Abstract
Objective
To perform a meta-analysis to answer the question, whether early closure (EC) of defunctioning loop ileostomy may be beneficial for patient as compared with late closure (LC) without exceeding the risk of surgical-related morbidity.
Design
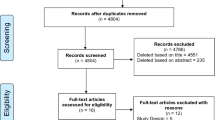
Medline and the Cochrane Trials Register were searched for trials published up to November 2016 comparing EC (defined as ≤14 days from the index operation in which the ileostomy was performed) versus LC for stoma closure after rectal surgery. Meta-analysis was performed using Review Manager 5.0. Inclusion criteria
Main outcome measures
Overall morbidity rate, anastomotic leakage rate, and wound infection rate within 90 days after elective surgery.
Results
Six studies were included and analyzed, yielding 570 patients (252 in EC group and 318 in LC). Meta-analysis showed no significant difference in the overall morbidity rate between the EC and LC groups (OR 0.63; 95% CI, 0.22–1.78; P = 0.38). Despite a significant higher wound infection rate of stoma site (OR 3.83; 95% CI 2.14–6.86; P < 0.00001), meta-analysis showed no significant difference in the anastomotic leakage rate between the EC and LC groups (OR 0.63; 95% CI 0.22–1.78; P = 0.38). Moreover, both stoma-related complications (OR 0.46; 95% CI 0.24–0.86; P = 0.02) and small bowel obstruction rates (OR 0.11; 95% CI 0.06–0.20; P < 0.00001) were significantly lower in the EC group than in the LC group, respectively.
Limitations
Heterogeneity of the studies
Conclusion
This meta-analysis suggests that EC of a defunctioning loop ileostomy is effective and safe in careful selected patients without increasing overall postoperative complications. This promising strategy should be proposed in patients in order to reduce stoma-related complications.







Similar content being viewed by others
References
Tan WS, Tang CL, Shi L et al (2009) Meta-analysis of defunctioning stomas in low anterior resection for rectal cancer. Br J Surg 96:462–472
Gu WI, Wu SW (2015) Meta-analysis of defunctioning stoma in low anterior resection with total mesorectal excision for rectal cancer: evidenced based on thirteen studies. World J Surg Oncol 13:9. https://doi.org/10.1186/s12957-014-0417-1
Hanna MH, Vinci A, Pigazzi A (2015) Diverting ileostomy in colorectal surgery: when is it necessary? Langenbecks Arch Surg 400:145–152
Marusch F, Koch A, Schmidt U et al (2002) Value of a protective stoma in low anterior resections for rectal cancer. Dis Colon Rectum 45:1164–1171
Dehni N, Schlegel RD, Cunningham C et al (1998) Influence of a defunctioning stoma on leakage rates after low colorectal anastomosis and colonic J pouch–anal anastomosis. Br J Surg 85:1114–1117
Karanjia ND, Corder AP, Holdworth PJ et al (1991) Risk of peritonitis and fatal septicaemia and the need to defunction the low anastomosis. Br J Surg 78:196–198
Peeters KCMJ, Tollenaar RAEM, Marijnen CAM et al (2005) Risk factors for anastomotic failure after total mesorectal excision of rectal cancer. Br J Surg 92:211–216
O’Toole GC, Hyland JM, Grant DC et al (1999) Defunctioning loop ileostomy: a prospective audit. J Am Coll Surg 188:6–9
Gessler B, Haglind E, Angenete E (2014) A temporary loop ileostomy affects renal function. Int J Colorectal Dis 29:1131–1135
Messaris E, Sehgal R, Deiling S et al (2012) Dehydration is the most common indication for readmission after diverting ileostomy creation. Dis Colon Rectum 55:175–180
Beck-Kaltenbach N, Voigt K, Rumstadt B (2011) Renal impairment caused by temporary loop ileostomy. Int J Colorectal Dis 26:623–626
Herrle F, Sandra-Petrescu F, Weiss C et al (2016) Quality of life and timing of stoma closure in patients with rectal cancer undergoing low anterior resection with diverting stoma: a multicenter longitudinal observational study. Dis Colon Rectum 59:281–290
Tulchinsky H, Shacham-Shmueli E, Klausner JM et al (2014) Should a loop ileostomy closure in rectal cancer patients be done during or after adjuvant therapy. J Surg Oncol 109:266–269
Velmahos GC, Degiannis E, Wells M et al (1995) Early closure of colostomies in trauma patients—a prospective randomized trial. Surgery 118:620–815
Bakx R, Busch ORC, van Geldere D et al (2003) Feasibility of early closure of loop ileostomies. Dis Colon Rectum 46:1680–1684
Jordi-Galais P, Turrin N, Tresallet C et al (2003) Fermeture précoce des stomies du grêle. Gastroenterol Clin Biol 27:697–699
Alves A, Panis Y, Lelong B et al (2008) Randomized clinical trial of early versus delayed temporary stoma closure after proctectomy. Br J Surg 95:693–698
Robertson JP, Puckett J, Vather R et al (2015) Early closure of temporary loop ileostomy: a systematic review. Ostomy Wound Manag 61:50–57
Robertson J, Linkhorn H, Vather R et al (2013) Cost analysis of early versus delayed loop ileostomy closure: a case-matched study. Dig Surg 32:166–172
Lasithiotakis K, Aghahoseini A, Alexander D (2016) Is early reversal of defunctioning ileostomy a shorter, easier and less expensive operation? World J Surg 40:1737–1740. https://doi.org/10.1007/s00268-016-3448-7
Danielsen AK, Park J, Jansen JE et al (2017) Early closure of a temporary ileostomy in patients with rectal cancer: a multicenter randomized controlled trial. Ann Surg 265:284–290
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Jadad A, Moore R, Carroll D et al (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–12
Worni M, Witschi A, Gloor B et al (2011) Early closure of ileostomy is associated with less postoperative nausea and vomiting. Dig Surg 28:417–423
Perez RO, Habr-Gama A, Seid VE et al (2006) Loop ileostomy morbidity: timing of closure matters. Dis Colon Rectum 49:1539–1545
Khan N, Bangash A, Hadi A et al (2010) Is early closure warranted in the management of temporary loop ileostomy? J Postgrad Med Inst 24:295–300
Tang CL, Seow-Choen F, Fook-Chong S et al (2003) Bioresorbable adhesion barrier facilitates early closure of the defunctioning ileostomy after rectal excision. Dis Colon Rectum 46:1200–1207
Memon S, Heriot AG, Atkin CE et al (2012) Facilitated early ileostomy closure after rectal cancer surgery: a case-matched study. Tech Coloproctol 16:285–290
Figueiredo MN, Mège D, Maggiori L et al (2015) When is the best time for temporary closure in laparoscopic sphincter-saving surgery for rectal cancer? A study of 259 consecutive patients. Tech Coloproctol 19:469–474
Chand M, Nash GF, Talbot RW (2008) Timely closure of loop ileostomy following anterior resection for rectal cancer. Eur J Cancer Care 17:611–615
Wong KS, Remzi FH, Gorgun E et al (2005) Loop ileostomy closure after restorative proctocolectomy: outcome in 1504 patients. Dis Colon Rectum 48:243–250
Menegaux F, Jordi-Galais P, Turrin N et al (2002) Closure of small bowel stomas on postoperative day 10. Eur J Surg 168:713–715
Gentilli S, Pizzorno C, Pessione S et al (2007) Early stoma closure in colorectal resections after endoscopic monitoring anastomosis. Clinical results. Chir Ital 59:507–512
Omundsen M, Hayes J, Collinson R et al (2012) Early ileostomy closure: is there a downside? ANZ J Surg 82:352–354
Krand O, Yalti T, Berber I et al (2008) Early vs delayed closure of temporary covering ileostomy: a prospective study. Hepatogastroenterology 55:142–145
Hirst NA, Tiernan JP, Millner PA et al (2014) Systematic review of methods to predict and detect anastomotic leakage in colorectal surgery. Colorectal Dis 16:95–109
Li LT, Hicks SC, Davilla JA et al (2014) Circular closure is associated with the lowest rate of surgical site infection following stoma reversal: a systematic review and multiple treatment meta-analysis. Colorectal Dis 16:406–416
Hsieh MC, Kuo LT, Chi CC et al (2015) Pursestring closure versus conventional primary closure following stoma reversal to reduce surgical site infection rate: a meta-analysis of randomized controlled trials. Dis Colon Rectum 58:808–815
Habbe N, Hannes S, Liese J et al (2014) The use of purse-string closure in loop ileostomy reversal leads to lower wound infection rates—a single high-volume centre experience. Int J Colorectal Dis 29:709–714
Milanchi S, Nasseri Y, Kidner T et al (2009) Wound infection after ileostomy closure can be eliminated by circumferential subcuticular wound approximation. Dis Colon Rectum 52:469–474
Chow A, Tilney HS, Paraskeva P et al (2009) The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Colorectal Dis 24:711–723
Shorthouse AJ, Bartram CI, Eyers AA et al (1982) The water soluble contrast enema after rectal anastomosis. Br J Surg 69:714–717
Gouya H, Oudjit A, Leconte M et al (2012) CT antegrade colonography to assess proctectomy and temporary diverting ileostomy complications before early ileostomy takedown in patients with low rectal endometriosis. AJR 198:98–105
Biagi JJ, Raphael MJ, Mackillop WJ et al (2011) Association between time to initiation of adjuvant chemotherapy and survival in colorectal cancer. A systematic review and meta-analysis. JAMA 305:2335–2342
Acknowledgments
We thank Hugh McGonigle, from Edanz Group (www.edanzediting.com/ac), for editing a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
Conception and design: BM, AA. Acquisition of data: BM, JL, AV. Analysis and interpretation of data: BM, AA. Drafting the article: BM, AA. Final approval: JL, AA.
Corresponding author
Rights and permissions
About this article
Cite this article
Menahem, B., Lubrano, J., Vallois, A. et al. Early Closure of Defunctioning Loop Ileostomy: Is It Beneficial for the Patient? A Meta-analysis. World J Surg 42, 3171–3178 (2018). https://doi.org/10.1007/s00268-018-4603-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4603-0