Abstract
Background
Benchmarking operative volume and resources is necessary to understand current efforts addressing thoracic surgical need. Our objective was to examine the impact on thoracic surgery volume and patient access in Rwanda following a comprehensive capacity building program, the Human Resources for Health (HRH) Program, and thoracic simulation training.
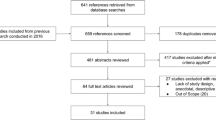
Methods
A retrospective cohort study was conducted of operating room registries between 2011 and 2016 at three Rwandan referral centers: University Teaching Hospital of Kigali, University Teaching Hospital of Butare, and King Faisal Hospital. A facility-based needs assessment of essential surgical and thoracic resources was performed concurrently using modified World Health Organization forms. Baseline patient characteristics at each site were compared using a Pearson Chi-squared test or Kruskal–Wallis test. Comparisons of operative volume were performed using paired parametric statistical methods.
Results
Of 14,130 observed general surgery procedures, 248 (1.76%) major thoracic cases were identified. The most common indications were infection (45.9%), anatomic abnormalities (34.4%), masses (13.7%), and trauma (6%). The proportion of thoracic cases did not increase during the HRH program (2.07 vs 1.78%, respectively, p = 0.22) or following thoracic simulation training (1.95 2013 vs 1.44% 2015; p = 0.15). Both university hospitals suffer from inadequate thoracic surgery supplies and essential anesthetic equipment. The private hospital performed the highest percentage of major thoracic procedures consistent with greater workforce and thoracic-specific material resources (0.89% CHUK, 0.67% CHUB, and 5.42% KFH; p < 0.01).
Conclusions and relevance
Lack of specialist providers and material resources limits thoracic surgical volume in Rwanda despite current interventions. A targeted approach addressing barriers described is necessary for sustainable progress in thoracic surgical care.


Similar content being viewed by others

References
Farmer PE, Kim JY (2008) Surgery and global health: a view from beyond the OR. World J Surg 32:533–536. https://doi.org/10.1007/s00268-008-9525-9
Meara JG, Leather AJM, Hagander L et al (2015) Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. The Lancet 386:569–624
Rose J, Weiser TG, Hider P et al (2015) Estimated need for surgery worldwide based on prevalence of diseases: a modelling strategy for the WHO Global Health Estimate. Lancet Glob Health 3:S13–S20
Debas HT, Donkor P, Gawande A et al (2015) Essential Surgery: disease control priorities, vol 1, 3rd edn. The World Bank, Washington
Weiser TG, Regenbogen SE, Thompson KD et al (2008) An estimation of the global volume of surgery: a modelling strategy based on available data. The Lancet 372:139–144
Weiser TG, Haynes AB, Molina G et al (2015) Estimate of the global volume of surgery in 2012: an assessment supporting improved health outcomes. The Lancet 385:S2–S11
Tollefson TT, Larrabee WF (2012) Global surgical initiatives to reduce the surgical burden of disease. JAMA 307:667–668
World Health Organization, Section II. Ten Essential Objectives for Safe Surgery: Review of the Evidence and Recommendations (2009) In: WHO guidelines for safe surgery 2009: safe surgery saves lives. Geneva, pp 10–96
Binagwaho A, Kyamanywa P, Farmer PE et al (2013) The human resources for health program in Rwanda—a new partnership. N Engl J Med 369:2054–2059
Cancedda C, Farmer PE, Kyamanywa P et al (2014) Enhancing formal educational and in-service training programs in rural Rwanda: a partnership among the public sector, a nongovernmental organization, and academia. Acad Med 89:1117–1124
Riviello R, Ozgediz D, Hsia RY et al (2010) Role of collaborative academic partnerships in surgical training, education, and provision. World J Surg 34:459–465. https://doi.org/10.1007/s00268-009-0360-4
Deckelbaum DL, Gosselin-Tardif A, Ntakiyiruta G et al (2014) An innovative paradigm for surgical education programs in resource-limited settings. Can J Surg 57:298–299
Livingston P, Bailey J, Ntakiyiruta G et al (2014) Development of a simulation and skills centre in East Africa: a Rwandan–Canadian partnership. Pan Afr Med J 17:315
World Health Organization (2017) Needs assessment and evaluation form for resource limited health care facility. http://apps.who.int/medicinedocs/documents/s15330e/s15330e.pdf. Accessed Feb 7, 2017
World Health Organization (2017) Guidelines for essential trauma care. http://apps.who.int/iris/bitstream/10665/42565/1/9241546409_eng.pdf. Accessed Sep 10, 2017
World Health Organization (2017) Guide to anesthetic infrastructure and supplies at various levels of health care facilities. http://www.who.intsurgerypublicationsGuideAnaestheticInfrastructureSuppliesrevAug.pdf. Accessed Mar 10, 2017
World Health Organization (2017) Surgical care at the district hospital. http://www.who.int/surgery/publications/en/SCDH.pdf. Accessed Oct 1, 2017
World Health Organization (2017) emergency relief items: compendium of basic specifications, vol 2. http://www.iapso.org/pdf/erc_vol2.pdf. Accessed Mar 3, 2017
Petroze RT, Groen RS, Niyonkuru F et al (2013) Estimating operative disease prevalence in a low-income country: results of a nationwide population survey in Rwanda. Surgery 153:457–464
Zogg CK, Kamara TB, Groen RS et al (2015) Prevalence of thoracic surgical care need in a developing country: results of a cluster-randomized, cross-sectional nationwide survey. Int J Surg 13:1–7
Biccard BM, Madiba TE, Kluyts H-L et al (2018) Perioperative patient outcomes in the African Surgical Outcomes Study: a 7-day prospective observational cohort study. Lancet 391:1589–1598
World Health Organization (2017) Integrated management for emergency and essential surgical care (IMEESC) toolkit. http://www.who.int/surgery/publications/imeesc/en/. Accessed Mar 5, 2017
Petroze RT, Nzayisenga A, Rusanganwa V et al (2012) Comprehensive national analysis of emergency and essential surgical capacity in Rwanda. BJS 99:436–443
Ramirez AG, Nuradin N, Byiringiro F et al (2018) Creation, implementation, and assessment of a general thoracic surgery simulation course in Rwanda. Ann Thorac Surg 105:1842–1849
Schipper PH, Diggs BS, Ungerleider RM, Welke KF (2009) The influence of surgeon specialty on outcomes in general thoracic surgery: a national sample 1996 to 2005. Ann Thorac Surg 88:1566–1573
Parker RK, Dawsey SM, Abnet CC et al (2010) Frequent occurrence of esophageal cancer in young people in western Kenya. Dis Esophagus 23:128–135
White RE, Abnet CC, Mungatana CK et al (2002) Oesophageal cancer: a common malignancy in young people of Bomet District, Kenya. The Lancet 360:462–463
Yendamuri S (2016) Thoracic surgery in India: challenges and opportunities. J Thorac Dis 8(Suppl 8):S596–S600
Linegar AG (2008) A model for the development of thoracic surgery in central South Africa. Ph.D. thesis, University of the Free State
Linegar A, Whittaker S, van Zyl G (2012) Academic hospital accreditation strengthens postgraduate training programmes: case study from Universitas Academic Hospital. S Afr Med J 102:146–148
Edwin F, Tettey M, Aniteye E et al (2011) The development of cardiac surgery in West Africa—the case of Ghana. Pan Afr Med J 9:15–27
Velebit V, Montessuit M, Bednarkiewicz M et al (2008) The development of cardiac surgery in an emerging country: a completed project. Tex Heart Inst J 25:301–306
Ghosh P (2005) Setting up an open heart surgical program in a developing country. Asian Cardiovasc Thorac Ann 13:299–301
European Respiratory Society (2017) European lung white book: thoracic surgery. https://www.erswhitebook.org/files/public/Chapters/32_surgery.pdf. Accessed Oct 10, 2017
Nyale GM, Anderson R, Patel AR et al (2016) A 10 years audit of cardiothoracic referrals from a pulmonology service in a developing country: impact of patient human immunodeficiency virus status. Ann Transl Med 4:2–132
Obaseki D, Adeniyi B, Kolawole T et al (2015) Gaps in capacity for respiratory care in developing countries. Nigeria as a case study. Ann Am Thorac Soc 12:591–598
Linegar A, Van Zyl G, Smit F et al (2010) Pleuro-pulmonary disease in central South Africa: a thoracicsurgical deficiency. SAMJ 100:510–512
Ekpe EE, Ette VF, Akpan A (2014) Pattern of cardiothoracic surgical diseases in a new cardiothoracic surgery unit in Nigeria. Nig J Med 23:77–82
Acknowledgements
We extend special appreciation to Drs. Christian Ngarambe and Emmanuel Kayibanda for their assistance in coordinating data collection on-site at CHUB and KFH, respectively. We also thank Drs. Marcel Durieux and Thomas Daniel for their supplementary feedback on essential surgical and anesthetic equipment for thoracic surgery. We are grateful to the Center for Global Health, the University of Virginia which provided financial support for travel expenses related to the work presented in this manuscript. The National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Numbers T32HL007849 supported research reported in this publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ramirez, A.G., Nuradin, N., Byiringiro, F. et al. General Thoracic Surgery in Rwanda: An Assessment of Surgical Volume and of Workforce and Material Resource Deficits. World J Surg 43, 36–43 (2019). https://doi.org/10.1007/s00268-018-4771-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4771-y