Abstract
Background
District hospitals in Africa could meet the essential surgical needs of rural populations. However, evidence on outcomes is needed to justify investment in this option, given that surgery at district hospitals in some African countries is usually undertaken by non-physician clinicians.
Methods
Baseline and 2–3-month follow-up measurements were undertaken on 98 patients who had undergone hernia repairs at four district and two central hospitals in Malawi, using a modified quality-of-life tool.
Results
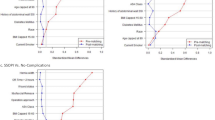
There was no significant difference in outcomes between district and central hospital cases, where a good outcome was defined as no more than one severe and three mild symptoms. Outcomes were marginally inferior at district hospitals (OR 0.79, 95% CI 0.63–1.0). However, in the 46 cases that underwent elective surgery at district hospitals, baseline scores for severe symptoms were worse (mean = 3.5) than in the 23 elective central hospital cases (mean = 2.5), p = 0.004. Also, the mean change (improvement) in symptom score was higher in district versus central hospital cases (3.9 vs. 2.3).
Conclusion
The study results support the case for investing in district hospital surgery in sub-Saharan Africa to increase access to essential surgical care for rural populations. This could free up specialists to undertake more complex and referred cases and reduce emergency presentations. It will require investments in training and resources for district hospitals and in supervision from higher levels.




Similar content being viewed by others
References
Meara JG, Greenberg SLM (2015) The Lancet Commission on Global Surgery Global surgery 2030: evidence and solutions for achieving health, welfare and economic development. Surgery 157:834–835. https://doi.org/10.1016/j.surg.2015.02.009
Ajayi OO, Adebamowo CA (1999) Surgery in Nigeria. Arch Surg 206–211. http://mbbsdost.com/Surgery-Nigeria-Archives-surgery-Chicago-Ill-1960-Ajayi-OO-Adebamowo-OO–1999-Feb/pubmed/12882203
Chokotho L, Jacobsen KH, Burgess D et al (2015) Trauma and orthopaedic capacity of 267 hospitals in east central and southern Africa. Lancet 385:S17. https://doi.org/10.1016/S0140-6736(15)60812-1
Grimes CE, Law RSL, Borgstein ES et al (2012) Systematic review of met and unmet need of surgical disease in rural sub-Saharan Africa. World J Surg 36:8–23. https://doi.org/10.1007/s00268-011-1330-1
Ozgediz D, Riviello R (2008) The “other” neglected diseases in global public health: surgical conditions in sub-Saharan Africa. PLoS Med 5:e121. https://doi.org/10.1371/journal.pmed.0050121
Mullan F, Frehywot S, Levy J et al (2007) Non-physician clinicians in 47 sub-Saharan African countries. Lancet (London, England) 370:2158–2163. https://doi.org/10.1016/S0140-6736(07)60785-5
Shawar YR, Shiffman J, Spiegel DA (2015) Generation of political priority for global surgery: a qualitative policy analysis. Lancet Glob Health 3:e487–e495. https://doi.org/10.1016/S2214-109X(15)00098-4
WHO|The world health report 2003-shaping the future. WHO Published Online First: 2013. http://www.who.int/whr/2003/en/. Accessed 19 June 2017
Groen R, Sesay S, Kushner A et al (2011) Three-stage repair of a giant inguinal hernia in Sierra Leone: a management technique for low-resource settings. J Surg Case Rep 2011:8. https://doi.org/10.1093/jscr/2011.12.8
Shillcutt SD, Clarke MG, Kingsnorth AN (2010) Cost-effectiveness of groin hernia surgery in the western region of Ghana. Arch Surg 145:954. https://doi.org/10.1001/archsurg.2010.208
Mabula JB, Chalya PL (2012) Surgical management of inguinal hernias at Bugando Medical Centre in northwestern Tanzania: our experiences in a resource-limited setting. BMC Res Notes 5:585. https://doi.org/10.1186/1756-0500-5-585
Mbah N (2017) Morbidity and mortality associated with inguinal hernia in Northwestern Nigeria. West Afr J Med 26:288–292. http://www.ncbi.nlm.nih.gov/pubmed/18705428. Accessed 19 June 2017
Uribe-Leitz T, Jaramillo J, Maurer L et al (2016) Variability in mortality following caesarean delivery, appendectomy, and groin hernia repair in low-income and middle-income countries: a systematic review and analysis of published data. Lancet Glob Health 4:e165–e174. https://doi.org/10.1016/S2214-109X(15)00320-4
Jenkins JT, O’Dwyer PJ (2008) Inguinal hernias. BMJ 336:269–272. https://doi.org/10.1136/bmj.39450.428275.AD
Deshpande P, Bl Sudeepthi, Rajan S et al (2011) Patient-reported outcomes: a new era in clinical research. Perspect Clin Res 2:137. https://doi.org/10.4103/2229-3485.86879
Bausewein C, Simon ST, Benalia H et al (2011) Implementing patient reported outcome measures (PROMs) in palliative care-users’ cry for help. Health Qual Life Outcomes 9:27. https://doi.org/10.1186/1477-7525-9-27
Hawn MT, Itani KM, Giobbie-Hurder A et al (2006) Patient-reported outcomes after inguinal herniorrhaphy. Surgery 140:198–205. https://doi.org/10.1016/j.surg.2006.02.003
Nelson EC, Eftimovska E, Lind C et al (2015) Patient reported outcome measures in practice. BMJ 350:g7818–g7818. https://doi.org/10.1136/bmj.g7818
Albers G, Echteld MA, de Vet HC et al (2010) Evaluation of quality-of-life measures for use in palliative care: a systematic review. Palliat Med 24:17–37. https://doi.org/10.1177/0269216309346593
Malawi country data. http://data.worldbank.org/country/malawi. Accessed 19 June 2017
Bailey N, Mandeville KL, Rhodes T et al (2012) Postgraduate career intentions of medical students and recent graduates in Malawi: a qualitative interview study. BMC Med Educ 12:87. https://doi.org/10.1186/1472-6920-12-87
Jiskoot P (2008) On-the-job training of clinical officers in Malawi. Malawi Med J 20:74–7. http://www.ncbi.nlm.nih.gov/pubmed/19537402. Accessed 19 June 2017
Henry JA, Frenkel E, Borgstein E et al (2015) Surgical and anaesthetic capacity of hospitals in Malawi: key insights. Health Policy Plan 30:985–994. https://doi.org/10.1093/heapol/czu102
Ahlsén AK, Spong E, Kafumba N et al (2015) Born too small: who survives in the public hospitals in Lilongwe, Malawi? Arch Dis Child Fetal Neonatal Ed 100:F150–F154. https://doi.org/10.1136/archdischild-2013-305877
O’Hare B, Phiri A, Lang H-J et al (2015) Task sharing within a managed clinical network to improve child health in Malawi. Hum Resour Health 13:60. https://doi.org/10.1186/s12960-015-0053-z
Global Surgery Map. http://www.cosecsa.org/global-surgery-map. Accessed 19 June 2017
Lavy C, Tindall A, Steinlechner C et al (2007) Surgery in Malawi: a national survey of activity in rural and urban hospitals. Ann R Coll Surg Engl 89:722–724. https://doi.org/10.1308/003588407X209329
Chu K, Rosseel P, Gielis P et al (2009) Surgical task shifting in sub-Saharan Africa. PLoS Med 6:e1000078. https://doi.org/10.1371/journal.pmed.1000078
van Amelsfoort JJC, van Leeuwen PAM, Jiskoot P et al (2010) Surgery in Malawi? The training of clinical officers. Trop Dr 40:74–76. https://doi.org/10.1258/td.2009.090068
Chilopora G, Pereira C, Kamwendo F et al (2007) Postoperative outcome of caesarean sections and other major emergency obstetric surgery by clinical officers and medical officers in Malawi. Hum Resour Health 5:17. https://doi.org/10.1186/1478-4491-5-17
Wilson A, Lissauer D, Thangaratinam S, et al (2011) A comparison of clinical officers with medical doctors on outcomes of caesarean section in the developing world: meta-analysis of controlled studies. BMJ 342. http://www.bmj.com/content/342/bmj.d2600. Accessed 19 June 2017
Wilhelm TJ, Thawe IK, Mwatibu B et al (2011) Efficacy of major general surgery performed by non-physician clinicians at a central hospital in Malawi. Trop Dr 41:71–75. https://doi.org/10.1258/td.2010.100272
COST Africa. www.costafrica.eu. Accessed 19 June 2017
Krpata DM, Schmotzer BJ, Flocke S et al (2012) Design and initial implementation of HerQLes: a hernia-related quality-of-life survey to assess abdominal wall function. J Am Coll Surg 215:635–642. https://doi.org/10.1016/j.jamcollsurg.2012.06.412
Literacy rates are on the rise but millions remain illiterate (2016). http://www.uis.unesco.org/Library/Documents/fs38-adult-youth-literacy-2016-en.pdf
Blum D, Selman LE, Agupio G et al (2014) Self-report measurement of pain and symptoms in palliative care patients: a comparison of verbal, visual and hand scoring methods in sub-Saharan Africa. Health Qual Life Outcomes 12:118. https://doi.org/10.1186/s12955-014-0118-z
Luboga S, Macfarlane SB, von Schreeb J et al (2009) Increasing access to surgical services in sub-Saharan Africa: priorities for national and international agencies recommended by the Bellagio Essential Surgery Group. PLoS Med 6:e1000200. https://doi.org/10.1371/journal.pmed.1000200
Samuel JC, Tyson AF, Mabedi C et al (2014) Development of a ratio of emergent to total hernia repairs as a surgical capacity metric. Int J Surg 12:906–911. https://doi.org/10.1016/j.ijsu.2014.07.019
Chan KY, Rohaizak M, Sukumar N et al (2004) Inguinal hernia repair by surgical trainees at a Malaysian teaching hospital. Asian J Surg 27:306–312. https://doi.org/10.1016/S1015-9584(09)60057-9
Gessessew A, Barnabas GA, Prata N et al (2011) Task shifting and sharing in Tigray, Ethiopia, to achieve comprehensive emergency obstetric care. Int J Gynecol Obstet 113:28–31. https://doi.org/10.1016/j.ijgo.2010.10.023
Eyal N, Cancedda C, Kyamanywa P et al (2015) Non-physician clinicians in sub-Saharan Africa and the evolving role of physicians. Int J Heal policy Manag 5:149–153. https://doi.org/10.15171/ijhpm.2015.215
Gajewski J, Mweemba C, Cheelo M, McCauley T, Kachimba J, Borgstein E, Bijlmakers L, Brugha R (2017) Non-physician clinicians in rural Africa: lessons from the Medical Licentiate programme in Zambia. Hum Resour Health 15(1):53
Pereira C, Cumbi A, Malalane R et al (2007) Meeting the need for emergency obstetric care in Mozambique: work performance and histories of medical doctors and assistant medical officers trained for surgery. BJOG Int J Obstet Gynaecol 114:1530–1533. https://doi.org/10.1111/j.1471-0528.2007.01489.x
Mkandawire N, Ngulube C, Lavy C (2008) Orthopaedic clinical officer program in Malawi: a model for providing orthopaedic care. Clin Orthop Relat Res 466:2385–2391. https://doi.org/10.1007/s11999-008-0366-5
Gosselin RA, Thind A, Bellardinelli A (2006) Cost/DALY averted in a small hospital in Sierra Leone: what is the relative contribution of different services? World J Surg 30:505–511. https://doi.org/10.1007/s00268-005-0609-5
Hounton SH, Newlands D, Meda N et al (2009) A cost-effectiveness study of caesarean-section deliveries by clinical officers, general practitioners and obstetricians in Burkina Faso. Hum Resour Health 7:34. https://doi.org/10.1186/1478-4491-7-34
Kolstad PR, Burnham G, Kalter HD, et al (1998) Potential implications of the integrated management of childhood illness (IMCI) for hospital referral and pharmaceutical usage in western Uganda. Trop Med Int Health 3:691–9. http://www.ncbi.nlm.nih.gov/pubmed/9754663. Accessed 19 June 2017
Grumbach K, Coffman J (1998) Physicians and nonphysician clinicians: complements or competitors? JAMA 280:825–6. http://www.ncbi.nlm.nih.gov/pubmed/9729998. Accessed 19 June 2017
Group W (1994) Development of the WHOQOL: rationale and current status. Int J Ment Health 23:24–56. https://doi.org/10.2307/41344692
Meltzer ME, Congdon N, Kymes SM et al (2017) Cost and expected visual effect of interventions to improve follow-up after cataract surgery. JAMA Ophthalmol 135:85. https://doi.org/10.1001/jamaophthalmol.2016.4735
Acknowledgements
Funding was provided by Seventh Framework Programme (Ref. FP7-AFRICA-2010, Grant Agreement No. 266417).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Gajewski, J., Conroy, R., Bijlmakers, L. et al. Quality of Surgery in Malawi: Comparison of Patient-Reported Outcomes After Hernia Surgery Between District and Central Hospitals. World J Surg 42, 1610–1616 (2018). https://doi.org/10.1007/s00268-017-4385-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4385-9