngeal nerve palsy, shorter length of stay (LOS), similar 30-day mortality and better quality of life 1 year after surgery as compared to OE [64, 65]. The six meta-analyses were exceedingly heterogeneous, but demonstrate that MIE was associated with a statistically significant reduced perioperative blood loss [66, 67], and a decrease in pulmonary infections [66, 67]. These findings were not confirmed in older meta-analyses [68]. The meta-analyses also documented similar leak rates, shorter hospital stay [66], similar mortality [66, 67, 69], similar [66, 68] or greater number of lymph nodes yielded [69], and equivalent overall survival [67, 68].
A propensity-matched population-based study of 1727 patients between the years 2011 and 2015 utilizing the Dutch Esophagectomy Database compared open versus minimally invasive transthoracic esophagectomy. This study reported that mortality and pulmonary complications were similar for OE and MIE. Anastomotic leaks and re-interventions were more frequently observed after MIE. MIE was associated with a shorter hospital stay [70].
Hybrid minimally invasive esophagectomy (HMIE) was compared with OE in a multicenter randomized trial for resectable cancers of the middle- or lower-third of the esophagus in 207 adult patients [71]. In this phase 3 controlled study, at 30-days, major postoperative morbidity occurred in significantly fewer patients in the HMIE compared to the OE group (35.9% vs 64.4%, p < 0·001). At 3 years, there was also a trend in the HMIE group toward improved overall survival and disease-free survival (67.0% vs 55%, p = 0.05 and 57% vs 48%, p = 0.15).
Summary and Recommendation
Both open and minimally invasive or hybrid approach to esophagectomy can yield acceptable outcomes. Recent assessments suggest that minimally invasive access during esophagectomy is feasible and safe and seems to be associated with some beneficial outcomes such as less perioperative blood loss, reduced rate of pulmonary infections and a shorter hospital stay without any clear significant disadvantages.
Evidence Level: Moderate
Recommendation Grade: Moderate
Choice of conduit
The most commonly used substitute organ after an esophageal resection is the stomach. Other potential replacements are colon and jejunum. The choice needs to be based on an awareness of the advantages and disadvantages of each as an esophageal substitute [72,73,74,75]. Advantages of the stomach are its relative ease of mobilization to reach even the neck and the need of only one anastomosis. Disadvantages include its sensitive vascularization, tendency to chronic reflux of acid and bile, and that its fundus has typically been within the field of preoperative radiotherapy for distal esophageal tumors which might impact healing at the site of anastomosis. Typically, the stomach cannot be used as an esophageal conduit if it previously has been partially resected or if the tumor extensively involves the proximal stomach.
Colon has a long length, is relatively resistant to acids and has excellent blood supply, but typically needs a preoperative evaluation before usage as an esophageal substitute to rule out any abnormalities or tumors as well as a need of preoperative bowel prep. Among the drawbacks of colon interposition are the longer operative time, and the requirement for three gastrointestinal anastomoses with the potential for long-term conduit redundancy.
Jejunal conduits have an antegrade segmental contraction and a low leakage rate, but will require technically complex supercharged microvascular anastomoses to reach the upper thorax or the neck.
There are no RCT comparisons between conduit options, and controlled observational studies are scarce. The limited available data, mostly case series, are conflicting regarding any differences in the long-term quality of life and functional outcome [74].
A systematic review of two RCTs and five cohort studies comparing whole stomach with gastric tube reconstruction after esophagectomy found a reduced risk of delayed gastric emptying, less reflux symptoms and better quality of life among patients with a gastric tube [76].
Summary and Recommendation
The stomach, colon and jejunum are all viable options for conduit reconstruction after an esophageal resection. There is no single option or substitute appropriate for all patients and circumstances. The decision needs to be based on an awareness of the possibilities and limitations as well as short-term and long-term advantages and disadvantages of each organ as an esophageal substitute. Due to its reliable vascularity, good outcome and relative simplicity a tubulized gastric conduit is recommended as the first option.
Evidence Level: Gastric conduit: Low
Tubulized stomach: Moderate
Recommendation Grade: Gastric conduit: Strong
Tubulized stomach: Strong
Role of pyloroplasty
The optimum management of the pylorus during esophagectomy remains unknown. The vagotomy that typically accompanies esophagectomy will denervate the pylorus, and this may lead to pylorospasm and gastric outflow obstruction. This may lead to an increased risk of aspiration, anastomotic leakage and failure to take adequate oral nutrition [25, 77, 78]. There are several other factors that affect the way the gastric conduit empties, such as the level and technique of anastomosis, the positioning of the conduit in the mediastinum, the length of time the gastric conduit is decompressed by the nasogastric (NG) tube and the rate of progression of oral intake. Many surgeons, nevertheless, routinely carry out pyloric drainage procedures such as pyloroplasty. Potential drawbacks, however, are bile reflux, shortening the conduit, prolonging the operation and potential risk of suture line leakage from the pyloroplasty. Many other factors influence gastric emptying. A meta-analysis in 2002 (9 RCTs, n = 553) concluded that although pyloroplasty significantly reduced gastric outlet obstruction, it made no difference to various outcome measures such as operative mortality, anastomotic leaks or pulmonary complications [77].
Alternative methods of improving gastric emptying following esophagectomy, such as pyloric dilatation, pyloric botulinum toxin injection [78], circular stapled pyloroplasty [79] and pyloromyotomy, have been suggested, but the current literature does not support making any recommendations at this time.
Summary and Recommendation
The evidence for pyloroplasty and other pyloric drainage procedures is limited, with no strong evidence of effect on outcome [4]. No specific recommendation on the role of pyloroplasty can made at this time.
Evidence Level: Low
Recommendation Grade: Strong
Lymphadenectomy [80]
Esophageal cancer is associated with a high rate of lymph node metastasis which varies according to histological subtype with a higher rate in equivalent stage for squamous cell carcinoma (SCC). Dissection of the lymph node stations is controversial, with some surgeons adopting a radical approach and others a more conservative philosophy.
Pathologically, the nodal stations involved relate to tumor site. Three-field lymphadenectomy removing upper abdominal, superior and inferior mediastinal and cervical nodes is advocated for upper- and middle-third SCC. There is a difference between two-field dissection for SCC and for adenocarcinoma (ACA) with superior mediastinal and recurrent laryngeal nerve (RLN) dissection more commonly performed in SCC.
Previous reports [81] have indicated an overall better survival for three-field dissection for SCC of the upper- and middle-third. However, this benefit is not observed with five or more positive nodes. In addition, three-field dissection is associated with increased morbidity and careful patient selection focusing on early-stage disease is recommended. An ongoing randomized trial (Pramesh C.S., personal communication, 2017, NCT 00193817) is evaluating the role of three-field lymphadenectomy in esophageal cancer, and the results are expected to provide a definitive answer to this long-standing controversy.
Experience with three-field dissection in the West is limited. Most favor two-field dissection reflecting the predominance of adenocarcinoma and patterns of recurrence. Isolated cervical node recurrence is rare and does not justify including neck dissection.
Although survival is related to the extent of nodal dissection, this should be considered in the context of disease stage at presentation. Two-field dissection is unnecessary in clinical T1a disease as the rate of nodal metastasis is very low. Extensive nodal involvement (>8 nodes) is a reflection of systemic disease, and there should be careful consideration of the benefit of surgery in such patients.
Recommendation
Two-field lymphadenectomy is recommended for T1b-T3/4 ACA in the middle and lower third of the esophagus. This should not include dissection of the recurrent laryngeal nerve nodes.
Three-field lymphadenectomy is recommended in upper third SCC but there should be careful selection according to early stage disease in patients with good performance status and surgery performed in experienced centers.
Evidence Level: Moderate
Recommendation Grade: Strong
Perianastomotic drains
Perianastomotic drains in esophagectomy have to be distinguished between cervical and thoracic on the basis of the surgical procedure. In thoracic cases, perianastomotic drain represents a drain placed in the mediastinum separate from the standard placement of a tube thoracostomy.
Only one randomized clinical trial on 40 patients tried to assess the usefulness of a cervical drainage. No leak was observed in either group, morbidity was comparable in the two groups, and the authors conclude that drainage does not give clinical information on leakage because it is often removed before the manifestation of anastomotic leak [82].
With regard to thoracic anastomosis drainage, the results from a retrospective study on 414 patients reported a comparable leak rate between the two groups (5.35% drainage; 3.64% no drainage). In the drainage group, an early diagnosis and faster resolution of the leak were shown, but without the need of any additional invasive procedure [83].
Two retrospective studies documented a correlation between high levels of drain amylase and the formation of anastomotic leak. Nevertheless, evidence is limited and an optimal amylase level cutoff is still debated [84, 85]
Summary and Recommendation
The use of perianastomotic drain in cervical anastomosis may be avoided (no benefit shown).
Evidence Level: Moderate
Recommendation Grade: Moderate
The evidence for benefit is very limited; and hence, no recommendation for perianastomotic drains in thoracic anastomosis can be made at this time.
NG tube/gastric decompression
A Cochrane review of the application of nasogastric decompression following abdominal surgery demonstrated that routine utilization of NG tubes did not accomplish any of its intended goals and therefore utilization should be on a “selective basis” rather than routinely applied. Historically, the utilization of gastric conduit decompression following esophageal resection has been considered of more importance compared to other abdominal resective procedures. Historic issues have included decreasing respiratory complications, decreasing the incidence of nausea and vomiting, avoiding conduit distension and decreasing the risk of anastomotic complications with the routine utilization of NG tubes for immediate postoperative conduit decompression [25]. Non-randomized comparative trials comparing NG tube decompression with either no nasogastric tube or a perioperative-placed gastrostomy have suggested an increased risk of anastomotic and respiratory complications in patients with nasogastric tubes [86]. However, two randomized controlled trials that have been conducted comparing standard nasogastric decompression with either early removal (on postoperative day 2) or no NG tube utilization showed that higher instances of pulmonary complications were seen in the group without nasogastric tube decompression [87, 88]. However, there was no difference in pulmonary or other complications in comparison between the early (POD 2) and delayed NG tube removal. Reinsertion rates were higher in the early removal group with patient discomfort being higher in the delayed group [87].
A recent meta-analysis highlighted that rates of anastomotic leak, pulmonary complications and mortality were not increased with immediate perioperative or early removal (on postoperative day 2) of NG tubes and that length of stay was found to be shorter when all studies were included in the meta-analysis, but not when the meta-analysis was limited to randomized controlled trials.
There are reports regarding the intraoperative insertion of retrograde jejunogastric decompression tubes and pharyngostomy tubes. The literature, however, is not extensive enough to include these approaches within the current recommendations.
Summary and Recommendation
Nasogastric tube decompression at the time of esophageal resection is currently recommended with the caveat of considering early removal (on postoperative day 2) when clinically appropriate.
Evidence Level: Moderate
Recommendation Grade: Strong
Chest drain management following esophagectomy
Routine chest drainage after esophagectomy is practiced in most centers and assists complete lung expansion and monitoring for air, chyle and anastomotic leaks. However, chest drainage is associated with increased pain and decreased mobility after surgery [89]. There is wide variation in the threshold volume and the duration for which the drains are retained after surgery [90]. Many centers practice routine drain removal when the volume is 100–150 mL though there is no evidence to support this threshold [90]. Two randomized trials (for non-esophageal indications) showed that fluid reaccumulation and re-intervention rates did not increase at a threshold of 200 mL per day [91, 92]. Even higher thresholds of 450 mL or more have been suggested in non-randomized studies on lung resectional surgery [93].
A randomized trial showed that passive chest drainage was as effective as active drainage after esophagectomy [94]. Traditionally, surgeons have used two drains after thoracotomy—one apical and one basal; however, studies, albeit after pulmonary resectional surgery, have shown that one drain was as effective as two drains and resulted in less postoperative pain and earlier discharge from hospital [95, 96].
Summary and Recommendation
The use (duration and number) of chest drains should be minimized. Chest drains may be removed in the absence of air and chyle leaks. A single mid-positioned drain is as effective as two drains and causes less pain; passive drainage is as good as active drainage.
Evidence Level: Weak
Recommendation Grade: Moderate
Routine use of enteric feeding tubes
Feeding after esophagectomy may be either enteral or parenteral with much of the data favoring an enteral route. Enteral feeding reduces surgical stress [97] and reduces postoperative complications including anastomotic leaks [98]. Three randomized trials on enteral feeding versus total parenteral nutrition (TPN) after esophagectomy showed no non-catheter-related complications with enteral feeding, while one of them showed an increase in catheter-related complications with TPN [99,100,101].
The options for enteral feeding include feeding jejunostomy or nasojejunal tubes—while feeding jejunostomies are commonly used, they have a recognized rate of complications, albeit minor with occlusion of the tube and dislodgement being the most common [102]. Nasojejunal and nasoduodenal tubes avoid the complications of feeding jejunostomies, but dislodgement can occur and patient preference between these two methods is unknown [103]. Currently, there is evidence to support initiating enteral nutrition early and reaching full calorie requirement target at 3–6 days following esophagectomy [104].
Summary and Recommendation
Early enteral feeding with target nutritional rate on day 3–6 should be strongly considered after esophagectomy. For appropriate target nutritional rate see post-operative feeding recommendations. Either feeding jejunostomy or nasojejunal/nasoduodenal tubes may be used.
Evidence Level: Moderate
Recommendation Grade: Moderate
Esophagectomy: perioperative fluid management
Most of the literature examining this subject has been related to major abdominal surgery [105]. Excess perioperative fluid may cause tissue edema, delayed return of normal gastrointestinal function, impaired wound healing, increased pulmonary edema and increased risk of cardiac and pulmonary failure [105,106,107]. Specifically following esophagectomy, an increased perioperative fluid balance has been reported to increase pneumonia, respiratory failure and delayed extubation [106, 107]. Prevention of fluid excess will reduce major morbidity by up to two-thirds and will reduce the length of stay [108, 109].
The assessments of fluid therapy have included outcomes from the liberal use of fluids to restrictive fluid therapy (RFT) or goal-directed fluid therapy (GDFT). There have been no studies of the use of GDFT that included esophagectomy. The most recent meta-analysis of GDFT included 23 RCT with 10 studies performed within an ERAS protocol. The authors found that over time the fluid volumes and goals for GDFT have reduced. They report analysis of early studies showed a reduced morbidity and length of stay, but these outcome differences disappeared if GDFT was used within an ERAS protocol in the most recent studies [110].
It is more relevant to focus on the benefit of balanced fluid therapy. In a meta-analysis of outcomes in elective open abdominal surgery, the authors did not find a difference between restrictive and standard or liberal fluid therapy. However, when balanced fluid therapy was compared with imbalanced therapy, there were 59% fewer complications and a 3–4 day shorter length of stay in the balanced fluid group [111].
Specific to esophagectomy, a review of the literature has recommended that during the abdominal phase the stroke volume should be optimized and during the thoracic phase the stroke volume should be monitored and aggressive fluid therapy should be avoided. The authors recommend the focus should be on balancing the fluids therapy rather than liberal or restrictive protocols [112].
Overall, the aim is for maintaining physiological blood flow dynamics with individualized and timely fluid replacement with or without vasopressor support. The placement and use of an epidural catheter impacts fluid therapy due to the vasodilation effect and potential for hypotension. If a patient with epidural analgesia is hypotensive, but normovolemic, vasopressors should be introduced [105]. Practically, perioperative fluids should be given aiming for zero weight gain [113]. In the postoperative phase the aim is for normovolemia, avoidance of excess fluids and a neutral fluid balance. In esophagectomy patients it has been recommended that the aim is for a mean arterial pressure of 70 mm Hg with fluid intake restricted to less than 30 mL/kg body weight [112]. Typically, a minimum urine output (UO) of 0.5 mL/kg/h has been the accepted norm. A recent RCT has shown equivalent outcomes when a UO of 0.2 mL/kg/h was accepted in patients having a colectomy who had no risk factors for an acute kidney injury [114].
Compared with balanced crystalloids, an excess of 0.9% saline increases the risk of electrolyte disturbance [115] and colloids do not offer better clinical outcomes than crystalloids [116].
Summary and recommendation
Optimal fluid balance should be the focus with consideration of all contributory factors, positive balance resulting in weight gain >2 kg/day is to be avoided.
Evidence Level: High
Recommendation Grade: Strong
Goal directed fluid therapy may be worthwhile for higher risk patients not part of a formal ERAS program.
Evidence Level: Moderate
Recommendation Grade: Weak
Balanced crystalloids use for fluid replacement is recommended.
Evidence Level: Moderate
Recommendation Grade: Moderate
Anesthetic management
The intraoperative anesthetic management of esophagectomy patients focuses on two goals: first, to minimize pro-inflammatory local (pulmonary) and systemic responses that are associated with postoperative complications; second, to facilitate early extubation, which reduces postoperative pulmonary complications and enables early ambulation.
Anesthetic maintenance
The selection of volatile versus intravenous anesthetic regimens for intraoperative maintenance does not affect major complications after pulmonary surgery [117]. Early extubation is facilitated by titrating depth of anesthesia with bispectral index (BIS) monitoring [118] and by avoiding long-acting neuromuscular blockers (NMBs) or excessive dosing of intermediate-acting NMBs [119].
Two-lung ventilation
Lung protective ventilatory strategies reduce local and systemic inflammation, enable early extubation and reduce the likelihood of subsequent invasive or noninvasive ventilation. Evidence-based support for two-lung protective ventilation (TLV) strategies is more robust than that for one-lung ventilation (OLV) strategies. For TLV, high-level evidence supports the use of low-tidal volume (VT) 6–8 mL/kg predicted body weight (PBW) during abdominal surgery. The benefits of routine, high (> 2 cm H2O) positive end-expiratory pressure (PEEP) and recruitment maneuvers are unclear, in part because they have been studied mostly as adjuncts to low VT rather than in isolation, are associated with hypotension, and have not been linked to improved pulmonary outcome in patients without underlying lung injury [120,121,122].
One-lung ventilation
Similar to TLV, the management of OLV needs to ensure adequate gas exchange for systemic oxygen delivery, protect the ventilated lung from ventilation-associated lung injury and the underlying inflammatory response, and optimize perfusion through the two lungs to minimize shunt circulation. To this end, steps should be taken to minimize the duration of OLV, avoid hyperoxia, and adjust respiratory rate to allow mild hypercapnia. Provision of 100% oxygen and recruitment just prior to initiation of OLV should be supplanted soon thereafter by the lowest FiO2 that maintains SpO2 >92%. Specific to esophagectomy, an OLV strategy of VT 5 mL/kg and PEEP 5 cm H2O to the ventilated lung was shown to decrease pro-inflammatory systemic response and promote early extubation [123]. The application of CPAP 5 cm H2O to the non-ventilated lung temporarily reduced local immune response without affecting systemic response or altering clinical outcome after laparoscopic esophagectomy, but doing so disturbed surgical visibility occasionally [124]. Nevertheless, there is no clinical evidence to support outcome improvement through the use of PEEP to the ventilated and/or CPAP to the non-ventilated lung [125]. Persistent hypoxia below SpO2 90% can often be rectified by increasing PEEP and instituting recruitment maneuvers to the ventilated lung up to every 30 min. Intermittent lung re-inflation may be necessary if these strategies fail to achieve adequate oxygenation.
The translation of knowledge gained from principles of lung protective ventilation in patients with acute respiratory distress syndrome (ARDS) to intraoperative ventilator management has embraced the importance of low-VT ventilation with appropriate PEEP to reduce cyclic opening and closing of lung units, thereby avoiding volutrauma and barotrauma. Lately, it has become clear that ventilated patients with ARDS only realize the benefits of low VT when associated with low driving pressures, because the latter parameter is now believed to be the major factor determining lung injury and the cause of worse clinical outcome [126]. Similar analysis also identified driving pressure, rather than VT or PEEP, as the major mediating factor of postoperative complications in a large meta-analysis of individual patient data undergoing various forms of general and thoracic surgery [127]. Two additional concepts relate to regular recruitment maneuvers to the ventilated lung to avoid atelectasis and hyperoxia to limit reactive oxygen species generation. The optimal PEEP in thoracic anesthesia is not known, but likely requires careful titration and continuous monitoring of SpO2 and frequent blood gases. The current PROTHOR trial is designed to test two levels of PEEP in routine thoracic surgery. Importantly, translation of beneficial respiratory parameters derived from the management of lung-injured patients from the critical care setting to the operative theater has not been fully elucidated.
Summary and Recommendation
Volatile or intravenous anesthetics are equally effective for maintenance of anesthesia. Intermediate-acting NMBs, BIS monitoring, avoiding volume overload, and lung protective strategies facilitate early extubation and reduce postoperative complications. Clinical evidence supporting lung protection strategies is strong for TLV, but less well studied during OLV.
Anesthetic Maintenance
Evidence Level: Volatile or intravenous maintenance of anesthesia—Moderate
Appropriately-dosed intermediate-acting muscle relaxants—High
BIS—High
Avoid volume overload—Moderate
Recommendation Grade: Strong
Two - Lung Ventilation
Evidence Level: Low VT(6–8 mL/kg PDW)—High
Routine PEEP > 2–5 cm H2O and recruitment maneuvers have not been fully defined—Moderate
Recommendation Grade: Strong
One - Lung Ventilation
Evidence Level: Avoid hyperoxia; allow mild hypercapnia—Strong
Low VT(4–5 mL/kg PBW)—Moderate
PEEP (5 cm H2O) ventilated lung—Low
CPAP (5 cm H2O) non-ventilated lung—Low
Recommendation Grade: Moderate
Post- and perioperative issues
Intensive care unit utilization
Conventional postoperative management after esophagectomy often involves routine admission to intensive unit (ICU). Some patients are left intubated and ventilated for up to 48 h with sedation. Sedation for comfort often leads to hypotension, to which over-enthusiastic intravenous fluid replacement or use of vasopressors may compromise perfusion of the gastric conduit. With availability of better pain relief, such as thoracic epidurals, and minimally invasive approaches, immediate extubation has become more common [128]. In most hospitals, step or progressive care units (PCU) may also be suitable for esophagectomy patients, thereby avoiding routine admission to ICU. The advantages of routine admission to ICU have been questioned [129,130,131,132]. The avoidance of routine ventilation and ICU admission potentially has significant economic implications. Large retrospective analysis has shown large variation in the use of ICU after major surgery without any impact on outcome [133].
Summary and Recommendation
Postoperative management of patients after esophagectomy should be individualized and does not routinely require ICU care. The availability of PCU/HDU is a safe alternative for lower risk patients.
Evidence Level: Moderate
Recommendation Grade: Strong
Perioperative pain control for esophagectomy
Perioperative pain control is important for humane reasons, in addition to reducing the stress response and restoring function so that a patient can breathe normally and mobilize, take enteral nutrition and sleep. Analgesia for esophagectomy poses challenges because it is often a two-cavity surgery, there is a large surface area of dissection, and a gastric tube is fashioned and moved from the abdominal cavity into the chest. The choice of analgesia will depend on the surgical approach, the position and sizes of incisions and patient factors. The situation is complicated further by the need for chest and abdominal drains. There also needs to be a plan for breakthrough pain and failure of the initial first-line technique.
The rationale of the ERAS approach to analgesia is to use multimodal analgesia combined with regional and local anesthetic techniques to allow a patient’s opiate consumption to be minimized. This avoids the unwanted side effects of sedation, nausea and vomiting, delirium and gut dysfunction. There are few specific studies on analgesia within enhanced recovery pathways so much of the evidence is extrapolated.
Multimodal non-opioid analgesia
The backbone of multimodal analgesia for esophagectomy within an ERAS program is a major opioid-sparing local anesthetic technique such as thoracic epidural anesthesia (TEA) or paravertebral block catheters combined with non-opioid medication. Acetaminophen (paracetamol) combined with a nonsteroidal anti-inflammatory drug (NSAID) is a good combination. Opioids are best reserved for breakthrough pain. Other analgesic adjuncts such as gabapentinoids, magnesium, ketamine and lidocaine are being increasingly used.
Thoracic epidural anesthesia
Thoracic epidural anesthesia (TEA) has been shown in some esophagectomy studies to offer the best analgesia in open thoraco-abdominal operations [134]. An accurately sited catheter may be effective in producing analgesia to cover both the thoracic and abdominal components although some centers use two catheters sited several dermatomes apart. The use of an epidurogram after siting improves efficacy. TEA may reduce respiratory complications, the stress response and the development of chronic pain post-thoracotomy pain [135]. Dilute local anesthetic solutions with opioids offer the best analgesia and minimize the risk of motor block. Bolusing the epidural should be avoided to avoid hypotension. Patients will selectively need vasopressors to maintain mean arterial pressure to maintain splanchnic perfusion when using TEA, but it is important to ensure the patient is not hypovolemic before starting them [136]. The use of vasopressors remains controversial. There is conflicting evidence that TEA may improve gastric conduit flow [137], but that vasopressors may contribute to conduit ischemia [138]. Other work has shown that, provided the patient is normovolemic, the use of phenylephrine [139] or adrenaline (epinephrine) [140] infusions to restore MAP while using TEA increases conduit blood supply and oxygen delivery.
Summary and Recommendation
Thoracic epidural analgesia should be considered as first line approach to post-operative analgesia following esophagectomy.
Evidence Level (extrapolated): Moderate
Recommendation Grade: Strong
Paravertebral analgesia
Paravertebral block (PVB) analgesia has gained favor in some surgical units due to the issues of hypotension and poor mobility with TEA. Several papers and a meta-analysis have shown analgesia to be as effective as TEA for analgesia in thoracotomy, but with fewer complications and less hypotension [141,142,143]. The use of PVB is a good alternative to TEA particularly when the abdominal component of esophagectomy has been done laparoscopically.
Summary and Recommendation
Paravertebral blocks are a good alternative to TEA following esophagectomy.
Evidence Level (extrapolated): Moderate
Recommendation Grade: Strong
Acetaminophen
Acetaminophen is administered q6 hourly and is safe provided the dose does not exceed 4 g in 24 h. It has analgesic, anti-inflammatory and antipyretic activity. Acetaminophen can be given via the intravenous, oral and rectal routes. The intravenous route enables rapid attainment of blood levels and is particularly useful during surgery and in the immediate postoperative period when the enteral route can be difficult in esophageal patients; however, it is more expensive.
Summary and Recommendation
Regular acetaminophen dosing should be considered post-esophagectomy.
Evidence Level (extrapolated): Moderate
Recommendation Grade: Strong
NSAIDS
NSAIDS can be COX1 or COX2 and can be given orally, intravenously and rectally. The common side effects are gastric irritation and erosion, platelet dysfunction and renal dysfunction. In esophageal surgery where there is a higher risk of renal dysfunction, it is reasonable to delay dosing until after surgery when it has been confirmed that renal function is not impaired. Intravenous examples of NSAIDS are ketorolac and parecoxib.
Summary and Recommendation
Commence NSAIDS on an individualized basis taking into account complexity and difficulty of surgery, age and renal function.
Evidence Level (extrapolated): Moderate
Recommendation Grade: Strong
Gabapentinoids
Gabapentin and pregabalin are being increasingly used to treat acute pain and neuropathic pain. The potential advantages are to reduce opioid consumption and to reduce the incidence of chronic thoracotomy pain [144]. There have been no studies to date in esophageal surgery addressing this.
Summary and Recommendation
Gabapentinoids may be applicable for post-esophagectomy analgesia but limited evidence is currently available.
Evidence Level (extrapolated): Low
Recommendation Grade: Weak
Ketamine
In many studies ketamine has been used in major abdominal surgery as an adjunct to improve analgesic efficacy and reducing opiate consumption [145]. It may also have a role in reducing chronic pain if run as a postoperative infusion. The dose and timing have not been examined in esophagectomy patients.
Summary and Recommendation
Ketamine may be applicable for post-esophagectomy analgesia but additional studies are required.
Evidence Level (extrapolated): Moderate
Recommendation Grade: Weak
Magnesium
Magnesium has analgesic properties and has a low side effect profile [146]. It has the additional benefit of reducing perioperative supraventricular arrhythmias.
Summary and Recommendation
Magnesium may be applicable for post-esophagectomy analgesia but additional studies are required.
Evidence Level (extrapolated): Moderate
Recommendation Grade: Weak
Lidocaine infusions
Lidocaine is an amide local anesthetic acting on Na+ channels. There is increasing interest also in how lidocaine interacts with muscarinic, dopaminergic and nicotinic receptors at plasma concentrations much lower than those needed to achieve sodium channel blockade in nerves. Lidocaine infusions have been shown to have analgesic, anti-inflammatory and hyperalgesia qualities and accelerate bowel function. There are an increasing number of studies to show a morphine-sparing effect in abdominal surgery, but there are no data in esophagectomy. Because of concerns for local anesthetic systemic toxicity, intravenous lidocaine should not be used in patients receiving epidural or paravertebral local anesthetic infusion.
Summary and Recommendation
Lidocaine infusion likely has a role in post-esophagectomy analgesia in patients not getting it through an epidural or paravertebral infusion but further studies are required.
Evidence Level (extrapolated): Moderate
Recommendation Grade: Weak
Postoperative early nutrition: oral vs Jejunostomy
Patients are at high risk of malnutrition when undergoing surgery for esophageal cancer. The disease itself can potentially reduce oral intake. In addition, the impact of chemotherapy, magnitude of the surgery, the physiological impact of a reconstructed upper gastrointestinal tract and in most cases poor nutritional state in the peri-operative period are major contributors to the increased malnutrition risk. As a consequence, nutritional support may at times be required for months following surgery [147].
Enteral nutrition is associated with reduced postoperative complications rates and length of hospital stay in comparison with parenteral nutrition [148, 149]. Establishing enteral nutrition in the early postoperative period has been shown to reduce the incidence of life-threatening complications and decrease postoperative hospital stay following esophagectomy [150].
Early oral feeding has been shown to have positive outcomes in patients who have undergone gastrointestinal surgery. However, there is an increased risk of vomiting and aspiration pneumonia [149]. Oral feeding in the presence of serious complications might not be possible and/or be associated with morbidity and mortality. Two RCTs have compared early versus late oral feeding in patients undergoing major upper gastrointestinal surgery. Both the studies were associated with reduced hospital stay with no associated increase in morbidity in patients who had early oral feeding.
Weijs et al. reviewed the routes for early enteral nutrition after esophagectomy. Thirteen studies evaluated the outcomes of feeding jejunostomy. Surgical placement of a feeding jejunostomy was associated with a mortality of 0–0.5% and re-operation rate of 0–2.9%. Other complications noted were entry site infection (0.4–16%), entry site leakage (1.4–25%) and gastrointestinal tract complaints (10–39%). Nutritional outcome was reported in four studies, three of which reported that 88–100% of the nutritional requirement was met between postoperative day 3 and day 6 in patients with a jejunostomy. Three prospective studies evaluated the role of nasojejunal feeding. No long-term nutritional outcomes were assessed. The main issue was dislocation of the tube, and 20–35% of patients required readmission for management of feeding access [104].
One RCT compared early NJ feeding versus feeding jejunostomy. Time to reach the target nutritional rate (3 days) and the duration of nutritional support (3 days) were similar in both cohorts. Tube-related complications were higher in the jejunostomy group (38% vs 29%).
Patients are at high risk of malnutrition following surgery for esophageal cancer, further compounded if they have undergone neo-adjuvant treatment. In addition, nutritional status will impact the provision for further adjuvant treatment. Establishing early enteral nutrition is important; however, the ideal route of administration remains unclear. Further trials are required to assess the long-term nutritional outcomes and patient satisfaction.
Summary and Recommendation
Introduction of early enteral nutrition is beneficial in patients undergoing surgery for esophageal cancer.
Evidence Level: Moderate
Recommendation Grade: Strong
The ideal route of administration of enteral nutrition in the early post-operative period remains unclear. No recommendation can be given at this time.
Early mobilization
Modern surgical patients spend very little time out of bed [22], and early structured mobilization is a major component of virtually all ERAS programs. Bed rest leads to increased muscle loss and weakness, impaired lung function and tissue oxygenation, insulin resistance, and increased risks of thromboembolic and respiratory complications [151,152,153,154]. Early mobilization not only helps preserve muscle function and prevent complications associated with bed rest, but also empowers patients to take an active role in their recovery from surgery. It is, however, a particular challenge following esophagectomy because of potential restrictions imposed by pain and various medical instruments such as drains, feeding apparatus and pumps. The evidence for the timing and nature of mobilization is lacking, although one narrative review of 9 non-randomized studies [152] concluded that early mobilization might reduce the incidence of VTE and hasten functional recovery after surgery.
Protocols differ between pathways [22], but the key elements are: [22, 152]
-
A standardized and structured approach.
-
Start before surgery with a prehabilitation program.
-
Postoperative mobilization to start on the day of surgery whenever feasible.
-
Incremental increase in activity each day to reach predetermined targets.
-
Provision of written material including pictures for patient with description of mobilization goals and explanation as to why each activity target is important.
Recommendation
Postoperatively, early mobilization should be encouraged as soon as possible using a standardized and structured approach with daily targets to meet.
Evidence Level: Moderate
Recommendation Grade: Strong
The role of multidisciplinary standardized clinical pathways
Multidisciplinary care entails appropriately utilizing knowledge, skills and best practice from multiple disciplines and professions to optimize patient care and outcome. To coordinate interventions from different disciplines, goal-directed evidence-based standardized clinical pathways that serve as templates for all medical personnel have been developed in the last decades. For patients undergoing esophagectomy such pathways have been successfully introduced with reduced morbidity, length of stay (LOS) and costs [25, 29, 155,156,157]. A pooled analysis of nine single-institutional studies comprising 1240 patients, of which 661 underwent conventional pathway and 579 a standardized pathway after esophagectomy, demonstrated a reduction in anastomotic leaks (12.2–8.3%), pulmonary complications (29.1–19.6%) and LOS (17.3–13.0 days) among patients in standardized pathways [157].
Summary and Recommendation
Evidence supports multidisciplinary care using a standardized pathway in the perioperative care of patients undergoing esophagectomy.
Evidence Level: Low
Recommendation Grade: Strong
Audit
There is a lack of proper and basic outcomes information from surgery in many countries in the world. While some countries, especially in Northern Europe, have implemented national quality registries for many surgical procedures, for a broader view of European outcomes even the more basic information such as mortality after major operations relies on research initiatives [158]. In North America, NSQIP, the National Surgical Quality Improvement Program (https://www.facs.org/quality-programs/acs-nsqip), is a non-compulsory dataset run by the American College of Surgeons and has a similar function by collecting random samples and reporting outcomes benchmarking from hospitals choosing to contribute to the database.
For the single unit, it is also important to understand why their outcomes are a certain way, and to achieve this insight, they need to know not only the outcomes, but also the details of their practice leading to the outcome. Members of the ERAS® Society have repeatedly shown that by auditing outcomes alongside the practice of guideline elements, a clear relationship can be shown. With improved compliance to guidelines, morbidity is reduced and length of stay shortened [17, 159, 160], resulting in healthcare cost savings [161]. Recently, an association between compliance and long-term cancer survival was also reported [162]. Furthermore, the use of continuous audit of goals within the patient’s journey as part of daily practice while also assessing compliance with the guideline protocols has resulted in improved outcomes [160, 161, 163]. However, reports indicate that if the audit is stopped, there is a risk of falling back in both compliance with best practice, and outcomes [14].
Summary and Recommendation
Continuous institutional audit of outcomes alongside key care processes should be part of daily practice. Audit contributing to institutional, regional, national or international datasets for benchmarking should be a targeted goal.
Evidence Level: Moderate
Recommendation Grade: Strong
Non-procedure specific
Preoperative counseling patient/family
With the near-limitless, but frequently contradictory, patient information that is available on the Internet, structured and peer-reviewed accurate information is vital to reduce patient confusion [164]. With this in mind, patient education has become an integral component of ERAS programs, with several excellent Web sites on pre-esophagectomy education available [165]. However, navigating these Web sites alone can still be a daunting task, and direct patient counseling with a healthcare professional facilitate retention of information [166]. Preoperative counseling, be it by a physician or allied health professional, has a primary goal of increasing a patient’s familiarity and education concerning the planned procedure and thereby facilitating preparedness and reducing anxiety. However, several studies on procedure-specific preoperative counseling have found inconsistent results in reduction of anxiety [167, 168], and the role of preoperative counseling on postsurgical outcomes, particularly after esophagectomy, is unknown.
Summary and Recommendation
Patients undergoing esophagectomy, and their family or care taker, should receive pre-operative counseling with emphasis on postoperative targets and goals.
Evidence Level: Low
Recommendation Grade: Strong
Smoking–alcohol cessation
Regular (daily) smokers have an increased risk of perioperative morbidity, primarily wound and pulmonary complications [169]. Randomized trials have shown that abstinence of at least a month reduces postoperative complications significantly [170, 171]. A retrospective study evaluated postoperative complications based on varying durations of smoking cessation and found an almost linear decrease in postoperative pneumonia and severe morbidities with increasing periods of cessation [172].
Similarly, postoperative complications are considerably higher (two- to threefold increase) among alcohol abusers with an increase in hemorrhagic, wound and cardiopulmonary morbidity [169, 173]. A randomized trial showed that 4 weeks of abstinence prior to surgery decreased the complication rate [174]. From a practical standpoint, the few weeks of neoadjuvant treatment and the preoperative period provide an excellent window to implement smoking and alcohol cessation initiatives.
A randomized controlled study demonstrated structured efforts in combination of brief counseling by the preadmission nurse, brochures on smoking cessation, referral to the Smokers’ Helpline and a free 6-week supply of transdermal nicotine replacement therapy resulted in decreased smoking rates on the day of surgery and promoted abstinence 30 days postoperatively. However, the overall rate of combined intraoperative and immediate postoperative complications was not significantly different between intervention and control groups [175].
Summary and Recommendation
Smoking should be stopped 4 weeks prior to surgery and regular high alcohol consumers should abstain at least 4 weeks before surgery to reduce postoperative complications.
Evidence Level: Moderate (extrapolated)
Recommendation Grade: Strong
Cardiopulmonary assessment
Patients undergoing preoperative assessment for esophagectomy will selectively undergo echocardiography, spirometry and treadmill or dobutamine stress test. Routine tests to assess cardiopulmonary performance may identify some high-risk patients, but do not provide accurate objective information or guide management to reduce postoperative morbidity and mortality [176].
Cardiopulmonary exercise testing (CPET) provides an integrated method of assessment of all body systems including respiratory, cardiac, vascular, hematopoietic and musculoskeletal. It is noninvasive, dynamic and safe. It permits assessment of both maximal and submaximal peak exercise response to stress. It therefore allows the clinician to diagnose exercise intolerance and functional capacity. It is important to emphasize that one of the major advantages of CPET is its ability to be a dynamic test as resting respiratory and cardiac assessment of “fitness” cannot reliably predict body’s response to stress; CPET therefore provides a better predictive representation of overall health status [177]. Multiple physiological parameters can be measured using CPET including the anaerobic threshold (AT).
Older et al. demonstrated that all postoperative cardiopulmonary deaths occurred in patients (>60 years of age or younger with known cardiopulmonary disease undergoing major abdominal surgery) with an anaerobic threshold (AT) of <11 mL/min/kg and/or with significant myocardial ischemia on CPET [178]. Forshaw and colleagues have also demonstrated that esophagogastric patients whose anaerobic threshold was below that of 11 mL/min/kg were at greater risk of developing postoperative complications. This was more marked in those whose anaerobic threshold was below that of 9 mL/min/kg [179]. However, an earlier study by the same author had demonstrated that an AT cutoff of 11 mL/kg/min was a poor predictor of postoperative cardiopulmonary morbidity. This study did, however, demonstrate that VO2 peak was significantly lower in patients with postoperative cardiopulmonary morbidity [180].
One systematic review of the role of CPET assessment in non-cardiopulmonary surgery has demonstrated that CPET-derived variables are superior to other methods of fitness assessment. Furthermore, in 11 of 12 and 7 of 12 studies in this review, a significant association was noted between VO2 at anaerobic threshold and VO2 at peak and postoperative outcomes, respectively [181]. It is also important to appreciate that many patients receive neoadjuvant oncological therapy prior to surgery. A recent study has demonstrated that neoadjuvant chemotherapy reduces patient’s anaerobic threshold significantly. This reduction in fitness may further impact perioperative morbidity [182]. The relationship of this reduction in fitness and perioperative morbidity is yet to be clearly defined among the cohorts receiving neoadjuvant chemotherapy and neoadjuvant chemoradiotherapy.
Summary and Recommendation
CPET results have been used to assess patients undergoing major surgery, to guide preoperative optimization, to predict postoperative cardiopulmonary complications after surgery and, in some centers, to assess whether borderline patients should undergo resection. Evidence in support of the use of exercise derived parameters in risk stratification of esophageal resection patients is currently limited.
Evidence Level: Low
Recommendation Grade: Moderate
Bowel preparation (taking into account issues regarding colonic reconstruction)
Mechanical bowel preparation (MBP) is often practiced by surgeons when a colonic reconstruction is considered after esophagectomy. However, MBP may cause several adverse physiological effects including fluid losses, electrolyte imbalance and dehydration [183]; moreover, it is also associated with patient distress and prolonged paralytic ileus after colonic surgery. A recent Cochrane systematic review and meta-analysis included eighteen randomized trials and 5805 patients. It showed no differences in anastomotic leakage, wound infection rates and postoperative mortality between patients undergoing MBP and those who did not [184]. The authors conclude that “bowel cleansing can be safely omitted and is not associated with a lower complication rate.” Another systematic review included 14 randomized trials and 5373 patients and showed similar results confirming that postoperative incidence of anastomotic leaks, wound infections and mortality was not different in the two groups [185]. Therefore, although there are no trials evaluating the need for MBP for esophageal resections not planned for colonic reconstruction, extrapolation from colonic surgery strongly suggests that routine bowel preparation may be unnecessary unless the colon is to be used for reconstruction.
Summary and Recommendation
Mechanical bowel preparation does not reduce the incidence of postoperative complications and should not be used routinely prior to esophageal resection with gastric reconstruction. Most surgeons would still recommend MBP for planned colonic reconstruction although evidence is lacking.
Evidence Level: Moderate (extrapolated)
Recommendation Grade: Strong
Preoperative fasting
Prolonged fasting (>6 h) prior to a general anesthetic was previously a widely supported paradigm due to a perceived risk of aspiration at time of induction [186]. However, the detrimental effects of prolonged fasting are not insignificant, including increased patient discomfort, enhanced insulin resistance and increased postsurgical stress response. Over the past decade and a half, abundant research has not supported routine, prolonged fasting as a strategy to reduce aspiration or other perioperative complications. Rather, ingestion of clear liquids up until 2 h prior to the surgery, particularly with specifically designed preoperative drinks high on complex carbohydrates, has shown to diminish insulin resistance [187, 188] and postoperative nausea [189] and may reduce length of stay after major abdominal surgery [190]. Indeed, numerous anesthesia guidelines allow for clear liquids up until 2 h prior to a planned procedure [190]. However, there are insufficient data regarding esophagectomy, and certain patients undergoing this procedure, particularly those with significant obstructive symptoms, may dampen the enthusiasm for more liberal fasting recommendations in esophageal cancer patients with dysphagia. There are sparse data on the use of carbohydrate drinks in diabetics.
Summary and Recommendation
Prolonged fasting should be avoided, and clear liquids, including specific preoperative high-carbohydrate drinks, should be allowed until 2 h prior to esophagectomy. Caution should be applied for patients with significant dysphagia or other obstructive symptoms.
Avoidance of Preoperative fasting
Evidence Level: High
Recommendation Grade: Strong
Preoperative carbohydrate drinks
Evidence Level: Low (extrapolated)
Recommendation Grade: Moderate
Preanesthetic analgesics and anxiolytics
A single dose of paracetamol (acetaminophen) has been shown to reduce postoperative pain in a range of surgical procedures; however, major oncologic procedures such as esophagectomy were not studied [191]. Other pre-emptive analgesics have not been proven to be beneficial [192]. Patients’ chronic analgesics should be continued until the time of surgery. Preanesthetic short-acting anxiolytics might be beneficial to relieve anxiety during insertion of epidural catheter and induction of anesthesia, while longer-acting drugs might increase sedation on POD 1 [193, 194]
Summary and Recommendation
Long acting anxiolytics should be avoided, especially in the elderly, while short acting drugs may be used to reduce preoperative anxiety.
Evidence Level: Moderate
Recommendation Grade: Weak
Postoperative nausea and vomiting
Postoperative nausea and vomiting (PONV) affects 25–35% of surgical patients [195]. No specific study on PONV in esophagectomy has been published.
High-risk patients should be identified in order to initiate PONV prophylaxis. Female gender, history of PONV, non-smoking status and younger age are the strongest patient-specific predictors, while the use of volatile anesthetics, duration of anesthesia, postoperative opioid use and nitrous oxide are the strongest anesthesia-related predictors [195]. Apfel’s simplified risk score, based on the first four of these predictors, has demonstrated a correlation between an increased risk of PONV and the presence of one or more factors (from 1 to 4, risk increases from 10 to 80%) [196]. Patients with two or more risk factors should be given prophylaxis; a combination therapy with two or more antiemetics should be preferred to high dose of a single medication [196]. Excellent results were obtained with combination of ondansetron and either droperidol or dexamethasone [197, 198]. For PONV treatment, 5-hydroxytryptamine receptor antagonists are the only drugs that have been adequately studied and therefore should be preferred as first choice [199].
Summary and Recommendation
Prophylaxis in high risk patients can reduce the incidence of PONV. The use of a combination therapy is recommended. If PONV occurs, therapy with 5-hydroxytryptamine receptor antagonists should be preferred.
Evidence Level: Low (extrapolated)
Recommendation Grade: Strong
Beta-blockade
The role of beta-blockade for reduction in cardiac morbidity after surgery has been studied extensively. However, no randomized study specifically addressed esophagectomy.
A randomized multicenter trial included 8351 patients who underwent non-cardiac surgery with patients assigned to have extended-release metoprolol in the perioperative period with controls (POISE Trial) [200]. Beta-blockade reduced the risk of myocardial infarction, but there were significantly more strokes and deaths in the metoprolol group. There were also more patients that died of sepsis or infection. A subsequent meta-analysis of 9 trials including 10 529 patients showed that starting beta-blockade before surgery caused a 27% risk increase in 30-day all-cause mortality. Non-fatal myocardial infarction was reduced, at the expense of increased stroke and hypotension [201].
The discrepancy seems to lie with cardiac risk stratification. In one multicenter retrospective study using propensity-matched patients undergoing non-cardiac, non-vascular surgery, perioperative beta-blocker exposure was associated with lower 30-day all-cause mortality in patients with 2 or more Revised Cardiac Risk Index factors. Beta-blocker exposure was also associated with a lower rate of non-fatal Q-wave infarction or cardiac arrest, but again this was limited to patients undergoing non-vascular surgery [202]. This dependency on cardiac risk was reaffirmed by a recent large retrospective study [203].
A systematic review by the American College of Cardiology/American Heart Association Task Force on Practice Guidelines as well as a recent Cochrane review also concluded that there were beneficial effects of beta-blocker on non-fatal myocardial infarction and supraventricular arrhythmias, but it increases hypotension, bradycardia, stroke and all-cause mortality in non-cardiac surgery [204, 205].
Summary and Recommendation
Prophylactic beta-blockage for non-cardiac surgery reduces the incidence of postoperative myocardial infarction and supraventricular arrhythmias, but may potentially increase stroke, hypotension, bradycardia and even death. The beneficial effects seem to be cardiac-risk related, and are only seen in those with moderate to high cardiac risk. Current evidence supports continuing beta-blockers in the peri-operative period in those who are chronically on beta-blockers and to prescribe beta-blockers for high-risk patients with coronary artery disease undergoing high-risk non-cardiac operations.
Evidence Level: Moderate
Recommendation Grade: Strong
Prophylaxis of atrial dysrhythmia
Postoperative cardiac dysrhythmias after esophagectomy are relatively common, and it is often considered a self-limited entity. However, recent international multicenter data reported postoperative atrial dysrhythmias requiring interventions have an incidence of 14.5% [206]. New-onset postoperative atrial fibrillation is the most common perioperative arrhythmia. Worsening of preexisting arrhythmia is also common for patients undergoing esophagectomy. Although this complication can happen in isolation often the atrial fibrillation is often associated with other complications. Risk stratification scores to identify the subgroups with higher probability for postoperative atrial fibrillation have been used in non-cardiac thoracic surgery.
A propensity score-matched analysis of 254 patients showed reduction in atrial fibrillation incidence in the treatment group that received IV amiodarone prophylaxis with no significant differences noted between the amiodarone and control groups in median postoperative length of hospital stay or in the incidence of pulmonary complications or mortality. However, there was a significantly higher incidence of adverse effects in the amiodarone group, including hypotension requiring treatment, bradycardia and QT interval prolongation [207].
A randomized control study of 80 patients undergoing esophagectomy also showed a reduction in postoperative atrial fibrillation, but not in length of stay [208]. This study had incidence of atrial fibrillation of 40% in the control group which was significantly higher than the 14.5% reported in the recent multicenter prospective assessment, while in the amiodarone prophylaxis group 15% incidence was noted.
Although many guidelines and publications focused on non-cardiac thoracic surgery and postoperative cardiac arrhythmia prophylaxis they are not necessarily translatable to esophagectomy patients.
Summary and Recommendation
Prophylactic amiodarone may reduce the incidence of postoperative atrial fibrillation but current evidence does not support reduction in length of stay, overall morbidity or mortality in patients undergoing esophagectomy.
Perioperative cardiac rhythm management strategies should be patient specific, aimed to reduce the modifiable risk factors and prompt recognition and treatment of associated or contributory complications.
Evidence Level: Moderate
Recommendation Grade: Moderate
Antithrombotic prophylaxis
Esophagectomy is associated with significantly high risk of symptomatic venous thromboembolism (VTE) [209]. The prevention of VTE consists of mechanical and pharmacological measures, which increase their effectiveness when applied together [210]. With regard to mechanical measures, elastic stockings are as effective as pneumatic compression [211]. The use of low molecular weight heparin (LMWH) demonstrates the same effectiveness of unfractionated heparin with a reduced risk of bleeding [212] and with a better compliance. A randomized clinical trial comparing VTE incidence in LMWH once-a-day patients with twice-a-day patients showed an advantage for the latter group without an increased risk of bleeding [213]. Injections are usually started 2–12 h before surgery and should be continued for 4 weeks after the operation [214]. The use of LMWH in relation to the epidural catheter is based on its dosing frequency. Epidural placement must be delayed at least 12 h from the last preoperative dose of prophylactic LMWH or 24 h from the last therapeutic dose of LMWH (e.g., 1 mg/kg enoxaparin). For once-daily postoperative dosing, the first LMWH should be given no sooner than 12 h from epidural placement. The second dose must be given no sooner than 24 h after the first dose. The epidural catheter should be removed at the trough of LMWH activity, and the next dose delayed for at least 4 h after catheter removal. For twice-daily postoperative dosing, the epidural catheter must be removed before the first LMWH dose, which itself must not be given until 4 h after catheter removal (i.e., epidural catheters are incompatible with twice daily LMWH dosing) [215].
Summary and Recommendation
Antithrombotic prophylaxis with LMWH, together with mechanical measures, reduce the risk of VTE. Treatment should be started 2–12 h before the operation and should continue for 4 weeks after the operation. Epidural catheters should be placed no sooner than 12 h from the last LMWH dose. LMWH should not be given until at least 4 h have passed after epidural catheter removal.
Evidence Level: High
Recommendation Grade: Strong
Hypothermia
Meta-analyses and randomized controlled trials have shown that intraoperative hypothermia is correlated with occurrence of wound infection [216], cardiac morbidities [217], bleeding and transfusion requirement [217, 218], shivering (which increases oxygen consumption), and prolonged hospital stay [216]. The effects are apparent when body temperature falls below 36 °C or 96.8 °F. Mild hypothermia is common during esophagectomy; the operation is prolonged and two body cavities (abdomen and chest) are entered.
Few studies have specifically studied esophagectomy patients. A recent retrospective study showed that intraoperative hypothermia (defined as urinary bladder temperate of less than 35 °C or 95 °F) was an independent factor for early postoperative events on multivariate analysis [219].
Measures to avoid hypothermia include pre-emptive skin warming, maintenance of operating room temperature at 21 °C or 69.8 °F, humidification of airway, intravenous fluid warming, applying blanket for skin coverage, forced-air convective warming system, circulating water mattresses, circulating water garments, or combinations of methods [220, 221]. A recently published randomized controlled trial compared saline versus amino acid infusion 30 min preanesthesia to the end of the thoracic procedure during video-assisted thoracoscopic esophagectomy. Administration of amino acids resulted in a significant increase in core body temperature [222].
Summary and Recommendation
Intraoperative hypothermia leads to adverse postoperative events. Measures to maintain normothermia, such as forced-air blankets, warming mattress or circulating-water garment systems, use of warm intravenous fluid should be recommended. Temperature monitoring with an aim of maintaining core temperature of above 36 °C or 96.8 °F is desirable.
Evidence Level: High
Recommendation Grade: Strong
Postoperative glycemic control
Patients with diabetes mellitus are more susceptible to postsurgical and other hospital-acquired infections. Furthermore, insulin resistance has been associated with morbidity and mortality after major GI surgery [223,224,225]. A landmark study in 2001 demonstrated that aggressive treatment of postoperative hyperglycemia in the cardiac surgical ICU significantly reduced rates of infection, morbidity and mortality, and 1-year survival [226]. However, hypoglycemia remains a risk factor. Many of the steps in enhanced recovery protocols reduce postoperative insulin resistance and allow for tighter glycemic control. Target threshold for glucose levels of >10–12 mmol/L or 180–216 mg/dL increases the risk of osmotic diuresis and can cause fluid balance disturbances. Hence, a target of 12 mmol/L or 216 mg/dL should therefore be regarded as a limit in any clinical setting [227].
Summary and Recommendation
Reducing insulin resistance and treatment of excessive hyperglycemia is strongly associated with improved outcomes. A multi modal approach to minimize the metabolic stress of surgery is recommended to reduce insulin resistance and hyperglycemia. Preoperative carbohydrate treatment, epidural anesthesia, minimally invasive surgical techniques and early enteral feeding are recommended.
Blood glucose levels above 10 mmol/L (180 mg/dL) should be treated.
Evidence Level: Moderate
Recommendation Grade: Strong
Bowel stimulation
Postoperative ileus (POI) is a common stress response to major gastrointestinal surgery, leading to abdominal pain, postoperative nausea and vomiting, and delay to oral intake [228]. An effective ERAS program must therefore include techniques to minimize POI and encourage prompt return to normal bowel function. There are no effective prokinetics available for the treatment of POI since cisapride was withdrawn [229]. Metoclopramide, although widely used, has no proven effect on POI. There is some evidence in abdominal surgery that chewing gum can reduce postoperative ileus by stimulating early recovery of gastrointestinal function, but most of the evidence exists for cesarean section or colorectal surgery. In a recent Cochrane review [230] of randomized controlled trials of the use of chewing gum in abdominal surgery, the authors identified some evidence of benefit of postoperative chewing gum, but none of the trials included patients undergoing esophagectomy. The use of oral laxatives such as magnesium sulfate or bisacodyl may stimulate early gastrointestinal transit after colonic resections, but they have not been evaluated following esophagectomy [228]. Glycerin suppositories are safe and cheap, and often used in esophagectomy ERAS programs to stimulate bowel action, but likewise have not been evaluated in this setting. The appropriate use of opioid-sparing pain management and maintaining a near-zero fluid balance are associated with an enhanced return of bowel activity after abdominal surgery [231,232,233] and are an essential part of perioperative care.
Summary and Recommendation
A multimodal approach with epidural analgesia and near-zero fluid balance is recommended. Oral laxatives and chewing gum given postoperatively are safe and may accelerate gastrointestinal transit.
Evidence Level: Low
Recommendation Grade: Weak
Foley catheter management
The longer the use of bladder drainage, the higher the potential for urinary infection; thus, the aim is to minimize the length of time urinary drainage is used. Following an esophagectomy patients are likely to have an epidural catheter and a need for urinary drainage in the immediate postoperative period.
Two cohort studies have assessed the timing of removal of a urethral catheter in patients following an open thoracotomy, who have an epidural catheter in place. A study of 61 patients were assessed following removal of the urethral catheter within 3 days while the epidural was still in place. The definition of urinary retention was more than 500 mL in the bladder. The re-insertion rate was 6.6% in male patients [234]. A larger comparative study assessed 101 patients who had the urethral catheter removed at 48 h post-surgery. Re-insertion was required in 26.7% compared with 12.4% in a historic cohort of 218 patients who had the urethral catheter removed 6 h after the epidural was removed. There was no difference in urinary infection rates [235].
Two RCTs have addressed this issue in patients who have had an open thoracotomy with an epidural catheter inserted. The first trial had 215 patients. (10 had an esophagectomy.) Patients were randomized to removal of the catheter on postoperative day (POD) one, compared with standard urethral catheter removal occurring after the epidural catheter had been removed. The primary outcome assessment was urinary infection rate. There was no significant difference in the need to re-insert and remove a urethral catheter, with rate being 7.6% for POD 1 group compared with 1.8% for standard treatment (p = 0.09). In the POD 1 group three patients required longer-term catheterization. The standard group had a urinary infection rate of 14% compared with 2% for the POD 1 removal group with infections higher in older patients (60 vs 69 years) [236].
In the most recent RCT containing 247 patients (esophagectomy 17%), patients were randomized to removal of the urinary catheter on POD 2 or removal 6 h after the epidural had been removed. Re-insertion occurred in 19 patients (18 males) and was higher in the POD 2 group with insertion and removal rates of 21.5% vs 9.5% (p = 0.009), and reinsertion/leave urethral catheter rates of 12.4% vs 3.2% (p = 0.006). There was no difference in females. Univariate analysis showed a higher reinsertion following esophagectomy and major pulmonary resection [237].
All the studies involving early removal of the urinary catheter, while the epidural was in place, had strict protocols for patient and bladder assessment following removal of the urinary catheter to allow early, timely catheterization if there was evidence of urinary retention.
The rate of urinary infection following the use of urethral catheterization compared with suprapubic catheterization, to drain the bladder, has been assessed in a meta-analysis. The analysis included six RCT and reported double the urinary infection rate for urethral catheterization. Suprapubic drainage was also reported to be more acceptable to patients [238]. The majority of the patients in these studies had catheterization for 4 days or longer; hence, the implication for shorter periods is not clear.
Summary and Recommendation
Expeditious removal of urinary catheters following surgery can positively impact rates of postoperative urinary tract infections. However, in patients that have had a thoracotomy and who have an epidural catheter in place, removal of the urinary catheter prior to removal of the epidural catheter carries a significant risk for urinary catheter replacement notably in males.
Catheter removal within 48 h has higher incidence of reinsertion for urinary retention. Early removal of urinary catheters is worthy of consideration but there needs to be strict protocols for patient bladder assessment of the need for catheter reinsertion.
Evidence Level: High
Recommendation Grade: Strong
Urinary infection rates are lower with the use of a suprapubic catheter if urinary drainage required for longer than 4 days.
Evidence Level: High
Recommendation Grade: Moderate
References
Kehlet H, Mogensen T (1999) Hospital stay of 2 days after open sigmoidectomy with a multimodal rehabilitation programme. Br J Surg 86:227–230
Fearon KC, Ljungqvist O, Von MM et al (2005) Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr 24:466–477
Ljungqvist O, Scott M, Fearon KC (2017) Enhanced recovery after surgery: a review. JAMA Surg 152:292–298
Lassen K, Soop M, Nygren J et al (2009) Consensus review of optimal perioperative care in colorectal surgery: Enhanced Recovery After Surgery (ERAS) Group recommendations. Arch Surg 144:961–969
Mortensen K, Nilsson M, Slim K et al (2014) Consensus guidelines for enhanced recovery after gastrectomy: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Br J Surg 101:1209–1229
Thorell A, MacCormick AD, Awad S et al (2016) Guidelines for perioperative care in bariatric surgery: Enhanced Recovery After Surgery (ERAS) Society recommendations. World J Surg 40:2065–2083. https://doi.org/10.1007/s00268-016-3492-3
Melloul E, Hubner M, Scott M et al (2016) Guidelines for perioperative care for liver surgery: Enhanced Recovery After Surgery (ERAS) Society recommendations. World J Surg 40:2425–2440. https://doi.org/10.1007/s00268-016-3700-1
Nelson G, Altman AD, Nick A et al (2016) Guidelines for pre- and intra-operative care in gynecologic/oncology surgery: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations, part I. Gynecol Oncol 140:313–322
Nelson G, Altman AD, Nick A et al (2016) Guidelines for postoperative care in gynecologic/oncology surgery: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations, part II. Gynecol Oncol 140:323–332
Low DE, Alderson D, Cecconello I et al (2015) International consensus on standardization of data collection for complications associated with esophagectomy: Esophagectomy Complications Consensus Group (ECCG). Ann Surg 262:286–294
Finks JF, Osborne NH, Birkmeyer JD (2011) Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med 364:2128–2137
Walters DM, McMurry TL, Isbell JM et al (2014) Understanding mortality as a quality indicator after esophagectomy. Ann Thorac Surg 98:506–511
Guyatt GH, Oxman AD, Vist GE et al (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336:924–926
Gillissen F, Ament SM, Maessen JM et al (2015) Sustainability of an enhanced recovery after surgery program (ERAS) in colonic surgery. World J Surg 39:526–533. https://doi.org/10.1007/s00268-014-2744-3
Hammond JS, Humphries S, Simson N et al (2014) Adherence to enhanced recovery after surgery protocols across a high-volume gastrointestinal surgical service. Dig Surg 31:117–122
Gustafsson UO, Hausel J, Thorell A et al (2011) Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Arch Surg 146:571–577
ERAS Compliance Group (2015) The impact of enhanced recovery protocol compliance on elective colorectal cancer resection: results from an international registry. Ann Surg 261:1153–1159
Martin TD, Lorenz T, Ferraro J et al (2016) Newly implemented enhanced recovery pathway positively impacts hospital length of stay. Surg Endosc 30:4019–4028
Gustafsson UO, Scott MJ, Schwenk W et al (2013) Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS((R))) Society recommendations. World J Surg 37:259–284. https://doi.org/10.1007/s00268-012-1772-0
Pecorelli N, Hershorn O, Baldini G et al (2017) Impact of adherence to care pathway interventions on recovery following bowel resection within an established enhanced recovery program. Surg Endosc 31:1760–1771
Lee L, Li C, Robert N et al (2013) Economic impact of an enhanced recovery pathway for oesophagectomy. Br J Surg 100:1326–1334
Feldheiser A, Aziz O, Baldini G et al (2016) Enhanced Recovery After Surgery (ERAS) for gastrointestinal surgery, part 2: consensus statement for anaesthesia practice. Acta Anaesthesiol Scand 60:289–334
Scott MJ, Baldini G, Fearon KC et al (2015) Enhanced Recovery After Surgery (ERAS) for gastrointestinal surgery, part 1: pathophysiological considerations. Acta Anaesthesiol Scand 59:1212–1231
Porteous GH, Neal JM, Slee A et al (2015) A standardized anesthetic and surgical clinical pathway for esophageal resection: impact on length of stay and major outcomes. Reg Anesth Pain Med 40:139–149
Findlay JM, Gillies RS, Millo J et al (2014) Enhanced recovery for esophagectomy: a systematic review and evidence-based guidelines. Ann Surg 259:413–431
Gemmill EH, Humes DJ, Catton JA (2015) Systematic review of enhanced recovery after gastro-oesophageal cancer surgery. Ann R Coll Surg Engl 97:173–179
Li C, Ferri LE, Mulder DS et al (2012) An enhanced recovery pathway decreases duration of stay after esophagectomy. Surgery 152:606–614
Underwood TJ, Noble F, Madhusudan N et al (2017) The development, application and analysis of an enhanced recovery programme for major oesophagogastric resection. J Gastrointest Surg 21:614–621
Markar SR, Karthikesalingam A, Low DE (2015) Enhanced recovery pathways lead to an improvement in postoperative outcomes following esophagectomy: systematic review and pooled analysis. Dis Esophagus 28:468–475
Bower MR, Martin RC (2009) Nutritional management during neoadjuvant therapy for esophageal cancer. J Surg Oncol 100:82–87
Weimann A, Braga M, Carli F et al (2017) ESPEN guideline: clinical nutrition in surgery. Clin Nutr 36:623–650
Ha L, Hauge T, Spenning AB et al (2010) Individual, nutritional support prevents undernutrition, increases muscle strength and improves QoL among elderly at nutritional risk hospitalized for acute stroke: a randomized, controlled trial. Clin Nutr 29:567–573
Ligthart-Melis GC, Weijs PJ, te Boveldt ND et al (2013) Dietician-delivered intensive nutritional support is associated with a decrease in severe postoperative complications after surgery in patients with esophageal cancer. Dis Esophagus 26:587–593
Odelli C, Burgess D, Bateman L et al (2005) Nutrition support improves patient outcomes, treatment tolerance and admission characteristics in oesophageal cancer. Clin Oncol (R Coll Radiol) 17:639–645
Rufenacht U, Ruhlin M, Wegmann M et al (2010) Nutritional counseling improves quality of life and nutrient intake in hospitalized undernourished patients. Nutrition 26:53–60
Okamoto Y, Okano K, Izuishi K et al (2009) Attenuation of the systemic inflammatory response and infectious complications after gastrectomy with preoperative oral arginine and omega-3 fatty acids supplemented immunonutrition. World J Surg 33:1815–1821. https://doi.org/10.1007/s00268-009-0140-1
Heys SD, Walker LG, Smith I et al (1999) Enteral nutritional supplementation with key nutrients in patients with critical illness and cancer: a meta-analysis of randomized controlled clinical trials. Ann Surg 229:467–477
Zhang Y, Gu Y, Guo T et al (2012) Perioperative immunonutrition for gastrointestinal cancer: a systematic review of randomized controlled trials. Surg Oncol 21:e87–e95
Mabvuure NT, Roman A, Khan OA (2013) Enteral immunonutrition versus standard enteral nutrition for patients undergoing oesophagogastric resection for cancer. Int J Surg 11:122–127
Sultan J, Griffin SM, Di Franco F et al (2012) Randomized clinical trial of omega-3 fatty acid-supplemented enteral nutrition versus standard enteral nutrition in patients undergoing oesophagogastric cancer surgery. Br J Surg 99:346–355
Ryan AM, Reynolds JV, Healy L et al (2009) Enteral nutrition enriched with eicosapentaenoic acid (EPA) preserves lean body mass following esophageal cancer surgery: results of a double-blinded randomized controlled trial. Ann Surg 249:355–363
Nagano T, Fujita H, Tanaka T et al (2013) Randomized controlled trial comparing antioxidant-enriched enteral nutrition with immune-enhancing enteral nutrition after esophagectomy for cancer: a pilot study. Surg Today 43:1240–1249
Healy LA, Ryan A, Doyle SL et al (2017) Does prolonged enteral feeding with supplemental omega-3 fatty acids impact on recovery post-esophagectomy: results of a randomized double-blind trial. Ann Surg 266:720–728
Taylor C, Munro AJ, Glynne-Jones R et al (2010) Multidisciplinary team working in cancer: what is the evidence? BMJ 340:c951
Davies AR, Deans DA, Penman I et al (2006) The multidisciplinary team meeting improves staging accuracy and treatment selection for gastro-esophageal cancer. Dis Esophagus 19:496–503
Stephens MR, Lewis WG, Brewster AE et al (2006) Multidisciplinary team management is associated with improved outcomes after surgery for esophageal cancer. Dis Esophagus 19:164–171
Taplin SH, Weaver S, Salas E et al (2015) Reviewing cancer care team effectiveness. J Oncol Pract 11:239–246
Blazeby JM, Wilson L, Metcalfe C et al (2006) Analysis of clinical decision-making in multi-disciplinary cancer teams. Ann Oncol 17:457–460
Schmidt HM, Roberts JM, Bodnar AM et al (2015) Thoracic multidisciplinary tumor board routinely impacts therapeutic plans in patients with lung and esophageal cancer: a prospective cohort study. Ann Thorac Surg 99:1719–1724
Fennell ML, Das IP, Clauser S et al (2010) The organization of multidisciplinary care teams: modeling internal and external influences on cancer care quality. J Natl Cancer Inst Monogr 2010:72–80
Smith TB, Stonell C, Purkayastha S et al (2009) Cardiopulmonary exercise testing as a risk assessment method in non cardio-pulmonary surgery: a systematic review. Anaesthesia 64:883–893
Carli F, Silver JK, Feldman LS et al (2017) Surgical prehabilitation in patients with cancer: state-of-the-science and recommendations for future research from a panel of subject matter experts. Phys Med Rehabil Clin N Am 28:49–64
Carli F, Charlebois P, Stein B et al (2010) Randomized clinical trial of prehabilitation in colorectal surgery. Br J Surg 97:1187–1197
Gillis C, Li C, Lee L et al (2014) Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology 121:937–947
Dunne DF, Jack S, Jones RP et al (2016) Randomized clinical trial of prehabilitation before planned liver resection. Br J Surg 103:504–512
Le Roy B, Pereira B, Bouteloup C et al (2016) Effect of prehabilitation in gastro-oesophageal adenocarcinoma: study protocol of a multicentric, randomised, control trial-the PREHAB study. BMJ Open 6:e012876
Ikebe M, Morita M, Yamamoto M et al (2016) Neoadjuvant therapy for advanced esophageal cancer: the impact on surgical management. Gen Thorac Cardiovasc Surg 64:386–394
Medical Research Council Oesophageal Cancer Working Group (2002) Surgical resection with or without preoperative chemotherapy in oesophageal cancer: a randomised controlled trial. Lancet 359:1727–1733
Cunningham D, Allum WH, Stenning SP et al (2006) Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med 355:11–20
Kelsen DP, Ginsberg R, Pajak TF et al (1998) Chemotherapy followed by surgery compared with surgery alone for localized esophageal cancer. N Engl J Med 339:1979–1984
Shapiro J, van Lanschot JJ, Hulshof MC et al (2015) Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol 16:1090–1098
Shapiro J, Van HP, Lingsma HF et al (2014) Prolonged time to surgery after neoadjuvant chemoradiotherapy increases histopathological response without affecting survival in patients with esophageal or junctional cancer. Ann Surg 260:807–813
Lin G, Han SY, Xu YP et al (2016) Increasing the interval between neoadjuvant chemoradiotherapy and surgery in esophageal cancer: a meta-analysis of published studies. Dis Esophagus 29:1107–1114
Biere SS, van Berge Henegouwen MI, Maas KW et al (2012) Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 379:1887–1892
Maas KW, Cuesta MA, van Berge Henegouwen MI et al (2015) Quality of life and late complications after minimally invasive compared to open esophagectomy: results of a randomized trial. World J Surg 39:1986–1993. https://doi.org/10.1007/s00268-015-3100-y
Nagpal K, Ahmed K, Vats A et al (2010) Is minimally invasive surgery beneficial in the management of esophageal cancer? A meta-analysis. Surg Endosc 24:1621–1629
Guo W, Ma X, Yang S et al (2016) Combined thoracoscopic-laparoscopic esophagectomy versus open esophagectomy: a meta-analysis of outcomes. Surg Endosc 30:3873–3881
Sgourakis G, Gockel I, Radtke A et al (2010) Minimally invasive versus open esophagectomy: meta-analysis of outcomes. Dig Dis Sci 55:3031–3040
Dantoc M, Cox MR, Eslick GD (2012) Evidence to support the use of minimally invasive esophagectomy for esophageal cancer: a meta-analysis. Arch Surg 147:768–776
Seesing MFJ, Gisbertz SS, Goense L et al (2017) A propensity score matched analysis of open versus minimally invasive transthoracic esophagectomy in the Netherlands. Ann Surg 266:839–846
ESMO 2017 Press Release: MIRO Trial: 3-year outcomes favour laparoscopic surgery for oesophageal cancer. Sept. 5, 2017. http://www.esmo.org/Press-Office/Press-Releases/MIRO-Trial-3-year-Outcomes-Favour-Laparoscopic-Surgery-for-Oesophageal-Cancer. European Society for Medical Oncology. Accessed 16 Feb 2018
Urschel JD (2001) Does the interponat affect outcome after esophagectomy for cancer? Dis Esophagus 14:124–130
DeMeester SR (2001) Colon interposition following esophagectomy. Dis Esophagus 14:169–172
Gust L, Ouattara M, Coosemans W et al (2016) European perspective in thoracic surgery-eso-coloplasty: when and how? J Thorac Dis 8:S387–S398
Watanabe M, Mine S, Nishida K et al (2016) Reconstruction after esophagectomy for esophageal cancer patients with a history of gastrectomy. Gen Thorac Cardiovasc Surg 64:457–463
Akkerman RD, Haverkamp L, van Hillegersberg R et al (2014) Surgical techniques to prevent delayed gastric emptying after esophagectomy with gastric interposition: a systematic review. Ann Thorac Surg 98:1512–1519
Urschel JD, Blewett CJ, Young JE et al (2002) Pyloric drainage (pyloroplasty) or no drainage in gastric reconstruction after esophagectomy: a meta-analysis of randomized controlled trials. Dig Surg 19:160–164
Cerfolio RJ, Bryant AS, Canon CL et al (2009) Is botulinum toxin injection of the pylorus during Ivor Lewis [corrected] esophagogastrectomy the optimal drainage strategy? J Thorac Cardiovasc Surg 137:565–572
Oezcelik A, DeMeester SR, Hindoyan K et al (2011) Circular stapled pyloroplasty: a fast and effective technique for pyloric disruption during esophagectomy with gastric pull-up. Dis Esophagus 24:423–429
Hiranyatheb P, Osugi H (2015) Radical lymphadenectomy in esophageal cancer: from the past to the present. Dis Esophagus 28:68–77
Altorki N, Kent M, Ferrara C et al (2002) Three-field lymph node dissection for squamous cell and adenocarcinoma of the esophagus. Ann Surg 236:177–183
Choi HK, Law S, Chu KM et al (1998) The value of neck drain in esophageal surgery: a randomized trial. Dis Esophagus 11:40–42
Tang H, Xue L, Hong J et al (2012) A method for early diagnosis and treatment of intrathoracic esophageal anastomotic leakage: prophylactic placement of a drainage tube adjacent to the anastomosis. J Gastrointest Surg 16:722–727
Perry Y, Towe CW, Kwong J et al (2015) Serial drain amylase can accurately detect anastomotic leak after esophagectomy and may facilitate early discharge. Ann Thorac Surg 100:2041–2046
Berkelmans GH, Kouwenhoven EA, Smeets BJ et al (2015) Diagnostic value of drain amylase for detecting intrathoracic leakage after esophagectomy. World J Gastroenterol 21:9118–9125
Weijs TJ, Kumagai K, Berkelmans GH et al (2017) Nasogastric decompression following esophagectomy: a systematic literature review and meta-analysis. Dis Esophagus 30:1–8
Mistry RC, Vijayabhaskar R, Karimundackal G et al (2012) Effect of short-term vs prolonged nasogastric decompression on major postesophagectomy complications: a parallel-group, randomized trial. Arch Surg 147:747–751
Shackcloth MJ, McCarron E, Kendall J et al (2006) Randomized clinical trial to determine the effect of nasogastric drainage on tracheal acid aspiration following oesophagectomy. Br J Surg 93:547–552
Refai M, Brunelli A, Salati M et al (2012) The impact of chest tube removal on pain and pulmonary function after pulmonary resection. Eur J Cardiothorac Surg 41:820–822
Lagarde SM, Omloo JM, Ubbink DT et al (2007) Predictive factors associated with prolonged chest drain production after esophagectomy. Dis Esophagus 20:24–28
Hessami MA, Najafi F, Hatami S (2009) Volume threshold for chest tube removal: a randomized controlled trial. J Inj Violence Res 1:33–36
Younes RN, Gross JL, Aguiar S et al (2002) When to remove a chest tube? A randomized study with subsequent prospective consecutive validation. J Am Coll Surg 195:658–662
Cerfolio RJ, Bryant AS (2008) Results of a prospective algorithm to remove chest tubes after pulmonary resection with high output. J Thorac Cardiovasc Surg 135:269–273
Johansson J, Lindberg CG, Johnsson F et al (1998) Active or passive chest drainage after oesophagectomy in 101 patients: a prospective randomized study. Br J Surg 85:1143–1146
Alex J, Ansari J, Bahalkar P et al (2003) Comparison of the immediate postoperative outcome of using the conventional two drains versus a single drain after lobectomy. Ann Thorac Surg 76:1046–1049
Gomez-Caro A, Roca MJ, Torres J et al (2006) Successful use of a single chest drain postlobectomy instead of two classical drains: a randomized study. Eur J Cardiothorac Surg 29:562–566
Fong YM, Marano MA, Barber A et al (1989) Total parenteral nutrition and bowel rest modify the metabolic response to endotoxin in humans. Ann Surg 210:449–456
Mazaki T, Ebisawa K (2008) Enteral versus parenteral nutrition after gastrointestinal surgery: a systematic review and meta-analysis of randomized controlled trials in the English literature. J Gastrointest Surg 12:739–755
Seike J, Tangoku A, Yuasa Y et al (2011) The effect of nutritional support on the immune function in the acute postoperative period after esophageal cancer surgery: total parenteral nutrition versus enteral nutrition. J Med Invest 58:75–80
Aiko S, Yoshizumi Y, Sugiura Y et al (2001) Beneficial effects of immediate enteral nutrition after esophageal cancer surgery. Surg Today 31:971–978
Baigrie RJ, Devitt PG, Watkin DS (1996) Enteral versus parenteral nutrition after oesophagogastric surgery: a prospective randomized comparison. Aust N Z J Surg 66:668–670
Myers JG, Page CP, Stewart RM et al (1995) Complications of needle catheter jejunostomy in 2,022 consecutive applications. Am J Surg 170:547–550
Han-Geurts IJ, Hop WC, Verhoef C et al (2007) Randomized clinical trial comparing feeding jejunostomy with nasoduodenal tube placement in patients undergoing oesophagectomy. Br J Surg 94:31–35
Weijs TJ, Berkelmans GH, Nieuwenhuijzen GA et al (2015) Routes for early enteral nutrition after esophagectomy: a systematic review. Clin Nutr 34:1–6
Holte K, Foss NB, Svensen C et al (2004) Epidural anesthesia, hypotension, and changes in intravascular volume. Anesthesiology 100:281–286
Casado D, Lopez F, Marti R (2010) Perioperative fluid management and major respiratory complications in patients undergoing esophagectomy. Dis Esophagus 23:523–528
Wei S, Tian J, Song X et al (2008) Association of perioperative fluid balance and adverse surgical outcomes in esophageal cancer and esophagogastric junction cancer. Ann Thorac Surg 86:266–272
Abbas SM, Hill AG (2008) Systematic review of the literature for the use of oesophageal Doppler monitor for fluid replacement in major abdominal surgery. Anaesthesia 63:44–51
Rahbari NN, Zimmermann JB, Schmidt T et al (2009) Meta-analysis of standard, restrictive and supplemental fluid administration in colorectal surgery. Br J Surg 96:331–341
Rollins KE, Lobo DN (2016) Intraoperative goal-directed fluid therapy in elective major abdominal surgery: a meta-analysis of randomized controlled trials. Ann Surg 263:465–476
Varadhan KK, Lobo DN (2010) A meta-analysis of randomised controlled trials of intravenous fluid therapy in major elective open abdominal surgery: getting the balance right. Proc Nutr Soc 69:488–498
Carney A, Dickinson M (2015) Anesthesia for esophagectomy. Anesthesiol Clin 33:143–163
Bundgaard-Nielsen M, Secher NH, Kehlet H (2009) ‘Liberal’ vs. ‘restrictive’ perioperative fluid therapy: a critical assessment of the evidence. Acta Anaesthesiol Scand 53:843–851
Puckett JR, Pickering JW, Palmer SC et al (2017) Low versus standard urine output targets in patients undergoing major abdominal surgery: a randomized noninferiority trial. Ann Surg 265:874–881
Shaw AD, Bagshaw SM, Goldstein SL et al (2012) Major complications, mortality, and resource utilization after open abdominal surgery: 0.9% saline compared to Plasma-Lyte. Ann Surg 255:821–829
Senagore AJ, Emery T, Luchtefeld M et al (2009) Fluid management for laparoscopic colectomy: a prospective, randomized assessment of goal-directed administration of balanced salt solution or hetastarch coupled with an enhanced recovery program. Dis Colon Rectum 52:1935–1940
Beck-Schimmer B, Bonvini JM, Braun J et al (2016) Which anesthesia regimen is best to reduce morbidity and mortality in lung surgery? A multicenter randomized controlled trial. Anesthesiology 125:313–321
Punjasawadwong Y, Boonjeungmonkol N, Phongchiewboon A (2007) Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev 4:CD003843
Brull SJ, Murphy GS (2010) Residual neuromuscular block: lessons unlearned. Part II: methods to reduce the risk of residual weakness. Anesth Analg 111:129–140
Guay J, Ochroch EA (2015) Intraoperative use of low volume ventilation to decrease postoperative mortality, mechanical ventilation, lengths of stay and lung injury in patients without acute lung injury. Cochrane Database Syst Rev CD011151
Guldner A, Kiss T, Serpa NA et al (2015) Intraoperative protective mechanical ventilation for prevention of postoperative pulmonary complications: a comprehensive review of the role of tidal volume, positive end-expiratory pressure, and lung recruitment maneuvers. Anesthesiology 123:692–713
Serpa Neto A, Hemmes SN, Barbas CS et al (2015) Protective versus conventional ventilation for surgery: a systematic review and individual patient data meta-analysis. Anesthesiology 123:66–78
Michelet P, D’Journo XB, Roch A et al (2006) Protective ventilation influences systemic inflammation after esophagectomy: a randomized controlled study. Anesthesiology 105:911–919
Verhage RJ, Boone J, Rijkers GT et al (2014) Reduced local immune response with continuous positive airway pressure during one-lung ventilation for oesophagectomy. Br J Anaesth 112:920–928
Lohser J, Slinger P (2015) Lung injury after one-lung ventilation: a review of the pathophysiologic mechanisms affecting the ventilated and the collapsed lung. Anesth Analg 121:302–318
Amato MB, Meade MO, Slutsky AS et al (2015) Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 372:747–755
Neto AS, Hemmes SN, Barbas CS et al (2016) Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: a meta-analysis of individual patient data. Lancet Respir Med 4:272–280
Robertson SA, Skipworth RJ, Clarke DL et al (2006) Ventilatory and intensive care requirements following oesophageal resection. Ann R Coll Surg Engl 88:354–357
Chandrashekar MV, Irving M, Wayman J et al (2003) Immediate extubation and epidural analgesia allow safe management in a high-dependency unit after two-stage oesophagectomy. Results of eight years of experience in a specialized upper gastrointestinal unit in a district general hospital. Br J Anaesth 90:474–479
Cerfolio RJ, Bryant AS, Bass CS et al (2004) Fast tracking after Ivor Lewis esophagogastrectomy. Chest 126:1187–1194
Li C, Ferri LE, Mulder DS et al (2012) An enhanced recovery pathway decreases duration of stay after esophagectomy. Surgery 152:606–614
Cao S, Zhao G, Cui J et al (2013) Fast-track rehabilitation program and conventional care after esophagectomy: a retrospective controlled cohort study. Support Care Cancer 21:707–714
Wunsch H, Gershengorn HB, Cooke CR et al (2016) Use of intensive care services for medicare beneficiaries undergoing major surgical procedures. Anesthesiology 124:899–907
Flisberg P, Tornebrandt K, Walther B et al (2001) Pain relief after esophagectomy: thoracic epidural analgesia is better than parenteral opioids. J Cardiothorac Vasc Anesth 15:282–287
Senturk M, Ozcan PE, Talu GK et al (2002) The effects of three different analgesia techniques on long-term postthoracotomy pain. Anesth Analg 94:11–15
Richards ER, Kabir SI, McNaught CE et al (2013) Effect of thoracic epidural anaesthesia on splanchnic blood flow. Br J Surg 100:316–321
Lazar G, Kaszaki J, Abraham S et al (2003) Thoracic epidural anesthesia improves the gastric microcirculation during experimental gastric tube formation. Surgery 134:799–805
Theodorou D, Drimousis PG, Larentzakis A et al (2008) The effects of vasopressors on perfusion of gastric graft after esophagectomy: an experimental study. J Gastrointest Surg 12:1497–1501
Pathak D, Pennefather SH, Russell GN et al (2013) Phenylephrine infusion improves blood flow to the stomach during oesophagectomy in the presence of a thoracic epidural analgesia. Eur J Cardiothorac Surg 44:130–133
Al-Rawi OY, Pennefather SH, Page RD et al (2008) The effect of thoracic epidural bupivacaine and an intravenous adrenaline infusion on gastric tube blood flow during esophagectomy. Anesth Analg 106:884–887
Davies RG, Myles PS, Graham JM (2006) A comparison of the analgesic efficacy and side-effects of paravertebral vs epidural blockade for thoracotomy: a systematic review and meta-analysis of randomized trials. Br J Anaesth 96:418–426
Ding X, Jin S, Niu X et al (2014) A comparison of the analgesia efficacy and side effects of paravertebral compared with epidural blockade for thoracotomy: an updated meta-analysis. PLoS ONE 9:e96233
Baidya DK, Khanna P, Maitra S (2014) Analgesic efficacy and safety of thoracic paravertebral and epidural analgesia for thoracic surgery: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg 18:626–635
Schmidt PC, Ruchelli G, Mackey SC et al (2014) Perioperative Gabapentinoids: choice of agent, dose, timing, and effects on chronic postsurgical pain. Surv Anesthesiol 58:96–97
Laskowski K, Stirling A, McKay WP et al (2011) A systematic review of intravenous ketamine for postoperative analgesia. Can J Anaesth 58:911–923
De Oliveira GSJ, Castro-Alves LJ, Khan JH et al (2013) Perioperative systemic magnesium to minimize postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology 119:178–190
Ryan AM, Rowley SP, Healy LA et al (2006) Post-oesophagectomy early enteral nutrition via a needle catheter jejunostomy: 8-year experience at a specialist unit. Clin Nutr 25:386–393
Xiao-Bo Y, Qiang L, Xiong Q et al (2014) Efficacy of early postoperative enteral nutrition in supporting patients after esophagectomy. Minerva Chir 69:37–46
Mazaki T, Ebisawa K (2008) Enteral versus parenteral nutrition after gastrointestinal surgery: a systematic review and meta-analysis of randomized controlled trials in the English literature. J Gastrointest Surg 12:739–755
Fujita T, Daiko H, Nishimura M (2012) Early enteral nutrition reduces the rate of life-threatening complications after thoracic esophagectomy in patients with esophageal cancer. Eur Surg Res 48:79–84
Convertino VA (1997) Cardiovascular consequences of bed rest: effect on maximal oxygen uptake. Med Sci Sports Exerc 29:191–196
Pashikanti L, Von Ah D (2012) Impact of early mobilization protocol on the medical-surgical inpatient population: an integrated review of literature. Clin Nurse Spec 26:87–94
Kehlet H, Wilmore DW (2002) Multimodal strategies to improve surgical outcome. Am J Surg 183:630–641
Brower RG (2009) Consequences of bed rest. Crit Care Med 37:S422–S428
Lauder CI, Marlow NE, Maddern GJ et al (2010) Systematic review of the impact of volume of oesophagectomy on patient outcome. ANZ J Surg 80:317–323
Markar SR, Karthikesalingam A, Thrumurthy S et al (2012) Volume-outcome relationship in surgery for esophageal malignancy: systematic review and meta-analysis 2000–2011. J Gastrointest Surg 16:1055–1063
Schmidt HM, El Lakis MA, Markar SR et al (2016) Accelerated recovery within standardized recovery pathways after esophagectomy: a prospective cohort study assessing the effects of early discharge on outcomes, readmissions, patient satisfaction, and costs. Ann Thorac Surg 102:931–939
Pearse RM, Moreno RP, Bauer P et al (2012) Mortality after surgery in Europe: a 7 day cohort study. Lancet 380:1059–1065
Gustafsson UO, Hausel J, Thorell A et al (2011) Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Arch Surg 146:571–577
Nelson G, Kiyang LN, Crumley ET et al (2016) Implementation of Enhanced Recovery After Surgery (ERAS) across a provincial healthcare system: the ERAS Alberta colorectal surgery experience. World J Surg 40:1092–1103. https://doi.org/10.1007/s00268-016-3472-7
Thanh NX, Chuck AW, Wasylak T et al (2016) An economic evaluation of the Enhanced Recovery After Surgery (ERAS) multisite implementation program for colorectal surgery in Alberta. Can J Surg 59:415–421
Gustafsson UO, Oppelstrup H, Thorell A et al (2016) Adherence to the ERAS protocol is associated with 5-year survival after colorectal cancer surgery: a retrospective cohort study. World J Surg 40:1741–1747. https://doi.org/10.1007/s00268-016-3460-y
Roulin D, Donadini A, Gander S et al (2013) Cost-effectiveness of the implementation of an enhanced recovery protocol for colorectal surgery. Br J Surg 100:1108–1114
Stergiopoulou A, Birbas K, Katostaras T et al (2007) The effect of interactive multimedia on preoperative knowledge and postoperative recovery of patients undergoing laparoscopic cholecystectomy. Methods Inf Med 46:406–409
McGill University Health Centre Patient Education Office. MUHC patient education guide: esophageal cancer. http://muhcguides.com/module/esophageal. Accessed 13 June 2017
Edward GM, Naald N, Oort FJ et al (2011) Information gain in patients using a multimedia website with tailored information on anaesthesia. Br J Anaesth 106:319–324
Sobanko JF, Da SD, Chiesa Fuxench ZC et al (2017) Preoperative telephone consultation does not decrease patient anxiety before Mohs micrographic surgery. J Am Acad Dermatol 76:519–526
Yang CL, Tan YH, Jiang XX et al (2012) Pre-operative education and counselling are associated with reduced anxiety symptoms following carotid endarterectomy: a randomized and open-label study. Eur J Cardiovasc Nurs 11:284–288
Mantziari S, Hubner M, Demartines N et al (2014) Impact of preoperative risk factors on morbidity after esophagectomy: is there room for improvement? World J Surg 38:2882–2890. https://doi.org/10.1007/s00268-014-2686-9
Lindstrom D, Sadr AO, Wladis A et al (2008) Effects of a perioperative smoking cessation intervention on postoperative complications: a randomized trial. Ann Surg 248:739–745
Thomsen T, Villebro N, Moller AM (2010) Interventions for preoperative smoking cessation. Cochrane Database Syst Rev CD002294
Yoshida N, Baba Y, Hiyoshi Y et al (2016) Duration of smoking cessation and postoperative morbidity after esophagectomy for esophageal cancer: how long should patients stop smoking before surgery? World J Surg 40:142–147. https://doi.org/10.1007/s00268-015-3236-9
Tonnesen H, Kehlet H (1999) Preoperative alcoholism and postoperative morbidity. Br J Surg 86:869–874
Tonnesen H, Rosenberg J, Nielsen HJ et al (1999) Effect of preoperative abstinence on poor postoperative outcome in alcohol misusers: randomised controlled trial. BMJ 318:1311–1316
Lee SM, Landry J, Jones PM et al (2013) The effectiveness of a perioperative smoking cessation program: a randomized clinical trial. Anesth Analg 117:605–613
Older P, Hall A (2005) Preoperative evaluation of cardiac risk. Br J Hosp Med 66:452–457
Ross RM (2003) ATS/ACCP statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 167:1451
Older P, Hall A, Hader R (1999) Cardiopulmonary exercise testing as a screening test for perioperative management of major surgery in the elderly. Chest 116:355–362
Moyes LH, McCaffer CJ, Carter RC et al (2013) Cardiopulmonary exercise testing as a predictor of complications in oesophagogastric cancer surgery. Ann R Coll Surg Engl 95:125–130
Forshaw MJ, Strauss DC, Davies AR et al (2008) Is cardiopulmonary exercise testing a useful test before esophagectomy? Ann Thorac Surg 85:294–299
Hennis PJ, Meale PM, Grocott MP (2011) Cardiopulmonary exercise testing for the evaluation of perioperative risk in non-cardiopulmonary surgery. Postgrad Med J 87:550–557
Sinclair R, Navidi M, Griffin SM et al (2016) The impact of neoadjuvant chemotherapy on cardiopulmonary physical fitness in gastro-oesophageal adenocarcinoma. Ann R Coll Surg Engl 98:396–400
Holte K, Nielsen KG, Madsen JL et al (2004) Physiologic effects of bowel preparation. Dis Colon Rectum 47:1397–1402
Guenaga KF, Matos D, Wille-Jorgensen P (2011) Mechanical bowel preparation for elective colorectal surgery. Cochrane Database Syst Rev CD001544
Cao F, Li J, Li F (2012) Mechanical bowel preparation for elective colorectal surgery: updated systematic review and meta-analysis. Int J Colorectal Dis 27:803–810
Brady M, Kinn S, Stuart P (2003) Preoperative fasting for adults to prevent perioperative complications. Cochrane Database Syst Rev CD004423
Ljungqvist O, Nygren J, Thorell A (2002) Modulation of post-operative insulin resistance by pre-operative carbohydrate loading. Proc Nutr Soc 61:329–336
Awad S, Varadhan KK, Ljungqvist O et al (2013) A meta-analysis of randomised controlled trials on preoperative oral carbohydrate treatment in elective surgery. Clin Nutr 32:34–44
Yilmaz N, Cekmen N, Bilgin F et al (2013) Preoperative carbohydrate nutrition reduces postoperative nausea and vomiting compared to preoperative fasting. J Res Med Sci 18:827–832
Smith MD, McCall J, Plank L et al. (2014) Preoperative carbohydrate treatment for enhancing recovery after elective surgery. Cochrane Database Syst Rev CD009161
Toms L, McQuay HJ, Derry S et al. (2008) Single dose oral paracetamol (acetaminophen) for postoperative pain in adults. Cochrane Database Syst Rev CD004602
Moiniche S, Kehlet H, Dahl JB (2002) A qualitative and quantitative systematic review of preemptive analgesia for postoperative pain relief: the role of timing of analgesia. Anesthesiology 96:725–741
Caumo W, Hidalgo MP, Schmidt AP et al (2002) Effect of pre-operative anxiolysis on postoperative pain response in patients undergoing total abdominal hysterectomy. Anaesthesia 57:740–746
Walker KJ, Smith AF (2009) Premedication for anxiety in adult day surgery. Cochrane Database Syst Rev CD002192
Gan TJ, Diemunsch P, Habib AS et al (2014) Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg 118:85–113
Apfel CC, Laara E, Koivuranta M et al (1999) A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology 91:693–700
Apfel CC, Korttila K, Abdalla M et al (2004) A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. N Engl J Med 350:2441–2451
Habib AS, El-Moalem HE, Gan TJ (2004) The efficacy of the 5-HT3 receptor antagonists combined with droperidol for PONV prophylaxis is similar to their combination with dexamethasone: a meta-analysis of randomized controlled trials. Can J Anaesth 51:311–319
Kazemi-Kjellberg F, Henzi I, Tramer MR (2001) Treatment of established postoperative nausea and vomiting: a quantitative systematic review. BMC Anesthesiol 1:2
Devereaux PJ, Yang H, Yusuf S et al (2008) Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet 371:1839–1847
Bouri S, Shun-Shin MJ, Cole GD et al (2014) Meta-analysis of secure randomised controlled trials of beta-blockade to prevent perioperative death in non-cardiac surgery. Heart 100:456–464
London MJ, Hur K, Schwartz GG et al (2013) Association of perioperative beta-blockade with mortality and cardiovascular morbidity following major noncardiac surgery. JAMA 309:1704–1713
Friedell ML, Van Way CW, Freyberg RW et al (2015) β-Blockade and operative mortality in noncardiac surgery: harmful or helpful? JAMA Surg 150:658–663
Wijeysundera DN, Duncan D, Nkonde-Price C et al (2014) Perioperative beta blockade in noncardiac surgery: a systematic review for the 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol 64:2406–2425
Blessberger H, Kammler J, Domanovits H et al. (2014) Perioperative beta-blockers for preventing surgery-related mortality and morbidity. Cochrane Database Syst Rev CD004476
Low DE, Kuppusamy MK, Alderson D et al (2017) Benchmarking complications associated with esophagectomy. Ann Surg. https://doi.org/10.1097/sla.0000000000002611
Tisdale JE, Jaynes H, Watson M et al (2017) Intravenous Amiodarone for prevention of atrial fibrillation following esophagectomy: a propensity score-matched analysis. J Am Coll Cardiol 69:545
Tisdale JE, Wroblewski HA, Wall DS et al (2010) A randomized, controlled study of amiodarone for prevention of atrial fibrillation after transthoracic esophagectomy. J Thorac Cardiovasc Surg 140:45–51
Mantziari S, Gronnier C, Pasquer A et al (2016) Incidence and risk factors related to symptomatic venous thromboembolic events after esophagectomy for cancer. Ann Thorac Surg 102:979–984
Kakkos SK, Caprini JA, Geroulakos G et al. (2008) Combined intermittent pneumatic leg compression and pharmacological prophylaxis for prevention of venous thromboembolism in high-risk patients. Cochrane Database Syst Rev CD005258
Morris RJ, Woodcock JP (2010) Intermittent pneumatic compression or graduated compression stockings for deep vein thrombosis prophylaxis? A systematic review of direct clinical comparisons. Ann Surg 251:393–396
Akl EA, Labedi N, Terrenato I et al. (2011) Low molecular weight heparin versus unfractionated heparin for perioperative thromboprophylaxis in patients with cancer. Cochrane Database Syst Rev CD009447
Song JQ, Xuan LZ, Wu W et al (2015) Low molecular weight heparin once versus twice for thromboprophylaxis following esophagectomy: a randomised, double-blind and placebo-controlled trial. J Thorac Dis 7:1158–1164
Rasmussen MS, Jorgensen LN, Wille-Jorgensen P (2009) Prolonged thromboprophylaxis with low molecular weight heparin for abdominal or pelvic surgery. Cochrane Database Syst Rev CD004318
Horlocker TT (2017) New updated anticoagulation publication. Unknown (in press)
Kurz A, Sessler DI, Lenhardt R (1996) Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med 334:1209–1215
Scott EM, Buckland R (2006) A systematic review of intraoperative warming to prevent postoperative complications. AORN J 83:1090–1113
Rajagopalan S, Mascha E, Na J et al (2008) The effects of mild perioperative hypothermia on blood loss and transfusion requirement. Anesthesiology 108:71–77
Yamasaki H, Tanaka K, Funai Y et al (2014) The impact of intraoperative hypothermia on early postoperative adverse events after radical esophagectomy for cancer: a retrospective cohort study. J Cardiothorac Vasc Anesth 28:943–947
Perez-Protto S, Sessler DI, Reynolds LF et al (2010) Circulating-water garment or the combination of a circulating-water mattress and forced-air cover to maintain core temperature during major upper-abdominal surgery. Br J Anaesth 105:466–470
Galvao CM, Liang Y, Clark AM (2010) Effectiveness of cutaneous warming systems on temperature control: meta-analysis. J Adv Nurs 66:1196–1206
Fujita T, Okada N, Kanamori J et al (2017) Thermogenesis induced by amino acid administration prevents intraoperative hypothermia and reduces postoperative infectious complications after thoracoscopic esophagectomy. Dis Esophagus 30:1–7
Hruska LA, Smith JM, Hendy MP et al (2005) Continuous insulin infusion reduces infectious complications in diabetics following coronary surgery. J Card Surg 20:403–407
Shah BR, Hux JE (2003) Quantifying the risk of infectious diseases for people with diabetes. Diabetes Care 26:510–513
Shilling AM, Raphael J (2008) Diabetes, hyperglycemia, and infections. Best Pract Res Clin Anaesthesiol 22:519–535
van den Berghe G, Wouters P, Weekers F et al (2001) Intensive insulin therapy in critically ill patients. N Engl J Med 345:1359–1367
van den Berghe G, Schetz M, Vlasselaers D et al (2009) Clinical review: intensive insulin therapy in critically ill patients: NICE-SUGAR or Leuven blood glucose target? J Clin Endocrinol Metab 94:3163–3170
Kehlet H (2008) Postoperative ileus: an update on preventive techniques. Nat Clin Pract Gastroenterol Hepatol 5:552–558
Traut U, Brugger L, Kunz R et al. (2008) Systemic prokinetic pharmacologic treatment for postoperative adynamic ileus following abdominal surgery in adults. Cochrane Database Syst Rev CD004930
Short V, Herbert G, Perry R et al. (2015) Chewing gum for postoperative recovery of gastrointestinal function. Cochrane Database Syst Rev CD006506
Bundgaard-Nielsen M, Holte K, Secher NH et al (2007) Monitoring of peri-operative fluid administration by individualized goal-directed therapy. Acta Anaesthesiol Scand 51:331–340
Jorgensen H, Wetterslev J, Moiniche S et al. (2000) Epidural local anaesthetics versus opioid-based analgesic regimens on postoperative gastrointestinal paralysis, PONV and pain after abdominal surgery. Cochrane Database Syst Rev CD001893
Bragg D, El-Sharkawy AM, Psaltis E et al (2015) Postoperative ileus: recent developments in pathophysiology and management. Clin Nutr 34:367–376
Tripepi-Bova KA, Sun Z, Mason D et al (2013) Early removal of urinary catheters in patients with thoracic epidural catheters. J Nurs Care Qual 28:340–344
Hu Y, Craig SJ, Rowlingson JC et al (2014) Early removal of urinary catheter after surgery requiring thoracic epidural: a prospective trial. J Cardiothorac Vasc Anesth 28:1302–1306
Zaouter C, Kaneva P, Carli F (2009) Less urinary tract infection by earlier removal of bladder catheter in surgical patients receiving thoracic epidural analgesia. Reg Anesth Pain Med 34:542–548
Allen MS, Blackmon SH, Nichols FC III et al (2016) Optimal timing of urinary catheter removal after thoracic operations: a randomized controlled study. Ann Thorac Surg 102:925–930
McPhail MJ, Abu-Hilal M, Johnson CD (2006) A meta-analysis comparing suprapubic and transurethral catheterization for bladder drainage after abdominal surgery. Br J Surg 93:1038–1044
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Allum reports other from Nestle, and personal fees from Lilly, outside the submitted work. Dr. Ljungqvist reports other from Encare AB, personal fees from Nutricia, NL, during the conduct of the study; other from Encare AB (Sweden), personal fees and other from Nutricia (NL), outside the submitted work. Dr. Neal reports other from American Society of Regional Anesthesia and Pain Medicine, other from Hospital for Special Surgery, New York, NY, personal fees from Virginia Mason Medical Center, personal fees from Occasional expert medical consultation, grants from Washington State Society of Anesthesiologists, and personal fees from Wolters Kluwer, outside the submitted work. Dr. Scott reports personal fees from Merck, personal fees from Deltex, and personal fees from Edwards, outside the submitted work. The authors Drs. Low, De Manzoni, Ferri, Immanuel, Kuppusamy, Law, Lindblad, Maynard, Pramesh, Smithers, and Addor have nothing to disclose.
Rights and permissions
About this article
Cite this article
Low, D.E., Allum, W., De Manzoni, G. et al. Guidelines for Perioperative Care in Esophagectomy: Enhanced Recovery After Surgery (ERAS®) Society Recommendations. World J Surg 43, 299–330 (2019). https://doi.org/10.1007/s00268-018-4786-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4786-4