Abstract
Background
Robotic systems introduced new surgical and technical demands. Surgical flow disruptions are critical for maintaining operating room (OR) teamwork and patient safety. Specifically for robotic surgery, effects of intra-operative disruptive events for OR professionals’ workload, stress, and performance have not been investigated yet. This study aimed to identify flow disruptions and assess their association with mental workload and performance during robotic-assisted surgery.
Methods
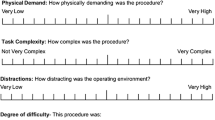
Structured expert-observations to identify different disruption types during 40 robotic-assisted radical prostatectomies were conducted. Additionally, 216 postoperative reports on mental workload (mental demands, situational stress, and distractions) and performance of all OR professionals were collected.
Results
On average 15.8 flow disruptions per hour were observed with the highest rate after abdominal insufflation and before console time. People entering the OR caused most flow disruptions. Disruptions due to equipment showed the highest severity of interruption. Workload significantly correlated with severity of disruptions due to coordination and communication.
Conclusions
Flow disruptions occur frequently and are associated with increased workload. Therefore, strategies are needed to manage disruptions to maintain OR teamwork and safety during robotic-assisted surgery.


Similar content being viewed by others
References
H-y Yu, Hevelone ND, Lipsitz SR et al (2012) Use, costs and comparative effectiveness of robotic assisted, laparoscopic and open urological surgery. J Urol 187:1392–1399
Randell R, Honey S, Alvarado N et al (2016) Embedding robotic surgery into routine practice and impacts on communication and decision making: a review of the experience of surgical teams. Cogn Technol Work 18:423–437
Sexton K, Johnson A, Gotsch A et al (2018) Anticipation, teamwork and cognitive load: chasing efficiency during robot-assisted surgery. BMJ Qual Saf 27:148–154
Catchpole K, Perkins C, Bresee C et al (2016) Safety, efficiency and learning curves in robotic surgery: a human factors analysis. Surg Endosc 30:3749–3761
Antoniadis S, Passauer-Baierl S, Baschnegger H et al (2014) Identification and interference of intraoperative distractions and interruptions in operating rooms. J Surg Res 188:21–29
Weigl M, Schneider A, Hoffmann F et al (2015) Work stress, burnout, and perceived quality of care: a cross-sectional study among hospital pediatricians. Eur J Pediatr 174:1237–1246
Mentis HM, Chellali A, Manser K et al (2016) A systematic review of the effect of distraction on surgeon performance: directions for operating room policy and surgical training. Surg Endosc 30:1713–1724
Wheelock A, Suliman A, Wharton R et al (2015) the impact of operating room distractions on stress, workload, and teamwork. Ann Surg 261:1079–1084
Persoon MC, Broos HJ, Witjes JA et al (2011) The effect of distractions in the operating room during endourological procedures. Surg Endosc 25:437–443
Parker SH, Laviana A, Wadhera R et al (2010) Development and evaluation of an observational tool for assessing surgical flow disruptions and their impact on surgical performance. World J Surg 34:353–361. https://doi.org/10.1007/s00268-009-0312-z
Jain M, Fry BT, Hess LW et al (2016) Barriers to efficiency in robotic surgery: the resident effect. J Surg Res 205:296–304
Allers JC, Hussein AA, Ahmad N et al (2016) Evaluation and impact of workflow interruptions during robot-assisted surgery. Urology 92:33–37
Catchpole K, Bisantz A, Hallbeck MS et al (2018) Human factors in robotic assisted surgery: lessons from studies ‘in the Wild’. Appl Ergon. https://doi.org/10.1016/j.apergo.2018.02.011
Arora S, Sevdalis N, Nestel D et al (2010) The impact of stress on surgical performance: a systematic review of the literature. Surgery 147:318–330
Blikkendaal MD, Driessen SR, Rodrigues SP et al (2016) Surgical flow disturbances in dedicated minimally invasive surgery suites: an observational study to assess its supposed superiority over conventional suites. Surg Endosc 31:228–298
Wilson MR, Poolton JM, Malhotra N et al (2011) Development and validation of a surgical workload measure: the surgery task load index (SURG-TLX). World J Surg 35:1961–1969. https://doi.org/10.1007/s00268-011-1141-4
Weigl M, Antoniadis S, Chiapponi C et al (2015) The impact of intra-operative interruptions on surgeons’ perceived workload: an observational study in elective general and orthopedic surgery. Surg Endosc 29:145–153
Weigl M, Stefan P, Abhari K et al (2016) Intra-operative disruptions, surgeon’s mental workload, and technical performance in a full-scale simulated procedure. Surg Endosc 30:559–566
Hart SG, Staveland LE (1988) Development of NASA-TLX (task load index): results of empirical and theoretical research. Adv Psychol 52:139–183
Wetzel CM, Kneebone RL, Woloshynowych M et al (2006) The effects of stress on surgical performance. Am J Surg 191:5–10
Yu D, Dural C, Morrow MM et al (2017) Intraoperative workload in robotic surgery assessed by wearable motion tracking sensors and questionnaires. Surg Endosc 31:877–886
Moore LJ, Wilson MR, McGrath JS et al (2015) Surgeons’ display reduced mental effort and workload while performing robotically assisted surgical tasks, when compared to conventional laparoscopy. Surg Endosc 29:2553–2560
Heemskerk J, Zandbergen HR, Keet SW et al (2014) Relax, it’s just laparoscopy! a prospective randomized trial on heart rate variability of the surgeon in robot-assisted versus conventional laparoscopic cholecystectomy. Dig Surg 31:225–232
Moore LJ, Wilson MR, Waine E et al (2015) Robotically assisted laparoscopy benefits surgical performance under stress. J Robot Surg 9:277–284
Suh IH, Chien JH, Mukherjee M et al (2010) The negative effect of distraction on performance of robot-assisted surgical skills in medical students and residents. Int J Med Robot + Comput Assist Surg: MRCAS 6:377–381
Suh IH, LaGrange CA, Oleynikov D et al (2016) Evaluating robotic surgical skills performance under distractive environment using objective and subjective measures. Surg Innov 23:78–89
Weigl M, Weber J, Hallett E et al (2018) Associations of intraoperative flow disruptions and operating room teamwork during robotic assisted radical prostatectomy. Urology 114:105–113
Gwet K (2002) Kappa statistic is not satisfactory for assessing the extent of agreement between raters. Stat Methods Inter-rater Reliab Assess 1:1–6
Hallgren KA (2012) Computing inter-rater reliability for observational data: an overview and tutorial. Tutor Quant Methods Psychol 8:23–34
Grawitch MJ, Granda SE, Barber LK (2008) Do prospective workday appraisals influence end-of-workday affect and self-monitored performance? J Occup Health Psychol 13:331–344
Dru CJ, Anger JT, Souders CP et al (2017) Surgical flow disruptions during robotic-assisted radical prostatectomy. Can J Urol 24:8814–8821
Catchpole KR, Hallett E, Curtis S et al (2018) Diagnosing barriers to safety and efficiency in robotic surgery. Ergonomics 61:26–39
Lee GI, Lee MR, Clanton T et al (2014) Comparative assessment of physical and cognitive ergonomics associated with robotic and traditional laparoscopic surgeries. Surg Endosc 28:456–465
Lee JR (2014) Anesthetic considerations for robotic surgery. Korean J Anesthesiol 66:3–11
Kakar P, Das J, Roy P et al (2011) Robotic invasion of operation theatre and associated anaesthetic issues: a review. Indian J Anaesth 55:18–25
Irvine M, Patil V (2009) Anaesthesia for robot-assisted laparoscopic surgery. Contin Educ Anaesth Crit Care Pain 9:125–129
Tiferes J, Hussein AA, Bisantz A et al (2018) Are gestures worth a thousand words?. Verbal and nonverbal communication during robot-assisted surgery, Appl Ergon
Widmer LW, Keller S, Tschan F et al (2018) More than talking about the weekend: content of case-irrelevant communication within the OR team. World J Surg. https://doi.org/10.1007/s00268-017-4442-4
Cavuoto LA, Hussein AA, Vasan V et al (2017) Improving teamwork: evaluating workload of surgical team during robot-assisted surgery. Urology 107:120–125
Weigl M, Muller A, Vincent C et al (2012) The association of workflow interruptions and hospital doctors’ workload: a prospective observational study. BMJ Qual Saf 21:399–407
Sevdalis N, Healey AN, Vincent CA (2007) Distracting communications in the operating theatre. J Eval Clin Pract 13:390–394
Gillespie BM, Chaboyer W, Fairweather N (2012) Interruptions and miscommunications in surgery: an observational study. AORN J 95:576–590
Hassan I, Weyers P, Maschuw K et al (2006) Negative stress-coping strategies among novices in surgery correlate with poor virtual laparoscopic performance. Br J Surg 93:1554–1559
Gillespie BM, Chaboyer W, Murray P (2010) Enhancing communication in surgery through team training interventions: a systematic literature review. AORN J 92:642–657
Acknowledgements
We thank all surgeons, nurses and anesthetists for their participation.
Funding
The study was supported by the Munich Centre for Health Sciences (MC-Health) and the Bavarian Research Alliance (BAYFOR).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Weber, J., Catchpole, K., Becker, A.J. et al. Effects of Flow Disruptions on Mental Workload and Surgical Performance in Robotic-Assisted Surgery. World J Surg 42, 3599–3607 (2018). https://doi.org/10.1007/s00268-018-4689-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4689-4